Accelerated idioventricular rhythm is defined as an uncommon ectopic rhythm with >3 consecutive premature ventricular beats due to enhanced automaticity of His-Purkinje fibres or myocardium. Although accelerated idioventricular rhythm is a benign arrhythmia, it can sometimes cause some life-threatening arrhythmias.Reference Crosson, Callans and Bradley1–Reference Zhao, Zhou and Cui3 Here, we presented cryoablation of left coronary cusp-originated accelerated idioventricular rhythm degenerating torsades de pointes and resulting in aborted cardiac arrest in a boy.
Case report
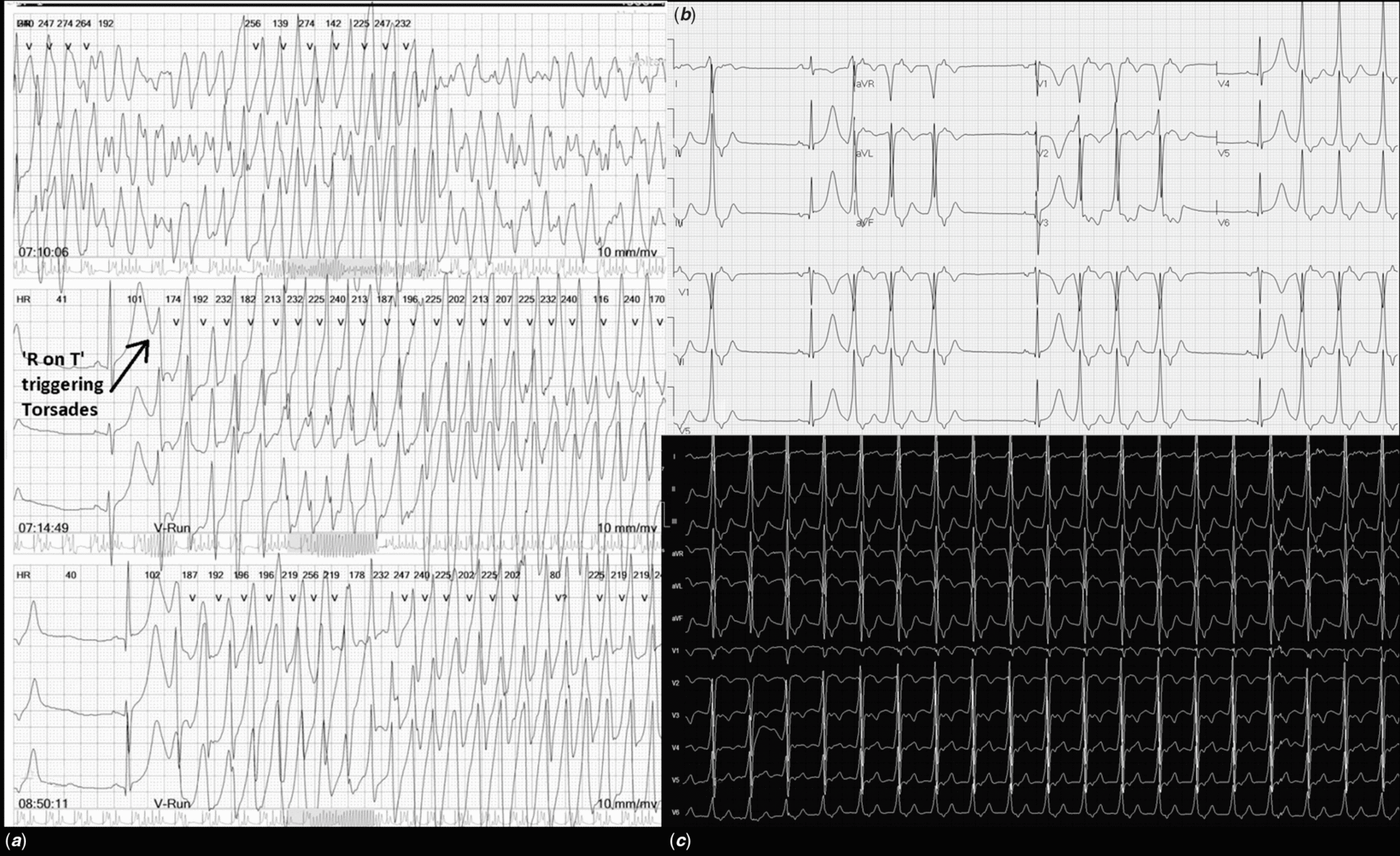
An 11-year-old boy followed up with asymptomatic accelerated idioventricular rhythm for 2 years before was referred to our department for evaluation after a cardiac arrest requiring cardiac resuscitation while asleep. There was no history of drug intake or substance abuse. He had no family history of sudden cardiac death and cardiac arrhythmias. Serum electrolytes and cardiac enzyme levels were in the normal range on admission. The electrocardiogram showed frequent accelerated idioventricular rhythm with a heart rate of 96 bpm. A 24-hour Holter-ECG revealed incessant accelerated idioventricular rhythm, with a median rate of 104 bpm (compared to median sinus rate of 89 bpm), and two torsades de pointes attacks triggered by accelerated idioventricular rhythm-induced “R on T” phenomenon and resulted in syncope and cardiac arrest requiring short resuscitations (Fig 1). The echocardiography showed mild left ventricular dilatation and the fractional shortening of 27.5%.
