Rheumatic heart disease is the only sequelae of acute rheumatic fever with potentially lifelong morbidity. Reference Gururaj, Choo, Ariffin and Sharifah1 It is the result of an immunological response to the cardiac myocyte after an infection with Group A streptococci bacterium in susceptible individuals. Despite being a preventable disease, it is among the leading causes of acquired valvular heart disease in Sabah and throughout the developing world, with 33.4 million cases and 319,400 deaths reported worldwide in 2015. Reference Watkins, Johnson and Colquhoun2 It is recognised that mortality rates were highest in Oceania, South Asia, and central sub-Saharan Africa. Reference Watkins, Johnson and Colquhoun2 However, despite concerted efforts to set up a national registry for Kawasaki disease, an acquired disease of the coronary vessels, a unified effort for continuous data monitoring for rheumatic heart disease among the aforementioned population remains elusive.
Sabah is recognised as the poorest state in Malaysia and as recent as April 2019, Sabah, together with two other states (Kelantan and Kedah) scored lowest in terms of per capita income. Reference Hassan3 Rheumatic heart disease itself is a disease of poverty, and its associations with overcrowding and lower socio-economic status were well documented. Reference Jaine, Baker and Venugopal4,Reference Okello, Kakande and Sebatta5 Although there are data on rheumatic heart disease that were published from the state of Kelantan in the 1990s, there has been no data produced on the paediatric population in Sabah. Realising this fact, we analysed the data of acute rheumatic fever admissions among the paediatric population in all tertiary hospitals of Sabah from 2016 to 2018. We hope these data will promote interest in the establishment of a national registry for paediatric rheumatic heart disease.
Materials and method
This is a retrospective cohort study. All records of admissions to paediatric wards in tertiary hospitals in the state of Sabah for acute rheumatic fever from January 2016 to December 2018 were collected. The information from patients’ records was collected by investigators and liaison staff. Records with incomplete data were excluded from the study. Acute rheumatic fever was diagnosed based on the Australian Criteria for Acute Rheumatic Fever Diagnosis (Second Edition). Reference Carapetis, Brown and Maguire6 The initial 2-D echocardiography and electrocardiogram were reviewed by a single paediatric cardiologist. We defined our population as high risk and used the corresponding criteria for diagnosis. Chest radiographs were defined as abnormal in the presence of cardiomegaly (cardiothoracic ratio of more than 0.5), pleural effusion (blunted costophrenic angles or gross opacities suggestive of pleural effusion), or plethoric lung fields (prominent pulmonary vasculature). All chest radiographs were reviewed by the respective patients’ paediatricians. Anti-streptolysin O titre was defined as positive at more than 200 IU/ml based on our laboratory-accepted upper limit of normal. All patients were managed by their respective paediatricians as planned by the paediatric cardiologist after being diagnosed. The data collected in forms were then tabulated and analysed using SPSS, and descriptive analysis was performed. Further chi-square analysis (Pearson’s) was done to calculate p-value and establish co-relations between the variables.
Results
There were 55 cases of acute rheumatic fever during the period of the study. Of these cases, 3 were excluded from the study due to incomplete data and the remaining 52 were analysed. The incidence of acute rheumatic fever was 74.4 per 100,000 paediatric admissions over a period of 3 years. Most patients were male (n = 35, 67.3%), and of the indigenous Kadazan-Dusun ethnicity (n = 21, 40.4%) (Table 1). The mean age at time of presentation was 9.58 years (SD 2.6, range 3–14). The majority of patients seen were in the West Coast (n = 24, 46.2%) and Kudat divisions of Sabah (n = 13, 25%).
Table 1. Demographic data of patients with acute rheumatic fever in the paediatric population in Sabah.

Most admissions were for newly diagnosed acute rheumatic fever (n = 39, 75%) and 13 cases (25%) were for recurrent rheumatic fever (Table 2). Most patients presented with carditis (n = 51, 98.1%) followed by polyarthritis (n = 28, 53.8%), erythema marginatum (n = 8, 15.4%), and subcutaneous nodules (n = 2, 3.8%). No patients presented with Syndenham’s chorea. For minor manifestations, 39 patients (75%) had fever on presentation, 44 patients (84.6%) had raised erythrocyte sedimentation rate or C-reactive protein, and 19 patients (36.5%) were found to have prolonged PR interval on their electrocardiogram. There were 36 patients (69.2%) with abnormal chest radiograph on presentation compared to 13 patients (25%) with normal chest radiograph on presentation.
