The term right aortic arch is used for an aorta that arches over the right bronchus. The right aortic arch embryologically develops from the right fourth pharyngeal arch vessel and the right dorsal aorta. The prevalence of right aortic arch is 0.1% in the general population and 13–34 % in tetralogy of Fallot. Reference Liechty, Shields and Anson1,Reference Hastreiter, D’Cruz, Cantez, Namin and Licata2 Right aortic arch has been classified into two types in 1963 by Felson et al, based on branching patterns, with an embryological explanation. Reference Felson and Palayew3 In 1970, Shuford et al added another variant (isolated left subclavian artery), which led to the right aortic arch being classified into three types. Reference Shuford, Sybers and Edwards4 Mart et al in 2001 provided an embryological explanation for the right aortic arch with an isolated left brachiocephalic artery from the arterial duct. Reference Mart, Zachary, Kupferschmid and Weber5 Bein et al in 2006, and Banka et al in 2009, described another right aortic arch type, again with a proposed embryological explanation. Reference Bein, Saba, Patel, Reinhartz and Hanley6,Reference Banka, Geva, Powell, Geggel, Lahiri and Valente7 This entity consisted of the right aortic arch with an aberrant left brachiocephalic artery with a retro-oesophageal course, which was later labelled as type 4 by Mangukia et al. Reference Mangukia, Sethi, Agarwal, Mishra and Satsangi8
Our recent comprehensive analysis of a large number of aortic arch anatomies has led to a compendious description of the different types of right aortic arch, as seen in cases of tetralogy of Fallot (25% of which have a right aortic arch). Reference Prabhu, Kasturi and Mehra9
The previous classifications were based primarily on angiographic studies and chest X-rays, with embryological explanations. Reference Felson and Palayew3,Reference Shuford, Sybers and Edwards4 With the current availability of non-invasive cardiac imaging (computed tomography and magnetic resonance), we have a better definition of both arching patterns and branching patterns. All the subtypes can be diagnosed with standard cardiac imaging supported by intraoperative findings.
Classification and proposed embryological basis
We have classified the right aortic arch, originating from the fourth right pharyngeal arch artery, into 10 variants as shown in Table 1, with proposed embryological explanations. This classification does not include right arch arising from structures other than the right fourth pharyngeal arch vessel (for example, right-sided cervical aortic arch is not included in this classification) and it does not include right aortic