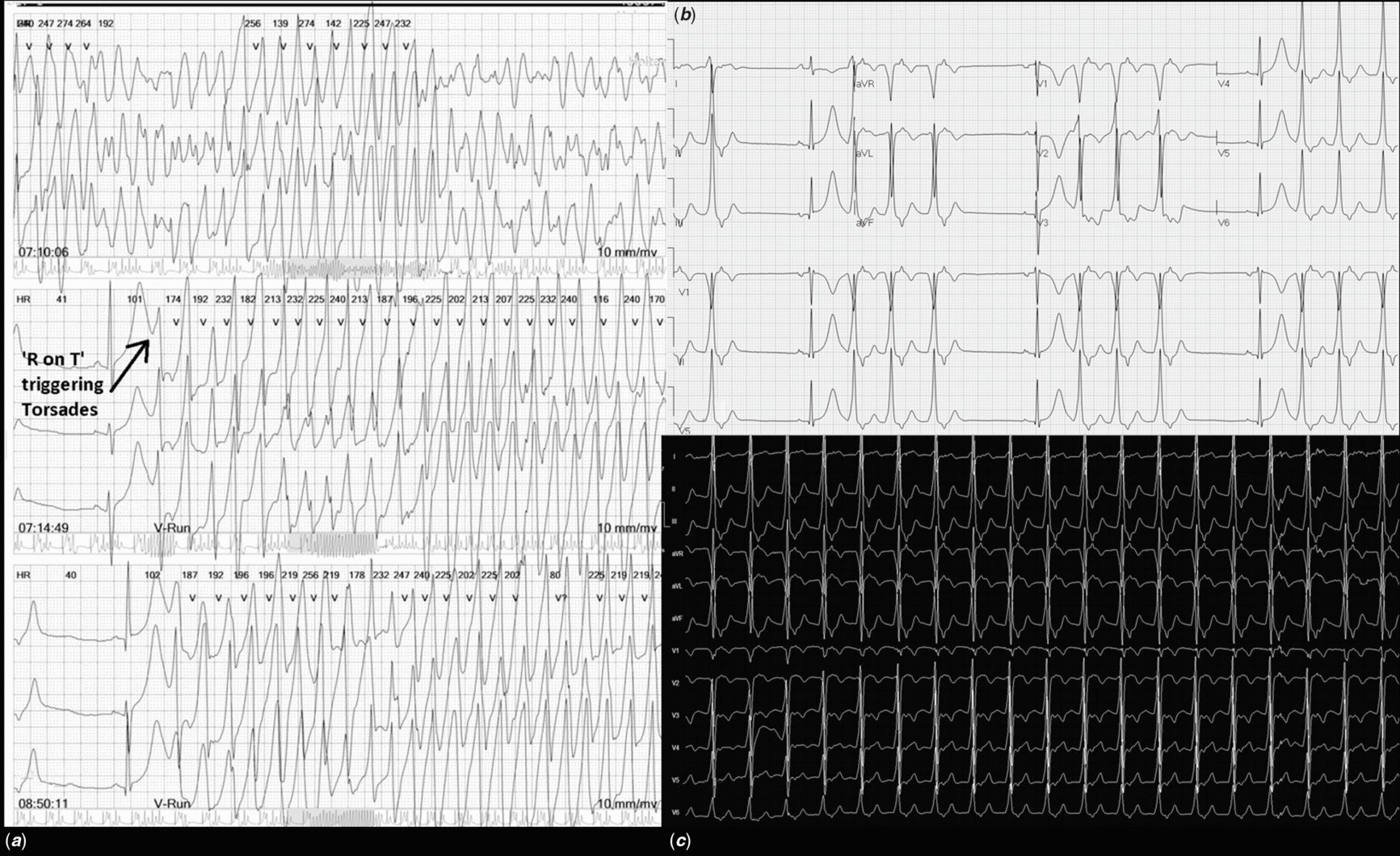
Figure 1. (a) Torsades de points episodes triggered with R on T phenomenon during accelerated idioventricular rhythm (*). (b) Frequent accelerated idioventricular rhythm on the surface electrocardiogram. (c) Incessant accelerated idioventricular rhythm on a 24-hour Holter-ECG, consisting of up to 90% of the whole record. (*the prototypical “short-long” sequence prior to initiation of torsades appears to some extend on the single channel tracing beneath the 3-channel detail).
