Acquired brain injury (ABI), from traumatic and non-traumatic causes, is a leading cause of death and disability worldwide (World Health Organization, 2006). Traumatic brain injury (TBI) can result from causes such as falls and motor vehicle collisions whereas non-traumatic brain injury (nTBI) can result from brain tumours and anoxia, for example. Colantonio, Chan, Zagorski, and Parsons (Reference Colantonio, Chan, Zagorski and Parsons2011) reported that from 2003/04 to 2009/10, there were 5,002 older adults (37% of all adults in rehabilitation) with ABI diagnosis codes in in-patient rehabilitation in Ontario. Although the highest rates of TBI have been reported among the older-adult population (Colantonio, Croxford, Farooq, Laporte, & Coyte, Reference Colantonio, Croxford, Farooq, Laporte and Coyte2009; Colantonio et al., Reference Colantonio, Saverino, Zagorski, Swaine, Lewko and Jaglal2010; Faul, Xu, Wald, & Coronado, Reference Faul, Xu, Wald and Coronado2010; Koskinen & Alaranta, Reference Koskinen and Alaranta2008), little research documents the profile and outcomes of in-patient rehabilitation in this rapidly growing population segment. Even less is known about older patients with nTBI. Recent estimates show that approximately 15 per cent of Canada’s population in 2011 comprised adults aged 65 and older (Statistics Canada, 2012a) and is estimated to be approximately 25 per cent by the year 2036 (Statistics Canada, 2012b). However, there is a lack of population-based studies of older adults in rehabilitation despite the likelihood that future consumers of rehabilitation services will increasingly be older adults.
Research on patients in in-patient rehabilitation has frequently used the FIM(TM) Instrument to assess a patient’s physical and cognitive disability (ERABI, 2011). Studies on older adults have found that FIM (total function) scores at admission among TBI patients were in the low to mid-50s, and the FIM scores at discharge were in the low 80s to low 90s (Cifu et al., Reference Cifu, Kreutzer, Marwitz, Rosenthal, Englander and High1996; Frankel et al., Reference Frankel, Marwitz, Cifu, Kreutzer, Englander and Rosenthal2006; Graham et al., Reference Graham, Radice-Neumann, Reistetter, Hammond, Dijkers and Granger2010). However, none of these studies examined the statistical significance of the increase in FIM score from admission to discharge. These scores also reflect the fact that patients are admitted in in-patient rehabilitation after a much briefer length of acute care stay. (e.g., in the United States, the average length of stay in rehabilitation from 2000 to 2007 was 18.7 days) (Granger et al., Reference Granger, Markello, Graham, Deutsch, Reistetter and Ottenbacher2010). Also, some studies have examined the relationship between FIM score and discharge destination. For example, Chang, Ostir, Kuo, Granger, and Ottenbacher (Reference Chang, Ostir, Kuo, Granger and Ottenbacher2008) found that an increase in FIM motor score was associated with increased odds of discharge to home and to assisted living and that an increase in FIM cognitive score was associated with increased likelihood of discharge home. Similarly, Richmond, Kauder, Stumpf, and Meredith (2002) found that while age significantly increased the odds of being discharged to skilled nursing facilities, higher FIM scores significantly lowered the odds of discharge to this destination.
Outside of the older-adult literature, researchers have compared FIM scores between TBI and nTBI patients, but their findings have been inconclusive. Some studies have found that TBI patients have significantly higher FIM scores at admission and discharge and that patients with TBI make significantly higher gains in FIM score over the course of in-patient rehabilitation (Colantonio, Gerber, et al., Reference Colantonio, Chan, Zagorski and Parsons2011; Cullen, Park, & Bayley, Reference Cullen, Park and Bayley2008; Cullen & Weisz, Reference Cullen and Weisz2011). However, another smaller study found no differences between admission and discharge FIM scores and no significant differences in gains in FIM score between these two groups (Cullen, Charmagne, & Bayley, Reference Cullen, Charmagne and Bayley2009). Note that the average age of TBI patients in the aforementioned studies ranged from 34 to 48 years whereas the average age of nTBI (or patients with anoxic brain injury) ranged from 37 to 59 years. Studies focusing on elucidating differences between TBI and nTBI patients in in-patient rehabilitation outcomes can inform planning of types of health care services for older adults in in-patient rehabilitation as well as the education of health care practitioners.