arch with the circumflex aorta. Presence or absence of a right-sided arterial duct does not change the classification. The explanation is based on Rathke’s diagram of aortic arches and Edwards’s concept of double aortic arch Reference Edwards10 (Figs 1–4). We have modified Rathke’s diagram, as the latest literature supports the concept that the fifth pharyngeal arch never existed, and hence there cannot be a fifth arch artery. Reference Graham, Poopalasundaram, Shone and Kiecker11
Table 1. Embryology-based classification of the right aortic arch (RAA – right aortic arch, LSA – left subclavian artery, LCCA – left common carotid artery, PA – pulmonary artery, LPA – left pulmonary artery). In any type of RAA, the right arterial duct may be present, but its presence does not alter the classification
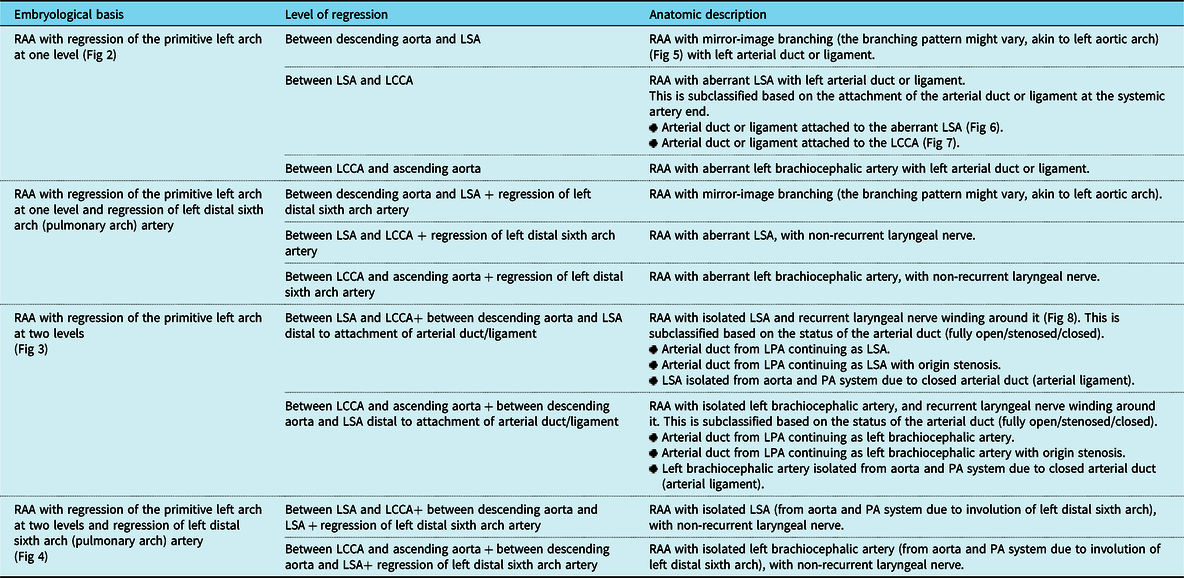

Figure 1. ( a ) – Rathke’s arch diagram demonstrating pharyngeal arch vessels (* depicts the seventh cervical intersegmental artery which is the future subclavian artery). We have shown the fifth arch artery as a discontinuous line as the latest literature suggests that it never existed. ( b ) – regression (painted brown) of primitive first, second, and fifth (never existed according to the latest literature) pharyngeal arch vessels and ductus caroticus (arrow) bilaterally. ( c ) – Edward’s double aortic arch concept depicted diagrammatically (1 – right common carotid artery, 2 – right subclavian artery, 3 – left common carotid artery, 4 – left subclavian artery, 5 – left-sided arterial duct, 6 – main pulmonary artery, 7 – right pulmonary artery, 8 – left pulmonary artery). Recent studies provide convincing evidence that there is never a fifth pharyngeal arch in humans, and hence there can never be a fifth arch artery. Reference Graham, Poopalasundaram, Shone and Kiecker11

Figure 2. Right aortic arch (RAA) with regression of the primitive left arch at one level. This can lead to three variants (and four phenotypes). RAA with mirror-image branching with left arterial duct or ligament (commonest type of RAA) ( a ), RAA with aberrant left subclavian artery (LSA) with left arterial duct or ligament ( b and c ) and RAA with aberrant left brachiocephalic artery ( d ). As shown in the figure, RAA with aberrant LSA with left arterial duct or ligament is further subclassified on the basis of attachment of arterial duct on the systemic artery side. RAA with aberrant LSA with arterial duct attachment to LSA forms a vascular ring. But in spite of being classified as RAA with aberrant LSA with left arterial duct, if the arterial duct is attached to left common carotid artery ( c ), it cannot form a vascular ring.
