Since the onset of the coronavirus disease 2019 (COVID-19) pandemic, there has been substantial evidence that cardiac injury is common in patients infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Early reports focused on highlighting the alarming rates of acute myocardial injury in hospitalised adult patients with severe disease. Reference Smilowitz, Jethani and Chen1–Reference Driggin, Madhavan and Bikdeli5
More recent studies, however, have demonstrated that a portion of adults with prior COVID-19 continue to have evidence of myocarditis, even after recovery from their illness and even in adults who were never hospitalised. Reference Puntmann, Carerj and Wieters6–Reference Rajpal, Tong and Borchers8 Several studies have evaluated younger adults, including collegiate and professional athletes, and have identified myocarditis in a small subset of these patients as well, even in mild or asymptomatic cases. Reference Rajpal, Tong and Borchers8–Reference Martinez, Tucker and Bloom13
There is currently a paucity of published data regarding the cardiac manifestations in children with acute COVID-19. Most of the current paediatric literature focuses on the multisystem inflammatory syndrome in children, since there is frequently associated ventricular dysfunction, and less commonly, coronary artery aneurysms and arrhythmias. Reference Valverde, Singh and Sanchez-de-Toledo14–Reference Godfred-Cato, Bryant and Leung15 Multisystem inflammatory syndrome in children, though, is felt to be a distinct entity due to a delayed immune response to SARS-CoV-2 rather than due to acute viral injury. Reference Diorio, Henrickson and Vella16–Reference Rostad, Chahroudi and Mantus18
Since myocarditis is a leading cause of sudden cardiac death in young competitive athletes, multiple guidelines have been developed to risk stratify patients prior to their return to competitive sports after COVID-19. Reference Phelan, Kim and Chung19–Reference Drezner, Heinz and Asif25 There are only a few published guidelines specifically for children, including statements from the American College of Cardiology and the American Academy of Pediatrics. Reference Kim, Levine and Phelan21,Reference Dean, Jackson and Paridon26,27 Most of these guidelines include recommendations for screening electrocardiograms in a subset of patients, followed by cardiology consultation for sports clearance among patients with abnormal electrocardiogram findings. There is no clear evidence, however, that screening electrocardiograms are helpful in the evaluation of myocarditis after COVID-19, especially in paediatrics. Reference Erickson, Poterucha and Gende28
We therefore sought to assess the utility of screening electrocardiograms after COVID-19 in children by analysing the diagnostic and clinical evaluations of those patients who were referred to outpatient paediatric cardiology for abnormal screening electrocardiograms.
Materials and methods
Data source
Identification of subjects and patient data were obtained through a review of electronic medical records.
Study population
This study was a retrospective chart review of children at a single institution, Children’s Hospital of Philadelphia (CHOP), with a history of SARS-CoV-2 infection who were referred by their primary care providers for an outpatient cardiology consultation due to concerning findings on a screening electrocardiogram. Subjects were identified by querying the electronic medical record for patients whose primary care providers had ordered an electrocardiogram after 1 March, 2020 with an associated diagnosis containing the term “COVID,” who then had an outpatient cardiology office evaluation either in person or via telemedicine that was completed prior to 25 March, 2021. The query was limited to electrocardiograms ordered by primary care providers within our large outpatient hospital network and limited to patients in whom both the ordered electrocardiogram and the cardiology office visit were completed, filtering out any cancelled or unattended visits. Patients with a diagnosis of multisystem inflammatory syndrome in children were excluded. Additionally, patients who had COVID-19 and were referred for cardiology evaluation due to cardiac symptoms alone, yet with a normal screening electrocardiogram, were similarly excluded.
