Background
Tetralogy of Fallot with absent pulmonary valve syndrome is rare, making up 3–6% of the tetralogy of Fallot spectrum. Patients with absent pulmonary valve syndrome have dysplastic or absent pulmonary valve, free pulmonary regurgitation, and annular stenosis.Reference Yong, Yim and Brizard 1
The right ventricle is hypertrophied and may contain obstructing muscle bands in addition to infundibular narrowing. The pulmonary annulus is mildly to moderately hypoplastic with vestigial nubbins of non-functional myxomatous tissue rather than developed valve leaflets.Reference Saygi, Haydin, Guzeltas, Odemis and Yeniterzi 2
The survival of uncorrected tetralogy of Fallot with the absence of pulmonary valve in young adulthood is uncommon. Typically, these patients present with early-age cyanosis, recurrent respiratory distress and failure to thrive, or heart failure.Reference Drogalis-Kim, Reemtsen and Reardon 3
The aim of this article is to present a case of uncorrected tetralogy of Fallot with absent pulmonary valve in a 37-year-old patient.
Case
A 37-year-old woman with a history of mild dyspnoea at the age of 8 went to the health centre of her community and a heart murmur was detected. After that, the patient had no more further medical attention.
She was hospitalised in a general hospital of her community for ascites, with a large-volume – 7 L of liquid – paracentesis was performed, which had a total protein concentration of 2.8 g/dl and on auscultation a holosystolic murmur was detected, so she was sent to our institution. At her admission, she reported having dyspnoea for 8 years, which progressed in the past 7 months to small efforts, asthenia, adynamia, and loss of 11 kg of weight.
Her examination was remarkable for cachexia, cyanosis, oedema of inferior limbs, and ascites. The pulse rate was 60 beats/minute; blood pressure 110/70 mmHg; and oxygen saturation 87% on room air.
On auscultation, a holosystolic murmur grade III/IV at the left upper sternal border with radiation throughout the thorax was detected and a thrill was palpated. On pulmonary focus, a systolo-diastolic murmur grade IV/IV was heard. Globose abdomen with grade II ascites was found. The remaining electrocardiogram was in the sinus rhythm with a heart rate of 100 beats/minute, and a complete right bundle branch block, bi-auricular enlargement, right ventricular hypertrophy, and premature ventricular beats in duplets are shown in Figure 1. A chest X-ray showed cardiomegaly with cardiothoracic index of 0.58 and enlargement of pulmonary artery. Two-dimensional transthoracic echocardiography demonstrated ventricular septal defect with overriding aorta (Fig 2a), remnant of pulmonary valve with severe pulmonary insufficiency (Fig 2b), and peak systolic gradient of 81 mmHg by continuous Doppler and color flow mapping (Fig 2c and d). Important dilatation of the right cavities and pulmonary artery, severe tricuspid regurgitation, mild right systolic ventricular dysfunction (Fig 2e), mild right ventricular longitudinal systolic dysfunction (Fig 2f) and moderate pericardial effusion was found.

Figure 1 Electrocardiography showing a complete right bundle branch block, bi-auricular enlargement, right ventricular hypertrophy and premature ventricular complexes.
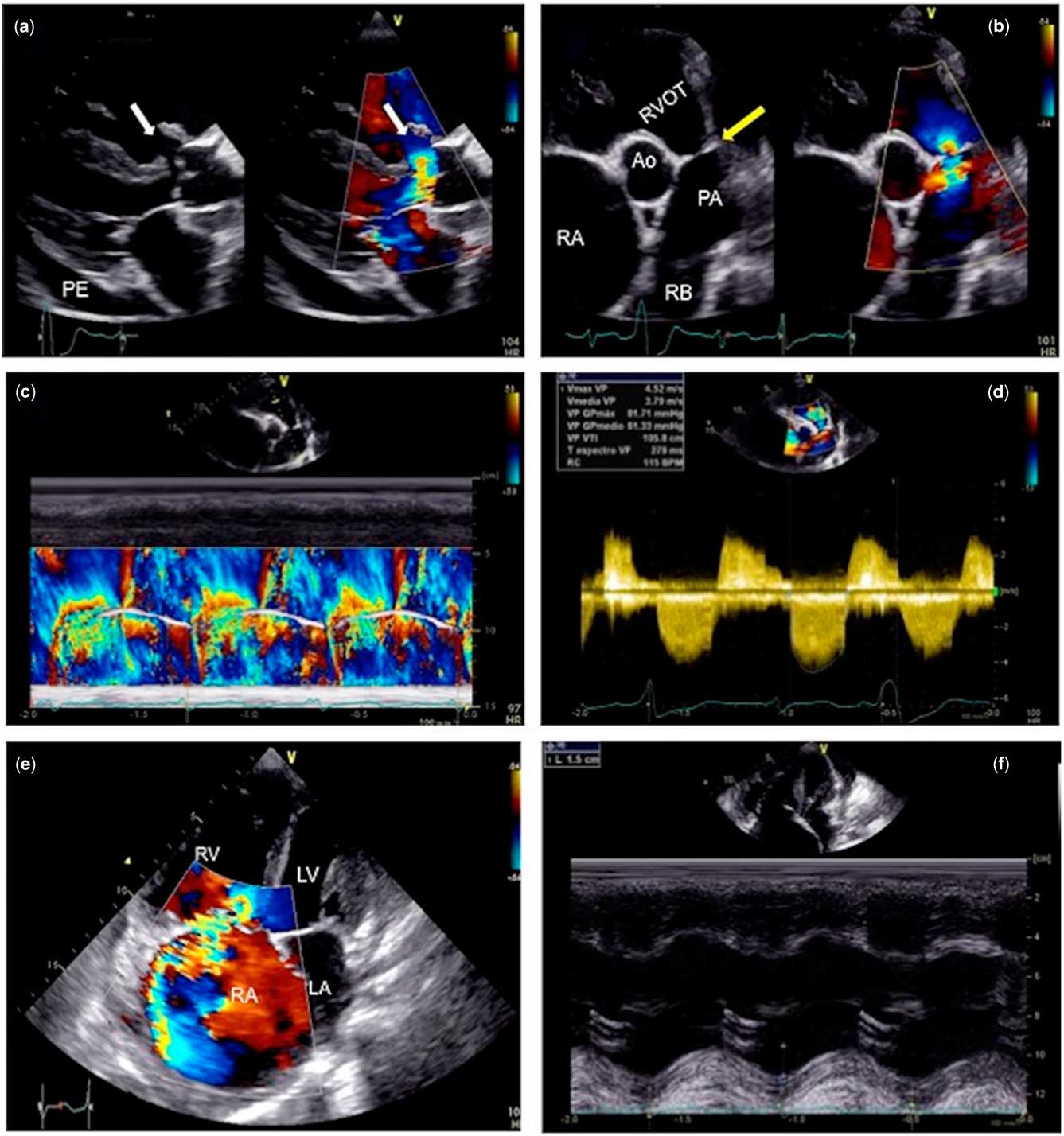