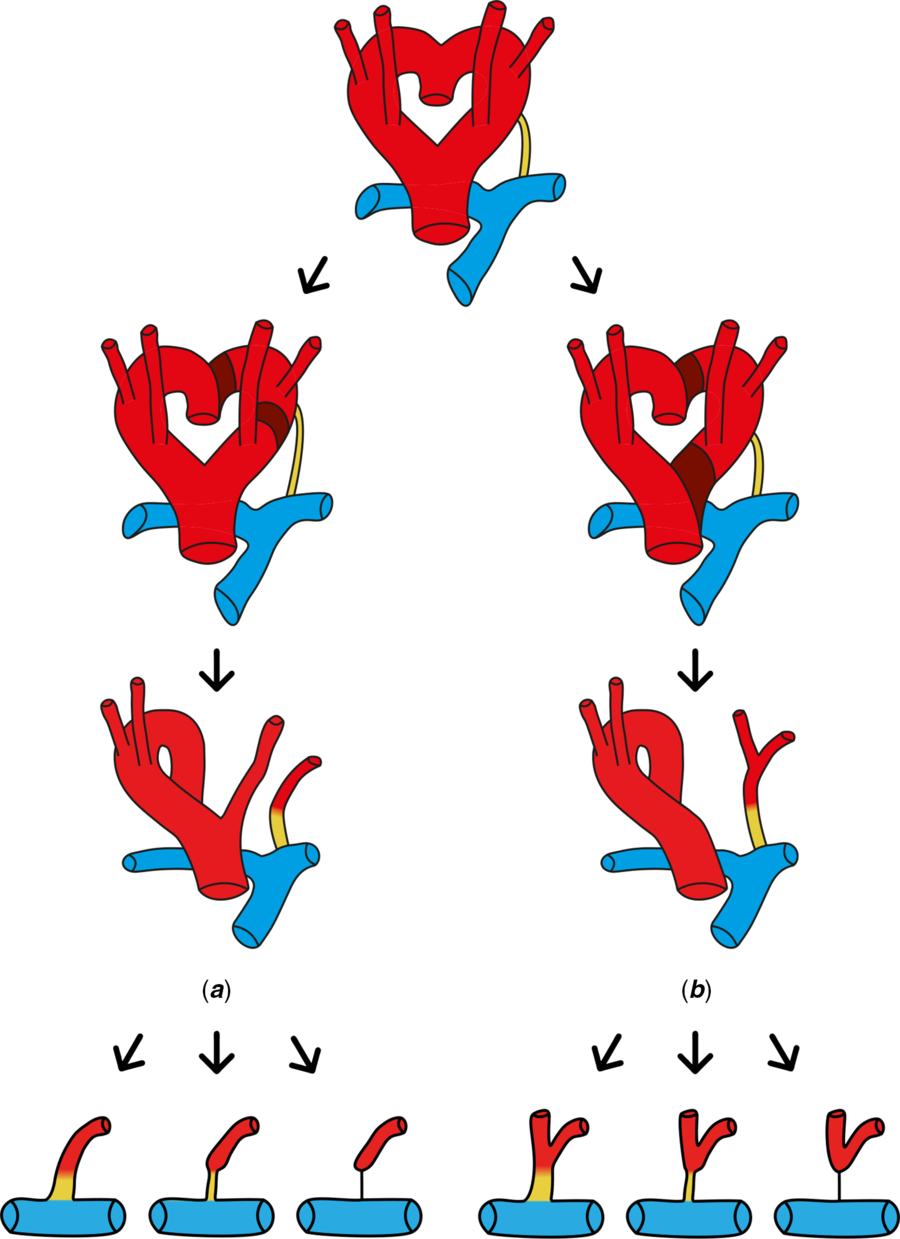
Figure 3. Right aortic arch (RAA) with regression of the primitive left arch at two levels. This leads to isolation of either left subclavian artery ( a ) or left brachiocephalic artery ( b ) with the recurrent laryngeal nerve (RLN) coursing around the artery. Both of these variants are further sub-classified into three types depending on the status of the arterial duct (fully open arterial duct – stenotic arterial duct – closed arterial duct or arterial ligament). RAA with the isolation of left subclavian or left brachiocephalic artery, when associated with a closed arterial duct, will cause isolation from pulmonary artery, but this is acquired; the RLN will course around the artery.

Figure 4. Right aortic arch (RAA) with regression of the primitive left arch at two levels and regression of distal sixth arch (pulmonary arch) artery. This leads to isolation of either the left subclavian artery ( a ) or left brachiocephalic artery ( b ) from both the aorta and from the pulmonary artery system. Here, isolation from the pulmonary artery system occurs because of involution of primitive left distal sixth arch (pulmonary arch), hence the nerve takes a non-recurrent course (as the fourth, fifth, and distal portion of sixth arch arteries have disappeared on the left side). The recent studies provide convincing evidence that there is never a fifth pharyngeal arch in humans, and hence there can never be a fifth arch artery.
