Brugada syndrome was first reported by the Brugada brothers in 1992. Reference Brugada and Brugada1 This syndrome shows a right bundle branch block pattern and ST-segment elevation in leads V1–V3 on an electrocardiogram and is associated with life-threatening ventricular arrhythmias, syncope, and sudden cardiac death.
A Brugada pattern may be observed transiently in patients during provoking factors such as fever. This report details the clinical features of a woman, who developed fever 1 day after device closure of her atrial septal defect accompanied by characteristic ST-segment elevation in the right precordial leads.
A case report
A 25-year-old woman was referred to our hospital to treat atrial septal defect. Detection of a heart murmur at 3 months of age led to the diagnosis of atrial septal defect. An incomplete right bundle branch block was documented in her electrocardiogram at 13 years of age. There was no family history of sudden cardiac death in first- or second-degree relatives.
Her height was 159.4 cm, weight was 61.2 kg, and body mass index was 24.1 kg/m2. Abnormal vital signs were not found, although a systolic murmur with Levine grade 1/6 was found at the fourth left sternal border. A chest X-ray showed a cardiothoracic ratio of 0.46 and a slightly enhanced pulmonary vascular shadow. An electrocardiogram showed normal sinus rhythm, a heart rate of 58 bpm, first-degree atrioventricular block, and incomplete right bundle branch block. A crochetage pattern was observed