Table 2. Clinical data of patients with acute rheumatic fever in the paediatric population in Sabah.
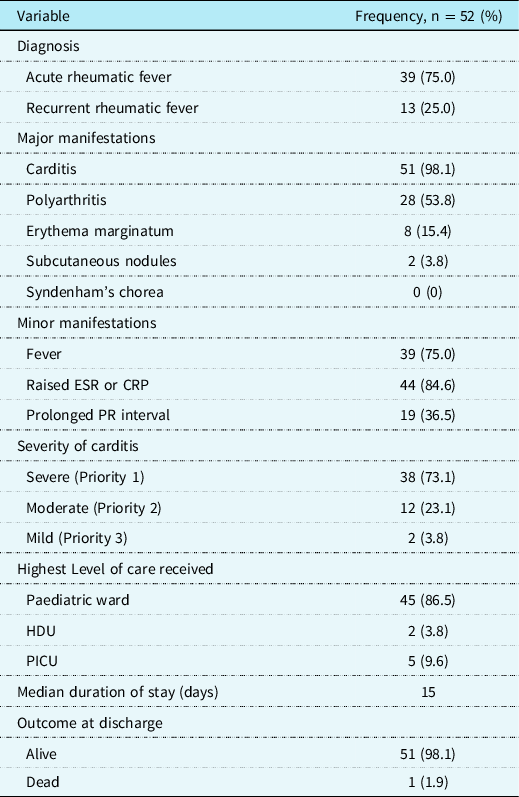
Abbreviations: CRP = C-reactive protein; ESR = erythrocyte sedimentation rate; HDU = high dependency unit; PICU = paediatric intensive care unit.
We found that the median total white count was 12.1 109/L, while the mean platelet count was 490.8 109/L (SD 181.3). The anti-streptolysin O titre was found to be positive in 38 patients (73.1%) and negative in 12 patients (23.1%), while 2 cases were not available (3.8%). (Table 3).
Table 3. Investigations of patients with acute rheumatic fever in the paediatric population in Sabah.

Abbreviations: ASOT = anti-streptolysin O titre.
* Median used as data was skewed.
Echocardiography revealed that 22 patients (42.3%) had 2 valves affected, 21 patients (40.4%) had 3 valves affected each, while only 7 patients (3.5%) had single valve involvement. In terms of affected valves, 49 patients (94.2%) had mitral valve involvement, 34 patients (65.4%) had aortic valve involvement, and 20 patients (61.6%) had tricuspid valve involvement.
All patients admitted were treated based on the Paediatric Protocols for Malaysian Hospitals. Reference Haji Muhammad Ismail, Hoong Phak and Thomas7 Patients with moderate to severe valve disease (n = 40, 76.9%) were treated with prednisolone followed by aspirin, while eight patients (15.4%) with mild to moderate valve disease were treated with aspirin alone. Patients with severe heart failure on presentation were treated with intravenous methylprednisolone (n = 3, 5.8%) and only one patient was given intravenous hydrocortisone as initial treatment due to multiple-organ failure.
When categorised by severity using the 2020 Australian Rheumatic Heart Disease Guidelines Priority Classification, Reference Bowen, Currie and Katzenellenbogen8 the majority of cases admitted (n = 38, 73.1%) were categorised as severe rheumatic heart disease (Priority 1), followed by 12 patients (23.1%) with moderate disease (Priority 2) and only 2 patients (3.8%) with mild disease (Priority 3) (Table 2). The patients had a median length of stay of 15 days in the hospital. One mortality (1.9%) was recorded during this period, whereby the patient was diagnosed with severe heart failure with sepsis and multiple-organ failure, while another patient was discharged with significant morbidity after suffering from cerebral emboli secondary to infective endocarditis (Table 2).