Regression of the primitive left arch at one level
This includes three variants (and four phenotypes) with left arterial duct or ligament present in all. The embryological bases for these phenotypes are shown in Fig 2.
The first and most basic phenotype is right aortic arch with mirror-image branching (Fig 5). This is the most common type of right aortic arch. In our series of tetralogy of Fallot cases, which included 688 patients with right aortic arch, 86.8% had mirror-image branching, which matched with the published literature. Reference Prabhu, Kasturi and Mehra9,Reference Knight and Edwards12 Here, the branching pattern might be like any of the left arch classifications. Reference Liechty, Shields and Anson1

Figure 5. CT scan with three-dimensional reconstruction of RAA with mirror-image branching ( a – anteroposterior view, b – postero-anterior view). 1 – ascending aorta, 2 – left brachiocephalic artery as the first branch dividing into left common carotid artery (CCA) and left subclavian artery, 3 – right CCA, 4 – right subclavian artery (RSA), 5 – main pulmonary artery (MPA).
The second variant is right aortic arch with aberrant left subclavian artery. This is the second most common type, and constituted 10.6% of the right aortic arches in our series. Reference Prabhu, Kasturi and Mehra9 There are two phenotypes of this variant, depending on the site of insertion of the arterial duct to the systemic artery end (Fig 2). A vascular ring can be formed when the right aortic arch with aberrant left subclavian artery is associated with left arterial duct or ligament attached to the subclavian artery (Fig 6). But if the arterial duct or ligament is attached to the left common carotid artery, a vascular ring will not be formed (Fig 7). Thus, this disproves the historical belief that right aortic arches with aberrant left subclavian artery and left-sided arterial duct always cause a vascular ring.

Figure 6. CT scan with three-dimensional reconstruction of RAA with aberrant LSA and arterial duct attachment to LSA ( a – anteroposterior view, b – supero-inferior view, c – postero-anterior view). Here, the aberrant LSA is the last branch of the aorta and has a retro-oesophageal course. This, in the presence of left distal sixth arch remnant (arterial duct/ligament), causes a vascular ring (* in Fig 2b). 1 – ascending aorta, 2 – left CCA, 3 – right CCA, 4 – RSA, 5 – aberrant LSA, 6 – MPA, 7 – RPA, 8 – LPA, 9 – ductal pouch from MPA and ligament at aortic end (completes the ring).

Figure 7. CT scan with three-dimensional reconstruction of RAA with aberrant LSA and arterial duct attachment to left common carotid artery (CCA) ( a – anteroposterior view, b – postero-anterior view). Here, the aberrant LSA is the last branch of aorta, and has a retro-oesophageal course. But the distal sixth arch (pulmonary arch) remnant (arterial duct/ligamentum) is attached to the base of left CCA, hence not forming a vascular ring (i.e. all RAA with aberrant LSA and left-sided arterial duct cannot cause vascular ring like previously postulated). 1 – ascending aorta, 2 – left CCA, 3 – right CCA, 4 – RSA, 5 – aberrant LSA, 6 – descending aorta, 7 – MPA, 8 – LPA, 9 – RPA, arrow pointing to the arterial duct between left CCA and LPA (no vascular ring).
In the left aortic arch with aberrant right subclavian artery, the course of the aberrant artery can be retro-oesophageal, between trachea and oesophagus or pretracheal. Reference Myers, Fasel, Kalangos and Gailloud13 Similarly in a right aortic arch with aberrant left subclavian artery, the aberrant vessel can take one of the three courses, the most common being retro-oesophageal course. When associated with a left-sided arterial duct or ligament, the aberrant artery coursing behind the oesophagus or between the oesophagus and trachea can form a vascular ring. But right aortic arch with aberrant left subclavian artery with a pretracheal course and a left-sided arterial duct or ligament cannot cause a vascular ring, but can lead to extrinsic pressure symptoms (vascular compression in the absence of a vascular ring).