Study measures
The primary exposure for the study was the identification by a patient’s primary care provider of a concerning finding on a post-COVID-19 screening electrocardiogram, which prompted an outpatient cardiology evaluation. All electrocardiograms performed at our institution are officially interpreted by a paediatric cardiologist. The outcomes of interest were the subsequent workup and testing the patients underwent as part of their cardiology evaluation as well as the final cardiology diagnosis. Each patient was evaluated by a paediatric cardiologist who determined the final diagnosis based on his/her clinical evaluation and any associated diagnostic testing that was ordered on the basis of the treating cardiologist’s clinical concerns. The spectrum of cardiac testing included additional electrocardiograms, echocardiography, Holter monitoring, cardiac MRI, and exercise stress tests. No test was ordered for research purposes. Data about a range of potentially influential covariates were also collected, which included both demographic factors (i.e. gender, race, ethnicity) and clinical factors, such as the patients’ past medical history, age at SARS-CoV-2 diagnosis, severity of illness, associated symptoms, and body mass index. For normally distributed data, mean and standard deviation were reported, and for non-normally distributed data, median and interquartile range were reported. Illness severity was graded according to the American Academy of Pediatrics classification in their published guidance for return to sports following COVID-19. 27 The final diagnosis was assigned by the treating cardiologist and independently reviewed by the authors (M.E. and A.G.) of this manuscript. Patient clinical and procedural data were collected via the web-based application Research Electronic Data Capture (REDCap) hosted at our institution. The study protocol was approved by the institutional review board with exempt determination. Lastly, we provide an overview of the current paediatric cardiology guidelines after COVID-19, important in the context of the current study methodology, with the proposed guidelines from our academic institution.
Results
The patient cohort consisted of 46 patients, of which 31 (67.4%) were male and 38 (86.4%) identified as Caucasian (Table 1). The mean age at the time of positive SARS-CoV-2 PCR testing was 15.6 years with a range of 12 to 18 years. Most patients (41, 89.1%) had mild symptoms, 4 (8.7%) were asymptomatic, and 1 (2.2%) had moderate symptoms, with none of the study patients experiencing severe disease or requiring hospitalisation. The most commonly reported symptoms were headache (47.6%), fever (40.5%), and fatigue (35.7%). With respect to cardiorespiratory symptoms, there were 4 (9.5%) reports of chest pain/tightness, 1 (2.4%) of shortness of breath, 1 (2.4%) of lightheadedness, and no instances of palpitations or syncope.
Table 1. Patient characteristics

Data presented as count (% of total), mean ± SD, or median (interquartile range). “Other” category for past medical history includes small anomalous optic pit of the right optic nerve, depression, Crohn’s disease, patellofemoral pain syndrome, type 1 diabetes mellitus, Sever’s apophysitis, fragile X syndrome carrier, hypertriglyceridemia, jejunal atresia, minocycline-induced hepatitis and pancreatitis, mild scoliosis, and eczema. ADHD, attention-deficit hyperactivity disorder; HEENT, head, eyes, ears, nose, and throat; GI, gastrointestinal; BMI, body mass index.
In the majority of patients, the date of a prior positive SARS-CoV-2 PCR was used to confirm evidence of a prior infection. There were, however, three instances of PCR results that were deemed false-negatives by the treating clinicians due to highly characteristic symptoms of COVID-19 and multiple affected family members with positive tests. There were also two patients who were presumed to have COVID-19 by their physicians without formal PCR testing, again due to highly characteristic symptoms. All five of these patients were included in the patient cohort given the high likelihood of clinical infection. The median length of time from the positive SARS-CoV-2 test to the electrocardiogram was 22 days (IQR 14–39), and the median length of time from the positive test to the date of the cardiology visit was 36 days (25–53). There was a range of electrocardiogram findings that prompted cardiology referral (Table 2), most commonly sinus bradycardia in 10 (21.7%), incomplete right bundle branch block or right ventricular conduction delay in 8 (17.4%), non-specific ST elevation in 7 (15.2%), and right atrial enlargement in 5 (13.0%).
Table 2. Initial ECG findings prompting cardiology referral

ECG = electrocardiogram; IRBBB = incomplete right bundle branch block; RVCD = right ventricular conduction delay; LVH = left ventricular hypertrophy; NSIVCD = non-specific intraventricular conduction delay; PVCs = pre-mature ventricular contractions; RBBB = right bundle branch block; RVH = right ventricular hypertrophy.
Most patients (72%) received another electrocardiogram during the subsequent cardiology outpatient visit, and just over half of the patients (59%) received an echocardiogram, with fewer receiving additional testing (Fig 1). Table S3 provides a summary of the pertinent findings on subsequent testing, number of outpatient visits completed, and final outcomes for those patients with concerning electrocardiogram findings who were referred to cardiology. Most patients (38, 82.6%) were determined to have no cardiac disease, with the electrocardiogram findings that prompted referral either having normalised on repeat assessment, or more often, being characterised as normal variants. Pertinent final cardiac diagnoses included individual cases of gene-positive congenital long QT syndrome, persistently borderline prolonged QTc interval, cor triatriatum sinister, prominent left ventricular trabeculations not meeting criteria for left ventricular non-compaction cardiomyopathy, mild ascending aortic dilation, bicuspid aortic valve, pre-mature ventricular contractions, and pre-mature atrial contractions. There were no patients with evidence of inflammatory heart disease (i.e. myocarditis or pericarditis) or ventricular dysfunction suggestive of acute cardiac injury.

