Following the first report of transcatheter occlusion of ventricular septal defects using a Rashkind double umbrella device,Reference Lock, Block, McKay, Baim and Keane1 various devices, such as the Clamshell (C.R. Bard, Inc., Billerica, Massachusetts, United States of America),Reference Bridges, Perry and Keane2 the CardioSEAL® (NMT Medical, Boston, Massachusetts, United States of America),Reference Knauth, Lock and Perry3 the buttoned device,Reference Sideris, Walsh, Haddad, Chen, Ren and Kulkarni4 and coilsReference Chaudhari, Chessa, Stumper and De Giovanni5 have been used, mainly for closure of muscular septal defects, and with limited success. Use of the Amplatzer® Muscular VSD occluder (AGA Medical Corporation, Golden Valley, Minnesota, United States of America) improved results,Reference Holzer, Balzer, Cao, Lock and Hijazi6 but did not offer a solution to transcatheter closure of perimembranous ventricular septal defects due to the distinct anatomical characteristics of the membranous septum, including its thickness, and its proximity to the aortic and tricuspid valves. Although use of the eccentric occluder developed from the occluder used to close muscular defects yielded very promising initial results without significant complications,Reference Bass, Kalra and Arora7 disturbances of conduction, including acute or long-term development of complete heart block, have emerged as serious complications in larger recent studies.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8 The reason for this alarming incidence of conduction disturbances lies in the close association of the atrioventricular conduction axis to the rims of the defect, especially the remnant of the membranous septum.Reference Anderson, Becker, Stark and deLeval9 The as yet undefined incidence of complete heart block, which may be lethal or necessitate placement of a pacemaker, represents an important factor in the decision to close interventionally a perimembranous ventricular septal defect. In this report, we describe our experience with the eccentric Amplatzer occluder, focussing on the acute and long-term disturbances of conduction disturbances after implantation, and reviewing both the anatomical and device-related considerations concerning those changes.
Materials and methods
Patients
We selected patients by clinical examination and transthoracic echocardiography having isolated perimembranous ventricular septal defect with left ventricular volume overload and enlarged left ventricular dimensions for age and size for interventional closure. Patients with an aortic rim of the defect judged to be less than 2 millimetres by echocardiography in the long-axis view, those with other associated defects, and those with elevated pulmonary vascular resistance were all excluded. Patients from collaborating hospitals were included only where the first author was directly involved.
The device
Like other devices manufactured by the AGA Medical Corporation, based at Golden Valley, Minnesota, United States of America, the two available devices for closure of ventricular septal defects are constructed from self-expandable nitinol wire mesh woven into two low-profile discs, with fabric baffles inside the discs and waist to promote thrombosis. The occluder designed for closure of perimembranous defects (Fig. 1) has a short waist of 2 millimetres diameter to minimize contact with the tricuspid valve. The left disc is asymmetric, with a superior rim of 0.5 millimetres to avoid the aortic valve, and a larger inferior rim of 5 millimetres, marked with platinum, to clasp the ventricular septum. The right disc is 2 millimetres larger than the waist on both sides. The device designed for closure of muscular defects consists of a central waist connecting two symmetric discs, both of which are 4 millimetres larger than the waist. Both devices are recapturable and redeployable, and have diameters of the waist varying from 4 to 18 millimetres in 2 millimetre increments. The delivery system consists of a sheath and dilator, a delivery cable, and a pusher catheter, with modifications for the perimembranous occluder to ensure alignment of the aortic rim of the left disc with the aortic valve.

Figure 1 Profile of the Amplatzer® Membranous VSD Occluder with a short 2 millimetres waist, of diameter 12 millimetres, a minimal superior rim toward the aorta, and a longer 5 millimetres inferior rim.
Procedure and implantation
Informed written consent was obtained from the patient or their guardian prior to the procedure. All procedures were performed under general endotracheal anaesthesia with continuous transoesophageal echocardiography guidance. The procedure we followed has been previously reported in detail.Reference Bass, Kalra and Arora7, Reference Pedra, Pedra and Esteves10 Briefly, access was obtained through the femoral artery and vein, and complete right and left heart catheterization was performed on 21% inspired oxygen to evaluate the degree of left-to-right shunting, and the pulmonary vascular resistance by the Fick method. Left ventriculography in the long axial oblique view of 60 degrees left anterior oblique and 20 degrees cranial was used to define the location and size of the ventricular septal defect and its distance from the aortic valve. The size of the occluder chosen was equal or up to 2 millimetres larger than the size measured by echocardiography or angiography. With establishment of an arteriovenous loop, the left ventricular disc was deployed with the platinum marker pointing to the apex of the heart, followed by deployment of the right ventricular disc. After confirmation of good position, and absence of interference of the occluder with the aortic valve both by echocardiography and left ventriculography, the occluder was released. Left ventriculograms and aortograms were obtained to assess residual shunting and possible aortic regurgitation.