in leads III and aVf. An inverted T-wave was observed in leads V1 and V2, but ST-segment elevation was not observed (Fig 1a). Echocardiography showed ostium secundum atrial septal defect (11 mm) and dilatation of the right atrium and the right ventricle (Fig 2). Cardiac catheterisation showed a mean pulmonary artery pressure of 15 mmHg, pulmonary blood flow/systemic blood flow ratio of 1.53, and pulmonary vascular resistance of 0.8 Wood units. Percutaneous atrial septal defect closure was performed, and the atrial septal defect was closed using a 12-mm Amplatzer® Septal Occluder (St. Jude Medical Co., Saint Paul, MN, United States of America).
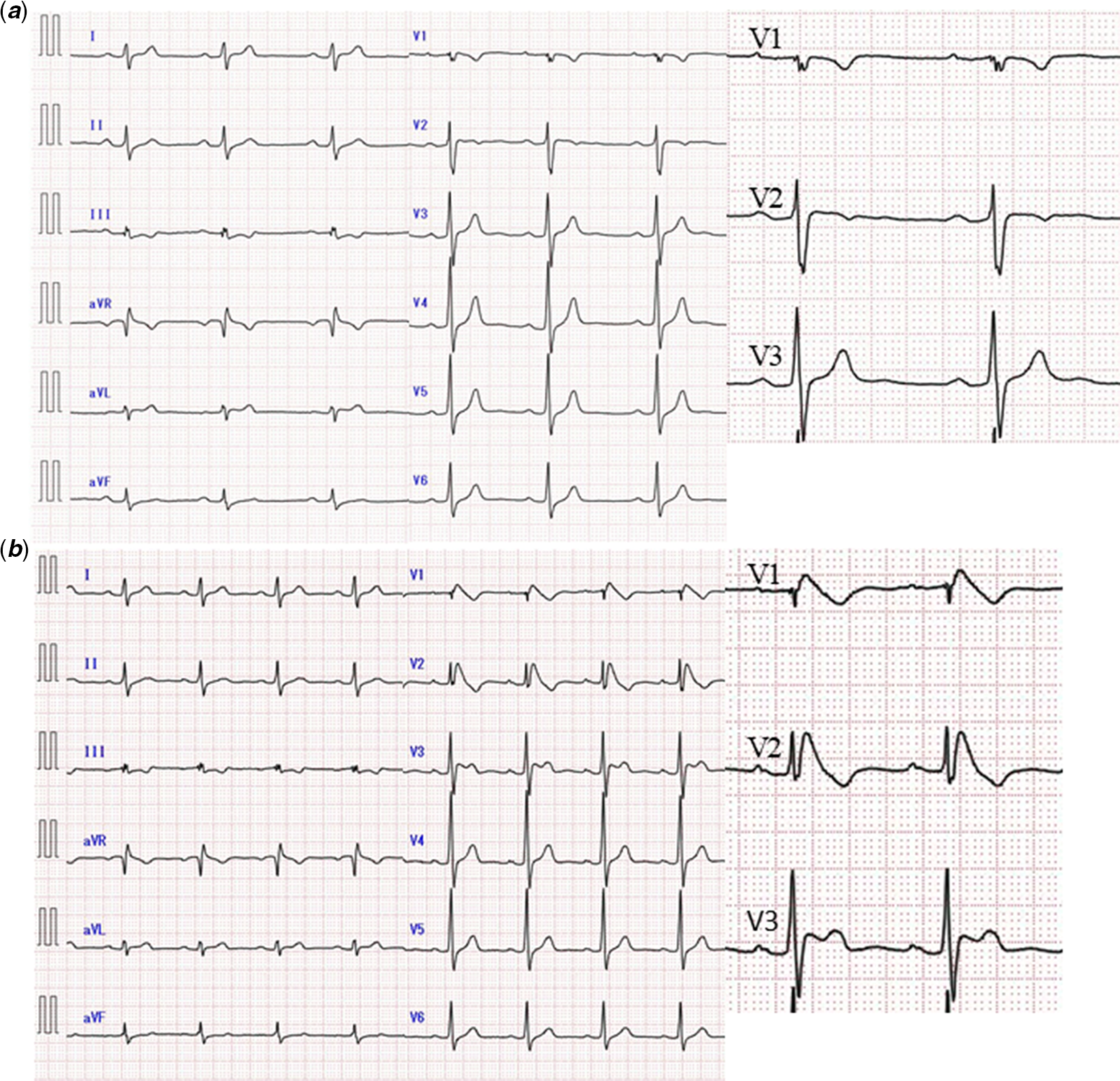
Figure 1. ( a ) Electrocardiogram without fever. First-degree atrioventricular block, incomplete right bundle branch block, and crochetage pattern were observed. Inverted T waves were observed in leads V1 and V2, but ST-segment elevation was not observed. ( b ) Electrocardiogram with slight fever (post-operative day 1). ST-segment elevation ≥ 2 mm in V1–V3, which was a finding of type 1 (coved type) Brugada pattern.
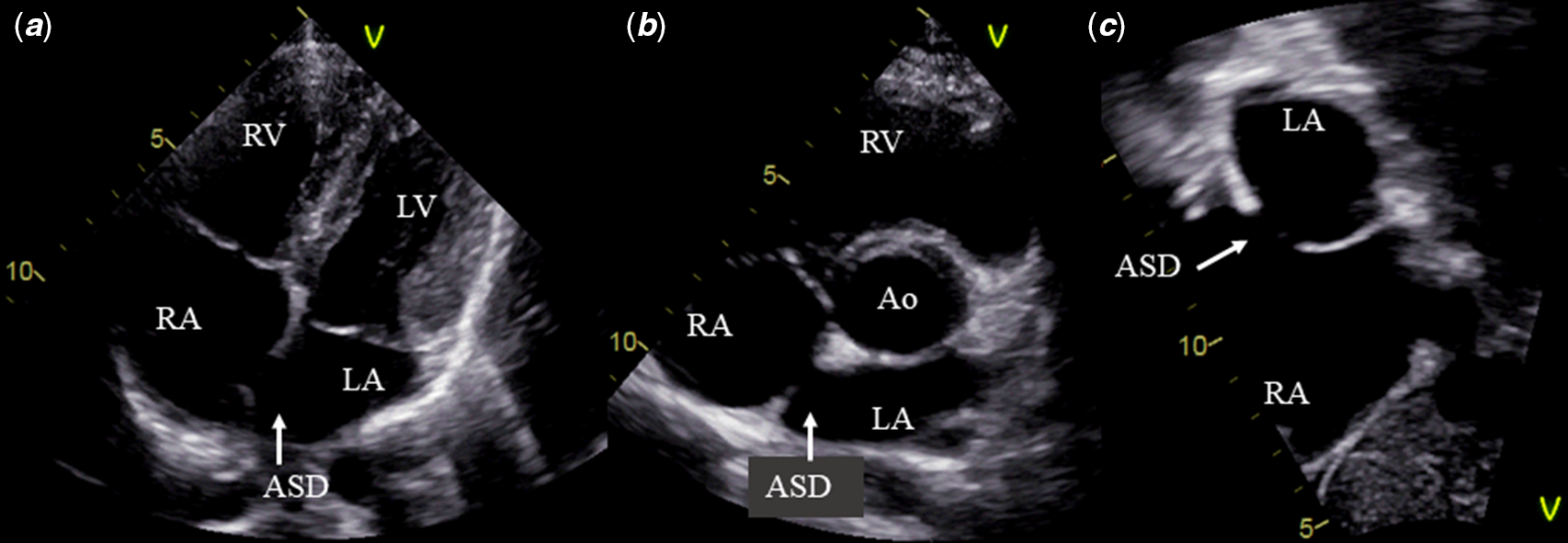
Figure 2. Echocardiography before catheterisation. ( a ) Four-chamber view, ( b ) short axis view, and ( c ) subcostal sagittal view. An echocardiography showed ostium secundum atrial septal defect (11 mm) and mild dilatation of the right atrium and ventricular. ASD = atrial septal defect; LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle.