This article addresses the gaps in knowledge of older adults with ABI in in-patient rehabilitation from a population-based perspective. Specifically, in our study we examined the characteristics of older adults aged 65 years and older with ABI admitted to in-patient rehabilitation from acute care and their functional outcomes using FIM scores across different in-patient rehabilitation referral destinations. FIM scores of older adults with TBI and nTBI were compared, as nTBI patients are often treated in similar or identical rehabilitation programs and facilities as those with TBI (Cullen & Weisz, Reference Cullen and Weisz2011).
However, little is known about TBI and nTBI patient profiles, how they differ in terms of functional outcomes, and thus, how the injury affects the use of resources. The comparison between TBI and nTBI is therefore of interest, as it can assist in the evaluation of current rehabilitation practices for patients with TBI and nTBI and can inform program planning for these patients.
Methods
Sample
The cohort included patients aged 65 and older with a TBI or nTBI diagnostic code discharged from acute care to in-patient rehabilitation and subsequently discharged from in-patient rehabilitation between April 1, 2003, and March 31, 2010.
Data Sources and Definition of ABI
All hospitalization data were obtained from the Discharge Abstract Database (DAD), and all in-patient rehabilitation data were obtained from the National Rehabilitation Reporting System (NRS). DAD and NRS data collection is mandatory in the province of Ontario. These data were obtained from the Ministry of Health and Long-Term Care (MOHLTC). Each record in the DAD included demographic and clinical information about all hospital admissions and discharges, including deaths and transfers, using standard diagnosis and procedure and intervention codes. Data quality in the DAD has been assessed using chart re-abstraction and has indicated good agreement for non-clinical variables, moderate to substantial agreement for the most responsible diagnoses (MRDx; the diagnosis most responsible for the acute care length of stay), and good specificity of ABI codes (Juurlink et al., Reference Juurlink, Preyra, Croxford, Chong, Austin and Tu2006). The NRS provides information on clinical outcomes and on the characteristics of various rehabilitation activities. NRS data collection includes data from in-patient rehabilitation units within acute care hospitals and free-standing rehabilitation hospitals. Cases in the NRS are grouped by conditions, referred to as Rehabilitation Client Groupings (RCG) (Canadian Institute for Health Information, 2012). Sensitivity analyses of patients aged 19 and older with ABI indicated that a small proportion was coded as treated in units for stroke (7.9%) and spinal cord or multiple trauma (17.8%). Therefore, we included these cases if they had a previous ABI diagnostic code in acute care.
ABI cases were identified in the DAD by the presence of an International Classification of Disease – Version 10 (ICD-10) code for TBI and nTBI in any of the 25 diagnosis fields. The ICD-10 codes that were used were informed through the international literature and stakeholder consultation (Chen & Colantonio, Reference Chen and Colantonio2011). TBI diagnostic codes included fracture and crushing of the skull and facial bones (S02.0, S02.1, S02.3, S02.7, S02.8, S02.9, S07.1), intracranial injury, excluding those with skull fracture (S06.0, S06.1, S06.2, S06.3, S06.4, S06.5, S06.6, S06.7, S06.8, S06.9), and late effects of injuries (F07.2, T90.2, T90.5). NTBI diagnostic codes included anoxia (G93.1, T71, T75.1, R09.0), brain tumours (C70, C71, C79.3, C79.4, D32.0, D33.0, D33.1, D33.2, D33.3, D42.0, D43, D43.2, G06.0, G06.1, G06.2, G07, G93.0), encephalitis (A81.1, A83.0, A83.2, A86.0, B00.4, B01.1, B02.0, B05.0, B94.1, G04.0, G04.2, G04.8, G04.9, G05, G09), meningitis (A87, B01.0, B37.5, G00, G01, G02, G03), metabolic encephalopathy (E10.0, E11.0, E13.0, E14.0, E15, G92, G93.4), other brain disorders and infections (G91.0, G91.1, G91.2, G93.2, G93.5, G93.6, G93.8, G93.9, G99.8, R29.1), toxic effects of substances, chiefly non-medical as to source (T40.5, T42.6, T51, T56, T57.0, T57.2, T57.3, T58, T64, T65.0), and vascular insults not captured in other national studies of stroke (I62.0, I62.9). We excluded stroke patients in the nTBI group when it was in the most responsible diagnosis field and anywhere in TBI diagnosis fields.