During the procedure, all patients received heparin at 100 units per kilogram and antibiotics, either flucloxacillin or cephazolin, and were discharged to home the day after the procedure. The policy of additional medications after the procedure differed slightly in the collaborating hospitals, for instance oral aspirin were not given in Oslo, while patients of the other institutions were discharged on oral aspirin at 3 to 5 milligrams per kilogram per day for 6 months. All patients were instructed to receive prophylaxis for endocarditis until complete closure was documented. Follow-up at 24 hours, 1, 3, 6, 9, 12 months and yearly thereafter included a physical examination, electrocardiogram and transthoracic echocardiogram, while a chest radiograph was performed 24 hours and 6 months after the procedure.
Statistics
Descriptive data are expressed as means plus or minus standard deviations with median and range, as appropriate.
Results
Patients and procedural data
Between May, 2002, and March, 2006, 35 patients, 18 male and 17 female, with a median age of 4.5 years and median weight of 16 kilograms underwent percutaneous transcatheter occlusion of isolated perimembranous ventricular septal defects using the Amplatzer device at our institutions (Table 1). The median ratio of pulmonary to systemic flows was 1.9, with median fluoroscopic time of 27 minutes, and median procedural time of 156 minutes. Aneurysm of the membranous septum was found in 6 patients, 2 of which underwent balloon dilation of the aneurysm prior to occlusion to permit smooth passage of the delivery sheath. A membranous occluder was used in all but 3 patients. In these patients, a distance of 4 to 7 millimetres was measured from the aortic valve, so we inserted a muscular occluder. In 1 patient, we performed balloon dilation of a stenotic pulmonary valve at the same session.
Table 1 Characteristics of the patients.

Rate of closure rate and follow-up
Median follow-up was 2.5 years. Immediate occlusion was shown angiographically in 5 (14%) patients, with a rate of complete closure of 53% at 1 month, 63% at 3 months, 73% at 6 months, and 87% and 91% at 1 and 2 years, respectively. One patient had mild aortic insufficiency after release of the occluder, and underwent surgical removal of the occluder and closure of the defect. Discounting this patient, eventual complete closure was achieved in all but 3 patients. Of these, 2 had a persistent but minimal residual shunt for 2 years without left ventricular dilation, while another had a moderate residual shunt without decrease over the next 2 years, and underwent surgical closure of the residual defect with a patch, leaving the occluder in place. Aside from the last patient, all other patients in this cohort had gradual resolution of left ventricular enlargement without other symptoms.
Fourteen patients had trivial tricuspid regurgitation before the procedure without changes immediately after occlusion and during follow up. New-onset trivial to mild tricuspid regurgitation during the procedure was observed in 14 patients; during follow-up, tricuspid regurgitation decreased to trivial or absent in 11 of these patients but persisted as mild in 3 patients (8.8%). Trivial aortic regurgitation has been observed in 4 patients before the procedure, and did not change immediately after occlusion and during follow up. Trivial to mild aortic regurgitation was observed as a new finding in 9 patients during the procedure, albeit disappearing in 7 of these, but persisting as trivial regurgitation in 2 patients. In addition, 4 patients developed trivial aortic regurgitation during the period of follow-up, bringing to 6 (17.6%) the total number of patients with aortic insufficiency due to the procedure at follow-up.
Disturbances of conduction
Abnormalities directly related to the procedure occurred in 7 patients (20%). This was transient left bundle branch block in 1 patient, while 6 patients (17%) had permanent disturbances. Of those, 2 patients had left anterior hemiblock, 2 had right bundle branch block and 1 had bifascicular block one day after implantation, changing to right bundle branch block after 6 days, including 4 days of treatment with corticosteroids. The remaining patient, with a defect measuring 3.5 millimetres on angiography, and 4 by 8 millimetres on transoesophageal echocardiography, had an occluder of 8 millimetres diameter placed without complications, albeit with a trivial residual shunt, which had disappeared at the follow-up visit after 1 month. The state of the occluder immediately after implantation, with a compressed central waist and bulging right ventricular disc, is shown in Figure 2a. The patient was discharged the next day in sinus rhythm with left bundle branch block, but developed intermittent second-degree atrioventricular block, of Mobitz type II, 6 months after implantation. At that time, fluoroscopy showed the occluder in good position, with full expansion of the waist and flattening of the right ventricular disc (Fig. 2b).