Figure 2 Transthoracic echocardiography. ( a ) Long axis view showing ventricular septal defect with overriding aorta (white arrow) and moderate pericardial effusion. ( b ) Short axis view at the level of great arteries. Remnants of pulmonary valvular tissue are observed and pointed by yellow arrow. The Doppler-color flow shows severe pulmonary insufficiency. ( c ) Color Doppler M-mode showing double pulmonary lesion. ( d ) Continuous Doppler and color flow mapping showing a peak and medium systolic gradient of 81 and 61 mmHg, respectively, and severe pulmonary regurgitation. ( e ) Bidimensional and color-flow four chamber view showing severe dilatation of right cavities and severe tricuspid regurgitation. ( f ) Mild longitudinal systolic dysfunction of the right ventricle is identified in M-mode. Ao=aorta; LA=left atrium; LV=left ventricle; PA=pulmonary artery; RA=right atrium; RB=right branch; RV=right ventricle; RVOT=right ventricular outflow tract.
The patient received treatment with diuretics and ACE-inhibitors with improvement of her NYHA functional class.
Discussion
Tetralogy of Fallot is the most common cause of cyanotic heart disease and may occur at a rate of 1–3 cases/1000 live births. 4 The absence of a functioning pulmonary valve gives rise to pulmonary regurgitation, causing elevated retrograde pressure.
The approach of tension ascites in the emergency room is very common owing to the prevalence of liver abnormalities, but it is important to always perform a complete medical history and physical examination. In this scenario, our patient had a history of heart murmur in childhood and progressive dyspnoea, asthenia, adynamia, and loss of weight in the past 7 months and cardiac ascites related with the congenital heart disease (CHD).
Owing to advances in cardiovascular surgery, an increasing number of patients with cyanotic CHD are surviving longer into adulthood and, consequently, may be at risk for developing liver abnormalities that may significantly influence any future clinical course.Reference Martínez-Quintana, Rodríguez-González, Cabrera-Pérez and Martínez-Martín 5 Decompensated right ventricular or biventricular heart failure causes transmission of elevated right atrial pressure to the liver via the inferior vena cava and hepatic veins. At a cellular level, venous congestion impedes efficient drainage of sinusoidal blood flow into terminal hepatic venules. Sinusoidal stasis results in accumulation of deoxygenated blood, parenchymal atrophy, necrosis, collagen deposition, and, ultimately, fibrosis. 6 Cardiac hepatopathy, which is manifested, among other symptoms, by the formation of ascites, is a well-described entity in both haemodynamic and histologic parameters. Ascites develops as a result of liver sinusoid congestion and subsequent portal hypertension.Reference Christou, Economou, Economou, Kolettis and Tsianos 7
The total protein concentration may also help differentiate ascites associated with cirrhosis from cardiac ascites, both of which have the same serum-albumin gradient (⩾1.1 g/dl), but in the case of ascites associated with cirrhosis the total protein is lower (<2.5 g/dl) than cardiac ascites (⩾2.5 g/dl).Reference Runyon 8 Differential diagnosis is needed for taking decisions of treatment.
Conclusion
This patient had a natural history of tetralogy of Fallot with the absence of pulmonary valve, and developed cardiac ascites.
Actually, she is asymptomatic in medical management with low-dose diuretics and she continues her follow-up in the CHD out-patient clinic.
The echocardiography is a very important tool in the diagnosis and follow-up of CHD.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.