In patients with tetralogy of Fallot with right aortic arch and aberrant left subclavian artery, the left subclavian artery usually arises directly from the distal aortic arch. In contrast, normal persons (without intra-cardiac lesions) with right aortic arch and aberrant left subclavian artery invariably have an aortic diverticulum (Kommerell diverticulum) from which the left subclavian artery originates. Velasquez et al in 1980 explained the possible different embryologic events responsible for these two forms of aberrant left subclavian artery. Reference Velasquez, Nath, Castaneda-Zuniga, Amplatz and Formanek14
The third variant is right aortic arch with aberrant left brachiocephalic artery. This, when associated with a left-sided arterial duct or ligament, will form a vascular ring, when the aberrant artery courses behind the oesophagus or between the oesophagus and the trachea.
Regression of the primitive left arch at one level and regression of left distal sixth arch (pulmonary arch) artery
This group includes three variants similar to those seen when the primitive left arch regresses at one level, but there will be only three phenotypes (right aortic arch with mirror-image branching, right aortic arch with aberrant left subclavian artery and right aortic arch with aberrant left brachiocephalic artery). Since the distal portion of the artery of the left-sided pulmonary arch, previously known as the sixth arch artery has regressed, there will not be a left-sided arterial duct or ligament. These variants therefore cannot cause a vascular ring. But airway compression by a right aortic arch in the absence of a vascular ring (bronchial compression by the right-sided arterial duct) has been reported. Reference Agati, Guerra Sousa and Calvaruso15
Though these variants do not cause a vascular ring, the surgical importance lies in the course of the inferior laryngeal nerve. The typical course of the inferior laryngeal nerve is due to the embryological development of the aortic arch and supra-aortic vessels. As explained in the left aortic arch with aberrant right subclavian artery where the right nerve has a non-recurrent course, the anomaly is extremely rare on the left side. Reference Lee, Won and Oh16–Reference Natsis, Didagelos, Gkiouliava, Lazaridis, Vyzas and Piagkou20 The rarity is because right aortic arch is seen in only 0.1% of the general population, out of which about 10% will have an aberrant left subclavian or brachiocephalic artery. The majority (up to 50%) of the right aortic arches will a have left-sided arterial duct. Reference Liechty, Shields and Anson1,Reference Prabhu, Kasturi and Mehra9,Reference Knight and Edwards12 Thus right aortic arch with regression of primitive left arch at one level, associated with regression of left distal pulmonary arch artery (sixth arch artery), is an extremely rare variant, which is associated with non-recurrent course of the laryngeal nerve, and has been published. Reference Masuoka, Miyauchi, Higashiyama, Yabuta, Kihara and Miya21
Regression of the primitive left arch at two levels
This includes two variants (and three phenotypes in each variant). Regression at two levels causes isolation of the artery (left subclavian or left brachiocephalic), wherein the artery is no longer connected to the aorta. However, the isolated artery is connected to the pulmonary artery through the derivative of the distal sixth arch artery (the pulmonary arch), now the arterial duct or ligament. Since the recurrent laryngeal nerve courses around the primitive distal sixth arch artery, intraoperatively the recurrent laryngeal nerve is found to be coursing around the isolated artery. The embryological bases for these phenotypes are shown in Figure 3.
The first variant is right aortic arch with the isolation of left subclavian artery and recurrent laryngeal nerve winding around it. This was the variant with the least frequent occurrence amongst the three types explained by Shuford et al. Reference Shuford, Sybers and Edwards4 This variant can be subclassified based on the characteristics of the arterial duct or ligament, which include fully open arterial duct (Fig 8), stenotic arterial duct, and closed arterial duct (arterial ligament) (Fig 3).