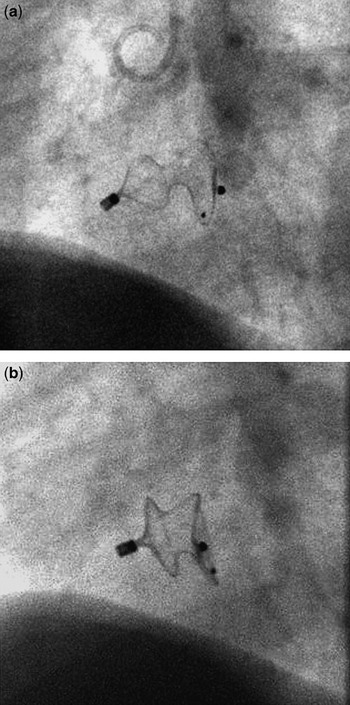
Figure 2 The long axial oblique projection immediately after placement of an 8 millimetres occluder in a perimembranous ventricular septal defect (a) shows a compressed central waist and bulging of the right ventricular disc of the occluder. The same projection after development of Mobitz II second-degree atrioventricular block 6 months after implantation (b) shows a good position of the occluder, with full expansion of the waist and flattening of the right ventricular disc.
Complications
Aside from the disturbances of conduction described above, 2 patients had transient ventricular ectopic beats and couplets 24 hours after implantation with spontaneous resolution. In 3 patients, the initial attempt at occlusion with a device of 6 millimetres, and in 1 patient a 10 millimetres occluder, showed inadequate stabilization, so the occluders were all replaced with a new device of the next size during the same session, the operator achieving a good position and ultimate complete closure in all 4 patients. As already discussed, 2 patients required surgical intervention; the first for repair of a moderate residual defect with a patch, leaving the occluder in place, and the second for retrieval of the occluder and closure of the defect due to mild aortic insufficiency caused immediately by the occluder. We had no episodes of embolization of the occluder, haemolysis, or obstruction of the left ventricular outflow tract.
Discussion
We report here our results with transcatheter closure of perimembranous ventricular septal defect using the Amplatzer device specifically designed for this purpose, with emphasis on the abnormalities observed in atrioventricular conduction, as well as their likely anatomical substrate. The rate of complete closure was 91%, in keeping with previous experiences,Reference Bass, Kalra and Arora7, Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8, Reference Fu, Bass and Amin11 with only 1 patient requiring further intervention for a haemodynamically significant residual shunt. Only 3 patients (8.5%) showed persistent mild tricuspid regurgitation at follow-up related to the insertion of the device, again in agreement with previous reports.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8 More alarmingly, however, we encountered persistent trivial aortic insufficiency immediately or during follow-up in a total of 6 patients (17.6%), albeit again in accordance with previous studies.Reference Fu, Bass and Amin11 Although complete heart block was not noted in our patients, the incidence of transient (3%) and permanent (17%) disturbances of atrioventricular conduction, as well as the delayed progression in one case, illustrates the importance of understanding the anatomy of the area (Fig. 3), and the potential risks of interventional closure of such perimembranous defects.

Figure 3 The course of the atrioventricular conduction tissuesReference Anderson, Becker, Stark and deLeval9 (dotted line) relative to perimembranous ventricular septal defects Reproduced by kind permission of Robert H. Anderson and Anton E. Becker.