One day after the operation, the patient had a slight fever of 37.8 degrees. A standard electrocardiogram showed ST-segment elevation ≥2 mm in leads V1–V3, which was a finding of a type 1 (coved type) Brugada pattern (Fig 1b). A blood test on the same day was negative for troponin T, and there were no electrolyte abnormalities (Na: 137.6 mmol/L, K: 4.0 mmol/L, Ca: 8.8 mmol/L). One month after the operation, although a standard electrocardiogram did not show ST-segment elevation, an electrocardiogram of the right precordial leads (V1–V3), which were placed in a superior position (third intercostal space), showed ST-segment elevation and a type 1 Brugada pattern again. Additionally, a signal-averaged electrocardiogram was positive for late potential. However, an electrocardiogram during treadmill exercise showed neither ventricular fibrillation nor ST elevation during recovery. A genetic test did not show SCN5A gene mutations.
Discussion
Brugada syndrome shows elevation in the J-wave amplitude and characteristic ST-segment elevation among the right precordial leads on electrocardiogram, causing ventricular fibrillation and sudden death. Reference Priori, Wilde and Horie2 The proportion of women with Brugada syndrome is relatively small, with a reported rate of 20–30% in Europe and the United States of America, and approximately 5% in Japan. Reference Kamakura, Ohe and Nakazawa3 The clinical presentation of Brugada syndrome in women (event rate of 0.7%/year) is less common than that in men (event rate of 1.9%/year). However, there have been rare reports of intractable arrhythmia in women, indicating their occasional vulnerability. Reference Sieira, Conte and Ciconte4
There have been few reports of Brugada syndrome with CHD. Reference Silvia, Martins and Cavaco5,Reference Sivakumar, Pavithran, Louis and Satish6 ST-segment elevation, which is characteristic of a Brugada pattern, has diurnal fluctuations and it may be difficult to distinguish from an incomplete right bundle branch block. Reference Chevallier, Forclaz and Tenkorang7 In our case, there was no elevation in the J-wave amplitude or ST-segment elevation in the standard electrocardiogram. Additionally, there was not diagnostic suspicion of the Brugada syndrome, and we thought that this electrocardiogram pattern before catheterisation was related to atrial septal defect. The standard electrocardiogram at the time of the patient’s fever showed right bundle branch block pattern and ST-segment elevation ≥2 mm, and we determined that this was a type 1 Brugada pattern. ST-segment elevation was normalised after a reduction in the fever. However, ST-segment elevation was observed in an electrocardiogram with the right precordial leads placed one space above the routine lead position, even when she was afebrile.
The Brugada pattern does not always appear in an electrocardiogram. In an electrocardiogram, the right precordial leads should be placed in the superior position if patients have a right bundle branch block pattern and clinical symptoms, such as a history of syncope or a family history of sudden cardiac death. An electrocardiogram with the right precordial leads placed in the superior position was able to show the Brugada pattern in our patient who also had atrial septal defect.
Our patient was diagnosed with Brugada syndrome Reference Antzelevitch, Yan and Ackerman8 by accidental induction of a Brugada pattern owing to postoperative fever. Fever increases the risk of fatal arrhythmia in young patients with Brugada syndrome. Reference Michowitz, Milman and Sarquella-Brugada9
In this case, we considered that the patient was unlikely to develop ventricular arrhythmia because she was asymptomatic, a woman, and she did not have any mutation of SCN5A or a family history of sudden cardiac death. Therefore, we decided not to insert an implantable cardioverter defibrillator. However, the patient needed to pay attention to fever, electrolyte abnormalities, and excessive alcohol intake.
Conclusion
We experienced a young woman with Brugada syndrome and atrial septal defect. An electrocardiogram with the right precordial leads placed in the superior position was effective in showing the Brugada pattern, even when associated with atrial septal defect.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The manuscript is an original work of all authors. All authors made significant contribution and have read and approved the final version of the manuscript.