We found no significant correlation between the patients’ demographics such as age, gender, locality and race with severity of disease. However, we found that with increasing severity, the duration of stay lengthened as did presence of abnormal chest radiograph on presentation. (Table 4)
Table 4. Comparison based on severity of patients with acute rheumatic fever in the paediatric population in Sabah.

Abbreviations: ASOT = anti-streptolysin O titre; CRP = C-reactive protein; ECG = electrocardiogram; ESR = erythrocyte sedimentation rate.
* p-Value <0.05 on chi-square analysis.
Discussion
In a recent review by Watkins et al, Malaysia, alongside Thailand and Vietnam, were highlighted in the Southeast Asian region as being non-endemic for rheumatic heart disease. Reference Watkins, Johnson and Colquhoun2 However, similar to Australia and New Zealand, there are areas of high susceptibility to rheumatic heart disease in the Bornean states where indigenous people are concentrated, and where access to healthcare remains logistically difficult for a large part of the population. It is noteworthy that the data on Malaysia in Watkins’ review only comprised of fatal cases, highlighting the lack of updated data on rheumatic heart disease in this country.
In this study, we undertook a retrospective review of all admissions for acute rheumatic fever to all hospitals in the Bornean state of Sabah for the period of 2016–2018. The number of cases appear to be highest in the West Coast region, where it is also the most densely populated and where it is easier logistically to reach healthcare services. Based on the total number of admissions, we estimate the incidence of in-hospital acute rheumatic fever to be 74.4 per 100,000 paediatric admissions over the 3 years studied. This number is significantly higher than a similar study done in Kuala Lumpur in 1995 where the incidence was 21.2 per 100,000 paediatric admissions per year. Reference Omar9
In our cohort, there appears to be a higher male-to-female ratio (2:1) among children admitted for rheumatic carditis. This is comparable to data in the Southeast Asian region; Reference Seckeler and Hoke10 however, it contrasts with the Global Rheumatic Heart Disease Registry (REMEDY), where females predominate throughout most age ranges. Reference Zühlke, Engel and Karthikeyan11 It also differs from the Northern Territory rheumatic heart disease registry data published by Cannon-et al, where females generally predominate in the 5–14 years range. Reference Cannon, Roberts, Milne and Carapetis12
Among all the indigenous races, the Kadazan-Dusun population makes up the largest number of admissions. This is not surprising given the fact that they make up about 25% of the population in the state of Sabah. Other indigenous ethnic groups such as the Bajau, Suluk, and Rungus populations were equally affected. The occurrence of this condition across diverse ethnic groups reflects the underlying widespread socio-economic disadvantage throughout the state. Reference Nascimento and Beaton13
The incidence of initial cases of acute rheumatic fever is highest in children aged 5–14 years Reference Carapetis, Beaton and Cunningham14 , with patients presenting a mean age of 9.58 years. Although it is uncommon to have patients presenting below 5 years of age, there was a 3-year-old patient who presented with severe mitral regurgitation and fulfilled the definitive criteria for acute rheumatic fever. In our analysis, the number of patients seemed to taper beyond 14 years of age, because some of the older children beyond 15 years old were admitted to adult medical wards. This may result in non-capture of some of the adolescent cases.
While most patients presented as the first onset of rheumatic fever, of concerning note was the high proportion of patients presenting with recurring acute rheumatic carditis (25%). This raises the alarm that secondary prevention measures in the state need further strengthening via multidisciplinary and multi-level effort. Adherence remains a major concern amongst the poor who can barely afford the cost of transportation, and the many hours of travel to the nearest healthcare facility. In Sabah, a 28-day benzathine penicillin regime was enforced. Although there were concerns that serum penicillin levels may be inadequate after a 4-week interval as compared to a 21-day regime, a study in Auckland demonstrated a very low failure rate at 0.07 per 100 patient years in the 28-day regime. Reference Lue, Wu, Wang, Wu and Wu15,Reference Spinetto, Lennon and Horsburgh16 Further long-term studies may be needed in our setting to assess which regime would be best in reducing the rate of local recurrence.