Figure 8. CT scan with three-dimensional reconstruction of RAA with the isolation of LSA with left arterial duct ( a – anteroposterior view, b – postero-anterior view). Here, the ductus is originating from MPA and continuing as LSA (which is isolated from the aorta). 1 – ascending aorta, 2 – left CCA, 3 – right CCA, 4 – RSA, 5 – isolated LSA, 6 – MPA, 7 – LPA, 8 – RPA, 9 – descending aorta.
The second variant is right aortic arch with the isolation of left brachiocephalic artery and recurrent laryngeal nerve winding around it. A similar subclassification (see above) can also be applied to this variant.
In both of these variants, in which arteries are isolated from the aorta, closure of the left-sided arterial duct leads to isolation of the vessel from the pulmonary artery. Since the isolation from the pulmonary artery is acquired here, the recurrent laryngeal nerve will still course around the isolated artery.
Regression of the primitive left arch at two levels and regression of left distal sixth arch (pulmonary arch) artery
This includes two variants. Regression at two levels causes isolation of the artery (left subclavian or left brachiocephalic) from the aorta. But here, the isolated artery is not connected to the pulmonary artery either as the distal sixth arch artery (the pulmonary arch) on the left side has also regressed (absent left-sided arterial duct). Since the recurrent laryngeal nerve courses around the distal sixth arch artery, in these variants, the nerve will have a non-recurrent course. The embryological bases for these phenotypes are shown in Fig 4.
The non-recurrent course of the nerve is explained by the disappearance of the fourth, fifth (either regressed or never existed), and distal portion of the sixth (pulmonary arch) arches, on the left side (Fig 4). This theory is substantiated by the fact that up to 30% of tetralogy of Fallot patients do not have an arterial duct. Reference Kouchoukos, Blackstone, Hanley and Kirklin22 Moreover up to 28% of right aortic arches do not have an arterial duct on either side. Reference Knight and Edwards12
The differentiation between right aortic arch with isolated left subclavian artery and closed left arterial duct (arterial ligament) and right aortic arch with isolated left subclavian artery and absent left arterial duct can be made only intraoperatively, as imaging will show the vessel (left subclavian artery) isolated from both the aorta and the pulmonary artery system, and laryngeal nerves or the arterial ligament are not defined on the CT scan or MRI. The former will have an arterial ligament which attaches the left subclavian artery to the pulmonary artery, with the left-sided recurrent laryngeal nerve coursing around it. In the latter, there will not be an arterial ligament, and the nerve will take the non-recurrent course. The same is true for distinguishing right aortic arch with isolated left brachiocephalic artery and closed left arterial duct (arterial ligament) and right aortic arch with isolated left brachiocephalic artery and absent left arterial duct.
Though it was previously believed that the fifth arch artery is seen at least transiently, recent studies provide convincing evidence that there is never a fifth pharyngeal arch in humans, and hence there can never be a fifth arch artery. Reference Graham, Poopalasundaram, Shone and Kiecker11,Reference Bamforth, Chaudhry and Bennett23,Reference Gupta, Gulati and Anderson24 This concept might challenge Rathke’s hypothetical arch diagram, but the embryological basis for the development of right aortic arch would not change.
Ethics and institutional review board: Our hospital ethics committee waived consent for this study, as it is a theoretical article. Parental consent was obtained for use of all images.
Conclusion
We have put forth a new classification of the right aortic arch, which is supported by accepted embryological concepts and our own radiological evidence, as well as intraoperative findings. This will help in understanding the morphological basis for the formation of different types of right aortic arches. This classification helps to identify the surgically important right aortic arch variations. This also proves that all right aortic arches with aberrant left subclavian artery and left-sided arterial duct cannot cause a vascular ring. An embryological explanation for the course of the recurrent laryngeal nerve in such cases is also provided. Advances in imaging technology might identify further anatomic variants relevant to this classification.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.