Figure 1. Additional cardiac testing performed following initial ECG.
Key: ECG, electrocardiogram; Echo, echocardiogram; CMR, cardiac MRI; EST, exercise stress test.
Discussion
Current paediatric guidelines for cardiac evaluation after COVID-19 prior to returning to sports are extrapolated from adult data and typically involve screening electrocardiograms. To the authors’ knowledge, this current study is the first to review the utility of electrocardiograms in the assessment of children after COVID-19. A recent study of 170 collegiate athletes evaluated whether routine screening electrocardiograms were beneficial; six patients (3.5%) had an abnormal electrocardiogram that warranted cardiology evaluation, and only one electrocardiogram identified viral pericarditis, with no patients having myocarditis. Reference Erickson, Poterucha and Gende28
In our study, the most common potentially abnormal electrocardiogram findings – sinus bradycardia, incomplete right bundle branch block, right ventricular conduction delay, non-specific ST elevation, and right atrial enlargement – have all been well recognised as normal variants in asymptomatic adolescent athletes, Reference Sharma, Drezner and Baggish29 which casts strong doubt that any of these findings were COVID-related. Among the patients referred to cardiology in this patient cohort, the majority (82.6%) were deemed to have no cardiac disease, and several were diagnosed with incidental findings unrelated to COVID-19. The electrocardiogram findings of pre-mature atrial contractions and pre-mature ventricular contractions that might potentially be COVID-related are also highly common incidental findings in general. Three patients were referred for a borderline QTc interval, of which two electrocardiograms were normal at the outpatient visit and one remained borderline. One additional patient had a persistently prolonged QTc leading to an incidental diagnosis of gene-positive congenital long QT syndrome. Although prolonged QTc intervals have been associated with COVID-19 in adults, Reference Akhtar, Gallagher and Yap30 genetic long QT syndrome is unrelated to COVID-19.
Most patients received a repeat electrocardiogram at their cardiology visit, and about half of the patients received an echocardiogram, with fewer undergoing additional testing consisting of Holter monitoring, cardiac MRI, and exercise stress test. Although these additional diagnostic modalities did reveal pertinent isolated cardiac diagnoses in several instances, there were importantly no patients with any evidence of myocarditis or ventricular dysfunction across this broad array of testing. While the presence of cardiac disease cannot be conclusively ruled out without additional testing often used in research studies, such as adjunct echocardiograms or cardiac MRIs, each patient was evaluated by a paediatric cardiologist at a large academic centre who determined the final diagnosis based on a comprehensive clinical evaluation with supplemental diagnostic testing as indicated.