We recognise that 23.1% of our cohort did not have positive anti-streptolysin O titre despite fulfilling definitive clinical criteria for rheumatic heart disease. These data are comparable to data in the region (Table 5) where 60.9% of anti-streptolysin O titre was positive. Reference Seckeler and Hoke10 The anti-streptolysin O titre should ideally be repeated 10–14 days later to demonstrate a rise in the titre. However, due to delay in obtaining results from the lab in our setting, most patients would have benefitted from immediate treatment on clinical grounds. Apart from that, more sensitive tests for evidence of preceding streptococcal infection like DNAse B or rapid antigen testing were not available in our centre.
Table 5. Comparison for percentage of major and minor criteria with meta-analysis by Seckeler et al.

Abbreviations: ASOT = anti-streptolysin O titre; CRP = C-reactive protein; EM = erythema marginatum; ESR = erythrocyte sedimentation rate; RF = rheumatic fever; SCN = subcutaneous nodules.
About three-quarter of admitted patients fell into the severe carditis category (73.1%). Based on global estimates that mild and moderate disease form the largest group of patients, it is very likely that a significant number of patients were not picked up in the community and referred for evaluation. Reference Cannon, Roberts, Milne and Carapetis12 This is further highlighted when 98.1% of the patients we observed presented with carditis as compared to the 66% reported in the Southeast Asian region. Reference Seckeler and Hoke10 (Table 5).
Most patients had more than one valve involvement at diagnosis. Consistent with global findings, the valves affected in order of the most common to the least common were the mitral, aortic, and tricuspid valves, respectively. A large number of patients in our cohort had three-valve disease (mitral, aortic, and tricuspid valves) at presentation, followed by equal proportions of mitral plus aortic valve and mitral plus tricuspid valve.
Majority of our cohort were treated initially with corticosteroids followed by aspirin, as most of them had severe disease at presentation. The remainder received aspirin alone. Although a recent Cochrane review did not find superiority of corticosteroids above aspirin in the treatment of acute rheumatic fever, most guidelines incorporate corticosteroids as an immunomodulatory regimen for severe disease. Reference Bowen, Currie and Katzenellenbogen8,Reference Cilliers, Adler and Saloojee17 Three of our patients received intravenous methylprednisolone. In a small study comparing intravenous steroid with oral corticosteroids in Brazil, there appears to be better treatment outcomes with the oral regimen. Reference Nassri Câmara, Vieira Braga, Alves-Silva, Câmara and Da Silva Lopes18 On the other hand, a study by Torres et al found that combining pulse methylprednisolone and oral prednisolone appear to contribute to both reduced left chamber dimensions and prevention of rebound phenomenon. Reference Torres, Torres, Torres and Torres19
A meta-analysis of the treatment of Group A streptococcus pharyngitis to prevent acute rheumatic fever concluded that there would be an approximately 60% reduction in cases of acute rheumatic fever if pharyngitis was appropriately treated, especially in endemic areas. Reference Lennon, Kerdemelidis and Arroll20 The large number of cases among the paediatric population underlines the need for more efforts in the public health sector for primary prevention, given the relative ease and low cost of Group A streptococcus pharyngitis treatment.
There are limitations to this study. We acknowledge the lack of data among patients above 15 years in our cohort, as the majority of them were admitted to adult wards. The retrospective nature of our study limits any meaningful comparison between the steroid and aspirin groups. In those with tricuspid valve involvement, we have not standardised an echocardiogram protocol to look for associated pulmonary hypertension and these data are thus lacking.
Conclusion
Our data are comparable with international data in proving that acute rheumatic fever has a higher prevalence in areas of socio-economic disadvantage. We had a higher number of patients presenting with severe carditis, suggesting that there is a significant cohort of patients with mild to moderate disease that remain undiagnosed. This highlights the need for additional resources and funding for prevention as well as diagnosis of acute rheumatic heart disease. A national registry would be beneficial to manage this disease in endemic areas of the country.
Acknowledgements
We would like to thank Amabel Seow, Loshini Anandaraj, Yashini Mohan, Anna Purani Raju, and Charlotte Gan Ying Shi for their assistance in data collection.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
This study obtained ethical approval from the Medical Research and Ethics Committee of the Malaysian National Institute of Health (NMRR-18-3355-44111).