It is rare for a perimembranous ventricular septal defects to be the consequence of simple deficiency of the interventricular component of the membranous septum. Instead, most cases are due to deficiency of the muscular septum that forms the circumference of the membranous area, the membranous septal remnant itself frequently becoming aneurysmal in an attempt to close the defect.Reference Anderson, Becker, Stark and deLeval9 The most vulnerable point of the defect is the site of penetration of the atrioventricular conduction axis, which may be enclosed within the membranous septal remnant. After it has penetrated, the axis tends to veer to the left side of the defect, thus making the crest of the ventricular septum in most instances, but not always, free of conduction tissue.Reference Anderson, Becker, Stark and deLeval9
Surgical repair of such defects has also been associated with conduction disturbances, most frequently right bundle branch block in up to 79% of patients,Reference Hobbins, Izukawa, Radford, Williams and Trusler12 while the incidence of complete heart block varies can be up to 4% after operative closure.Reference Houyel, Vaksmann, Fournier and Davignon13 We may doubt whether this reported high incidence is still the reality in specialist centres nowadays, but it is known that onset of life-threatening complete heart block could be acute or delayed, even 15 years after surgical repair of ventricular septal defect, especially in the presence of postoperative disturbances of conduction such as bifascicular block.Reference Fukuda, Nakamura, Iemura and Oku14 The abnormalities are due to direct injury of the conduction tissues that are in close proximity with the rim of the defect, the surgical technique and depth of the stitches being known to affect their incidence.Reference Fukuda, Suzuki, Kashima, Sato and Morikawa15
Transient disturbances of conduction during transcatheter occlusion of perimembranous defects may be produced by manipulation of the catheter at the rims of the defect. Care should be taken, therefore, to cross the defect from the left ventricle with a floppy wire to minimize trauma.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8 Transient abnormalities may also be due to local oedema and inflammation, a fact that has prompted some investigators to use corticosteroids and anti-inflammatory agents after insertion, with encouraging results.Reference Yip, Zimmerman and Hijazi16
Permanent abnormalities of conduction, including right bundle branch block and left anterior hemiblock, as seen in our study, have been noted by previous investigators.Reference Masura, Gao and Gavora17 Permanent complete heart block requiring insertion of a pacemaker after closure of perimembranous defects with the Amplatzer device was reported in the initial studies with an incidence from 3 to 4%, and was also seen in more recent larger studies.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8, Reference Fu, Bass and Amin11, Reference Masura, Gao and Gavora17 The specially designed occluder, made of nitinol wire mesh, and with a shape memory, is gaining increasing popularity in various centres due to its efficiency in producing high rates of closure, which is attributable to its mechanism of closure, namely stenting the defect with the nitinol waist. This mechanism, however, produces of necessity continued pressure by the waist on the rim of the defect, including the conduction tissue, and this is probably the cause of the observed disturbances of conduction. This becomes especially important should an oversized occluder be inserted, as was probably the case in our patient shown in Figure 2, where the waist initially appeared compressed, and there was mushrooming of the right ventricular disc of the occluder. Continued force of the waist against the defect rim over the next 6 months may be the cause of progression of left bundle branch block to intermittent Mobitz type II second-degree atrioventricular block, accompanied by expansion of the waist and the right ventricular disc. Our observation of serious disturbances of conduction, despite a good position and expansion of the occluder without residual shunting, is in agreement with previous reports.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8 We should realize that defects themselves are frequently elliptical in shape, and ‘correct’ sizing of the occluder in one plane of the defect may lead to oversizing in the orthogonal plane, with the result of relentless pressure of the nitinol waist trying to resume its cylindrical shape in an oval hole damaging the conducting tissues in its rim.
Delayed progression of the abnormalities of conduction even into lifet-hreatening complete heart block has been reported both after surgicalReference Bonatti, Agnetti and Squarcia18 and interventional occlusion.Reference Carminati, Butera, Chessa, Drago, Negura and Piazza8, Reference Masura, Gao and Gavora17 This finding is particularly disconcerting, as it involves apparently healthy individuals. Careful long-term follow-up, and frequent monitoring of rhythm, is advocated at least until the incidence and outcome of heart block after transcatheter closure of perimembranous ventricular septal defects is fully elucidated with larger long-term studies.
In conclusion, we have found that the Amplatzer occluder designed specifically for closure of perimembranous defects is an effective device, producing limited complications, which are equal to, or probably even higher, than those produced by surgical closure nowadays by those working in specialist centres. The incidence of immediate, and more importantly long-term, evolving disturbances of conduction in our experience, and the previously reported incidence of complete heart block, along with the known proximity of the atrioventricular conduction tissues to the rim of the defect, raise concerns. They stress the importance of larger and longer studies to assess the safety and risks of this procedure as an alternative to surgical closure.
Addendum
Since the paper was accepted for publication, we know that a four year-old patient developed complete heart block 11 months after closure of a ventricular septal defect, requiring implantation of a pacemaker.