Variables
Demographic and clinical characteristics that were examined included (a) gender, (b) Charlson Comorbidity Index (CCI) score, (c) length of stay (LOS) in acute care and in in-patient rehabilitation, (d) number of alternate level of care (ALC) days, (e) number of special-care days, and (f) number of previous ABI admissions.
The CCI score was used as an indicator of the healthcare need of patients with ABI (Charlson, Pompei, Ales, & Mackenzie, Reference Charlson, Pompei, Ales and MacKenzie1987). It has been widely accepted as a useful tool for measuring co-morbidity disease and has been shown to have a consistent correlation to in-hospital mortality (Sundararajan et al., Reference Sundararajan, Henderson, Perry, Muggivan, Quan and Ghali2004). LOS in acute care was defined as the number of days between admission and discharge in acute care. LOS in in-patient rehabilitation was defined as the number of days between admission and discharge from in-patient rehabilitation. ALC days are days in which a patient occupies an acute care hospital bed but could be appropriately cared for in a less-intensive setting (Canadian Institute for Health Information, 2009). Special-care days were defined as the cumulative number of days spent in all intensive care units. FIM scores were calculated by summing up all motor and cognitive scores. The absolute FIM change was calculated by subtracting the FIM score at admission from the FIM score at discharge.
In-patient rehabilitation referral destinations were examined using the “referral to” code in the NRS. For the purpose of this study, we categorized referral destinations into three groups: (a) community/home, (b) another in-patient rehabilitation facility or in-patient unit, and (c) residential care. Community/home destinations include private practice; services for ambulatory care, drug dependency, community (including public health and transportation), and legal needs; and educational and home care agencies. Another in-patient rehabilitation facility or in-patient unit included in-patient acute care unit in the same or different facility and rehabilitation unit in the same or different facility. Residential care facilities included long-term care homes, continuing care, and nursing homes.
Analyses
Descriptive analyses were conducted to determine the demographic and clinical characteristics of TBI and nTBI patients. T-tests and chi-square tests were conducted to test for significant differences between TBI and nTBI patients on specific characteristics. T-tests were also conducted to (1) assess for significant differences between TBI and nTBI patients on FIM scores at admission and at discharge from in-patient rehabilitation and on their absolute change in FIM score; (2) determine if significant gains were made at discharge among TBI patients and also nTBI patients; and (3) compare the FIM scores between younger adults (19–64 years) and older adults (65 years and older). All FIM scores were also analyzed by in-patient rehabilitation referral destinations. All analyses were performed using SAS, version 9.2 (SAS Institute, Inc., Cary, NC) software.
Results
Characteristics
From April 1, 2003, to March 31, 2010, there were 1,214 patients with a TBI diagnostic code and 1,530 patients with an nTBI diagnostic code admitted to in-patient rehabilitation from acute care. This represents 40 per cent and 47 per cent respectively of the total number of adults in rehabilitation during this period. Among patients with TBI, 44.7 per cent were female. Approximately 16 per cent had a CCI score of 2 or higher, 65.2 per cent stayed in acute care for 12 days or longer, 60.7 per cent stayed in in-patient rehabilitation for 25 days or longer, 45.6 per cent had at least one ALC day, 42.7 per cent had at least one special-care day, and 22.9 per cent had at least one previous ABI admission. Among patients with nTBI, 46.7 per cent were female. Approximately 43 per cent had a CCI score of 2 or higher, 64.1 per cent stayed in acute care for 12 days or longer, 65.8 per cent stayed in in-patient rehabilitation for 25 days or longer, 42 per cent had at least one ALC day, 39.8 per cent had at least one special-care day, and 24.6 per cent had at least one previous ABI admission (see Table 1).