The importance of identifying potential myocarditis stems from myocarditis being one of the most common causes of sudden cardiac death in competitive adolescent athletes, Reference Maron, Thompson and Ackerman31 accounting for approximately 5–10% of cases. Given the potential risk of myocarditis after COVID-19, in May 2020, the American College of Cardiology Sports and Exercise Section generated recommendations to promote safe return-to-play for competitive adult athletes following COVID-19, which included 2 weeks of convalescence without exercise after symptom resolution, followed by “triad testing” consisting of a troponin, electrocardiogram, and echocardiogram. Reference Phelan, Kim and Chung19 These guidelines have been refined in light of emerging data on the rarity of myocardial involvement, especially in asymptomatic patients or those with only mild disease, to recommend cardiac diagnostic testing only in higher risk groups, such as those who had moderate or severe COVID-19 symptoms. Reference Kim, Levine and Phelan21
A statement from the American College of Cardiology in July 2020 highlighted an important distinction in children with the introduction of an age cut-off for screening at 12 years old. Reference Dean, Jackson and Paridon26 For younger children, the level of intensity of a sporting event may not be that much more strenuous than normal recreational activities and regular play. For older children and adolescents, who may be naturally pushed by their coaches and teammates beyond their normal comfort level in order to maximise their athletic performance, the risk of a sudden cardiac event may increase if they happen to have underlying myocarditis. Therefore, the authors recommended a screening electrocardiogram prior to return-to-play only in those older than 12 years who experienced moderate COVID-19 symptoms and participated in competitive sports. The American Academy of Pediatrics’ guidelines have evolved over the past year and similarly recommend a screening electrocardiogram for moderately symptomatic patients (≥4 days of fever, ≥1 week of myalgia, chills, or lethargy, or non-ICU admission), although without a specific age cut-off and regardless of activity level. 27
Our institution has created additional paediatric guidelines, led by several authors of this current study, based on the latest literature, published guidelines, and local experience and consensus among divisions, including this current data. The initial guidelines were intentionally conservative and recommended a screening electrocardiogram prior to return-to-play in patients ≥12 years old who had either mild or moderate symptoms and were involved in competitive sports, along with an outpatient cardiology evaluation regardless of age or activity level for those with severe symptoms, with the possibility of up to 3–6 months of exercise restriction depending on clinical severity. These guidelines were recently updated in April 2021 to limit the recommendation for a screening electrocardiogram to those with at least moderate symptoms, eliminating many of the current study’s patients who underwent electrocardiogram screening with only mild symptoms (Fig 2). 32
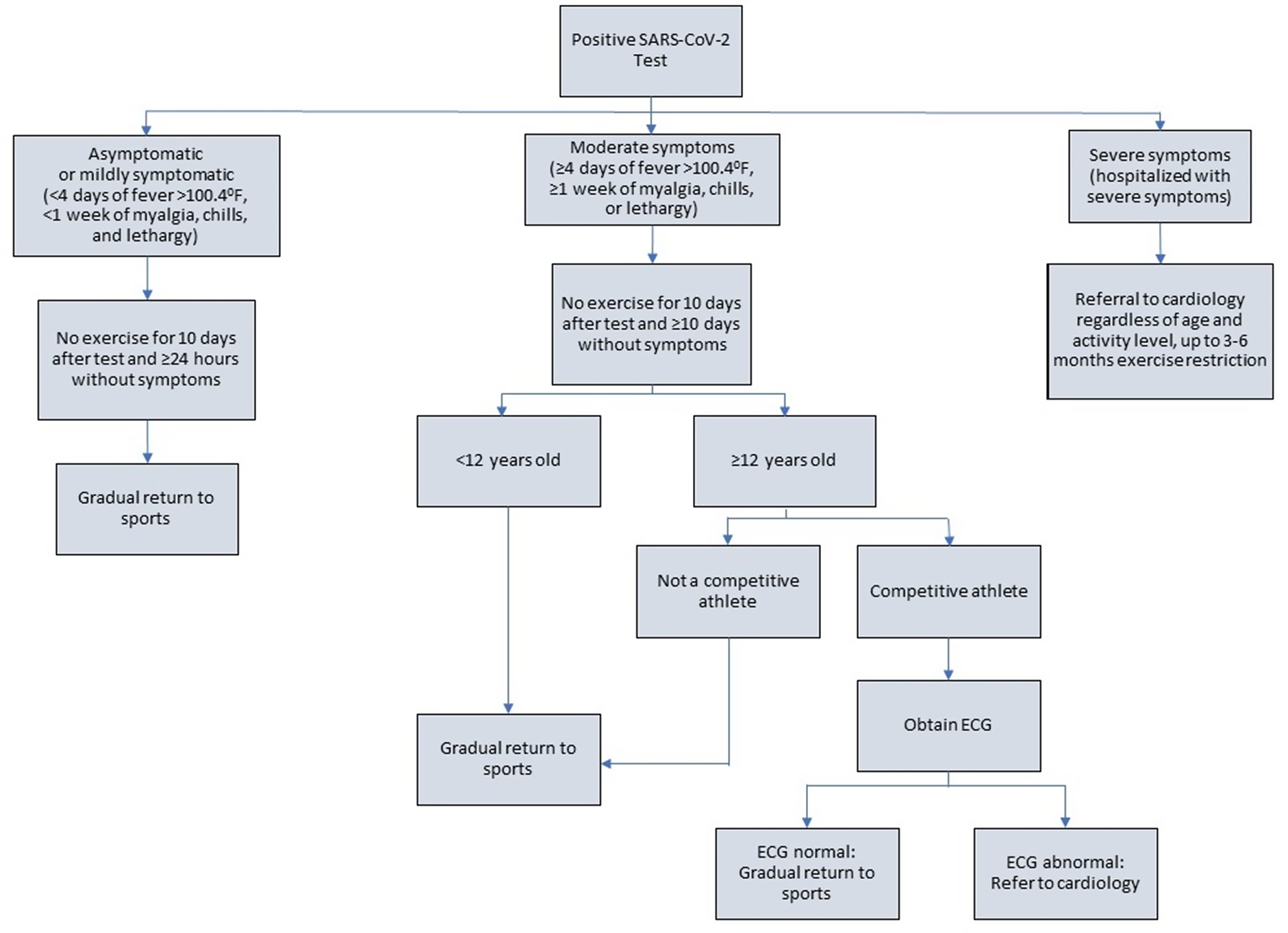
Figure 2. CHOP cardiology return-to-play algorithm.