During the electrophysiological study by EnSite three-dimensional electroanatomic mapping system (St. Jude Medical Inc., St. Paul, Min), the endocardial activation mapping demonstrated a site of early activation originating from the left aortic coronary cusp. Pacemapping at this site showed a complete matching (12/12) with accelerated idioventricular rhythm. Selective left coronary angiography determined a close neighbourhood to the coronary ostium. Therefore, cryoablation of the accelerated idioventricular rhythm with 8-mm-tip cryocatheter (Freezor; Medtronic Inc., Minneapolis, Minnesota, United States of America) was successfully performed (Fig 2). After the procedure, the QT interval of the patient was 470 ms. Three days later, he was discharged without any ectopic beats, with a fractional shortening of 38% and no left ventricular dilatation. On his 1 year of follow-up, he has been still in good condition with no PVC/accelerated idioventricular rhythm and symptom, and normal QT interval as 412 ms.

Figure 2. (a) Three-dimensional anatomy with Ensite Velocity System, showing aortic root and coronary cusps. Blue dots are target lesions for cryoablation in the left coronary sinus, close to the orifice of the left main coronary artery, where the earliest signals were mapped with a −90 ms. Cryocatheter with 8-mm tip is seen as active. (b) Intracardiac electrocardiograms showing the earliest signals at the distal end of the coronary sinus catheter during incessant accelerated idioventricular rhythm, proving a left-sided focus. (c) Fluoroscopy image demonstrating left coronary artery angiogram and the 8-mm cryocatheter tip standing just on the target lesions for ablation. (d) Intracardiac electrograms pointing the time of successful cryoablation with the elimination of the frequent premature ventricular contractions.
Discussion
Most of the literature about paediatric accelerated idioventricular rhythm point to the benign nature, and often idiopathic aetiology,Reference MacLellan-Tobert and Porter4–Reference Wang, Zhu, Hamilton, Kirsh, Stephenson and Gross6 suggesting follow-up without therapy, and even development of specific guides separating this entity from the more malign ventricular tachycardias. In adult studies, accelerated idioventricular rhythm was reported to be related to the reperfusion phase after myocardial infarction, congenital heart disease, and several drugs intoxications such as halothane, cocaine, or digitalis.Reference Crosson, Callans and Bradley1–Reference Zhao, Zhou and Cui3, Reference Chen, Gu and Yang7 Moreover, although rare, it can also be associated with a life-threatening event in the children. Hagel et alReference Hagel, Escudero and Kirsh8 reported a newborn case of accelerated idioventricular rhythm degenerating to a ventricular tachycardia causing hemodynamic deteriorations. Errahmouni et alReference Errahmouni, Bun, Latcu, Tazi-Mezalek and Saoudi2 published a 12-year-old boy with accelerated idioventricular rhythm-induced ventricular tachycardia, left ventricular dysfunction, and cardiogenic shock. Wang et alReference Wang, Zhu, Hamilton, Kirsh, Stephenson and Gross6 reported one infant and one teenage suffered from impairment of left ventricular and reduced right ventricular function, respectively. Similarly, our patient had left ventricular dysfunction probably due to accelerated idioventricular rhythm-induced cardiomyopathy. Torsades de pointes is a variant of polymorphic ventricular tachycardia with the twisting of the QRS morphology around an isoelectric line on the electrocardiogram. If a ventricular ectopic beat occurs over the T wave, defined as an R on T phenomenon, torsades de pointes may begin. In this scenario, torsades de pointes can automatically disappear or can eventually progress into life-threatening ventricular fibrillation if not treated.Reference Childers9 In our case, the QT interval was above the normal range right after the ablation. This prolongation was recovered on follow-up. Celiker et al reported that the increased QT dispersion in the children with accelerated idioventricular rhythm, implying inhomogeneity of myocardial repolarisation and predisposition for arrhythmia, was improved with verapamil treatment. We also think accelerated idioventricular rhythm may have caused some degree of repolarisation disorder leading to the QT prolongation and facilitating the occurrence of torsades de pointes in our patient. To the best of our knowledge, this is the first paediatric case of accelerated idioventricular rhythm-triggered torsades de pointes causing cardiac arrest. Beta-blockers can usually ease clinical symptoms of accelerated idioventricular rhythm. Catheter ablation is also effective in case of accelerated idioventricular rhythm-induced cardiomyopathy.Reference Crosson, Callans and Bradley1, Reference Wang, Zhu, Hamilton, Kirsh, Stephenson and Gross6 The risk of complication during the ablation might be higher in the children, since they do not have a thick cardiac wall and their coronary arteries are usually closer to the endocardial layer. It was reported that the cryoablation had a lower risk of coronary artery damage compared with the radiofrequency ablation.Reference Aras, Topaloglu, Ozeke, Cay, Ozcan and Baser10 In this case, we also performed the cryoablation without complication. After the ablation, torsades de pointes has not recurred on follow-up. In conclusion, this case report shows that accelerated idioventricular rhythm in a child may trigger torsades de pointes, a life-threatening arrhythmia, and cause a cardiac arrest. Cryoablation is a good option for the coronary cusp ablation for an ultimate cure.