As supported by the current data and reflected in the latest guidelines, electrocardiograms have a relatively low specificity for the detection of myocarditis after COVID-19, particularly in athletes, Reference Martinez, Tucker and Bloom13 and may not be beneficial as a screening tool in the absence of more significant baseline COVID-19 symptoms. Primary care providers, paediatric cardiologists, athletic trainers, schools, and others involved in the care of paediatric athletes must balance the risks of over-testing and exercise restriction with the small potential risk of myocarditis after COVID-19. To mitigate these risks, cardiologists must correctly identify well-recognised normal electrocardiogram variants in athletes, such as sinus bradycardia, incomplete right bundle branch block, right ventricular conduction delay, benign early repolarisation manifesting as diffuse non-specific ST segment elevation, and right atrial enlargement. Awareness of these normal findings is known to reduce workload and cost of screening significantly without compromising the ability to detect athletes with serious cardiac disease. Reference Sharma, Drezner and Baggish29,Reference Dhutia, Malhotra and Finocchiaro33
Study limitations
This study is retrospective and is subject to all of the biases inherent to this type of investigation. It was also conducted at a single centre and reflects the practices of our institution exclusively. Patients were identified through electronic medical record coding, which resulted in a small sample size and may not have produced an exhaustive list. Although our sample size was small, we posit that it is nevertheless representative of the general patient population being referred for these indications with involvement from a primary care referral network comprised of urban, suburban, and rural populations. Importantly, there was only one patient in our study with moderate symptoms and none with severe symptoms, so our data cannot be extrapolated to this potentially higher risk population. The fewer number of patients in the study cohort with moderate symptoms likely reflects the majority of patients experiencing milder symptoms. Patients with moderate symptoms may have also been more likely to be referred to cardiology due to symptoms alone, rather than obtaining a screening electrocardiogram and referring only if the electrocardiogram was abnormal. There were notably no African-American patients in our study population; it is unclear whether this difference is due to the small sample size not adequately representing the heterogenous population of athletes or if it is a reflection of broader disparities with respect to seeking and accessing the healthcare system. This observation is especially germane to our study, as racial and ethnic minorities have been shown to carry a higher burden of COVID-19 infection. Reference Abedi, Olulana and Avula34,Reference Goyal, Simpson and Boyle35 Finally, only one patient in our cohort underwent cardiac MRI, which has historically been considered the gold standard for the diagnosis of myocarditis. The true clinical significance, however, of an isolated abnormal cardiac MRI in the context of a prior COVID-19 infection and its impact on the risk of sudden cardiac death have not been well established. Reference Moulson, Petek and Drezner12
Conclusion
In a small cohort of children with prior COVID-19, who were primarily either asymptomatic or mildly symptomatic at the time of illness, subsequent screening electrocardiograms identified a variety of potential abnormalities prompting cardiology consultation. Many findings were well-recognised normal variants in adolescent athletes, and no patient was diagnosed with myocarditis following cardiology evaluation. The utility of screening electrocardiograms in this population prior to return-to-play remains unclear, although there is a definite risk of over-testing and likely low yield of informative data from electrocardiograms alone. Larger multi-centre studies are warranted to establish more comprehensive best practice guidelines, particularly with respect to patients with more severe disease.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121003012
Acknowledgements
We are grateful for all healthcare workers providing care for COVID-19 patients during this pandemic and certainly all patients and their families.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None