Table 1: Characteristics of TBI and nTBI patients discharged from in-patient rehabilitation from acute care, 2003/04 to 2009/10
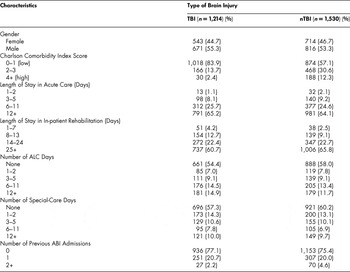
ABI = acquired brain injury
ALC = alternate level of care
nTBI = non-traumatic brain injury
TBI = traumatic brain injury
Results showed that TBI patients (mean age = 77.2, SD = 7.0) were significantly older (p < .001) than nTBI patients (mean age = 75.5, SD = 6.8). Chi-square tests revealed that significantly more nTBI patients had a CCI score of 2 or higher (p < .0001) and stayed in in-patient rehabilitation for at least 25 days (p < .01) (see Table 2). Univariate odds ratios indicated that nTBI patients were 3.90 times more likely than TBI patients to have a CCI score of 2 or higher, and nTBI patients were 1.24 times more likely than TBI patients to have stayed in in-patient rehabilitation for 25 days or longer.
Table 2: Chi-square tests of select demographic and clinical characteristics by type of brain injury

ALC = alternate level of care
FIM = total function
nTBI = non-traumatic brain injury
SD = standard deviation
TBI = traumatic brain injury
FIM Scores
From 2003/04 to 2009/10, the average FIM score at discharge (99.9, SD = 21.1) among TBI patients was significantly higher (p < .0001) than the score at admission (77.8, SD = 22.1). Among patients referred to the community/home, the average score at discharge (105.5, SD = 15.0) was also significantly higher (p < .0001) than the score at admission (81.3, SD = 20.7). Similarly, the discharge FIM among patients referred to another in-patient rehabilitation unit or another in-patient unit (74.4, SD = 27.9) was significantly higher (p < .01) than the admission FIM (64.6, SD = 22.7). The discharge FIM among patients referred to residential care (82.7, SD = 25.0) was also significantly higher (p < .0001) than the admission FIM (66.3, SD = 21.4) (see Table 3).
Table 3: Comparison of FIM score among TBI and nTBI patients at admission and at discharge by in-patient rehabilitation referral destination

FIM = total function
SD = standard deviation
From 2003/04 to 2009/10, the overall average FIM score at discharge (95.9, SD = 23.6) among nTBI patients was significantly higher (p < .0001) than the score at admission (73.7, SD = 22.6). Among patients referred to the community/home, the average score at discharge (102.4, SD = 17.9) was also significantly higher (p < .0001) than the score at admission (77.7, SD = 20.7). Similarly, the discharge FIM among patients referred to another in-patient rehabilitation unit or another in-patient unit (65.7, SD = 24.8) was significantly higher (p < .01) than the admission FIM (58.2, SD = 21.0). The discharge FIM among patients referred to residential care (77.1, SD = 24.7) was also significantly higher (p < .0001) than the admission FIM (61.7, SD = 21.7) (see Table 3).
T-tests revealed that TBI patients had a significantly higher overall FIM at admission compared to nTBI patients (p < .001) and across all referral destinations (community/home = p < .001, another in-patient rehabilitation unit or another in-patient unit = p < .05, and residential care = p < .05). Similarly, TBI patients had a significantly higher overall discharge FIM compared to nTBI patients (p < .0001) and across all referral destinations (community/home = p < .0001, another in-patient rehabilitation unit or another in-patient unit = p < .05, residential care = p < .05). While both TBI and nTBI patients made significant gains in FIM from admission to discharge (see Table 3), a comparison of absolute change in FIM among these two groups across all referral discharge destinations revealed that the gains made were not significantly different (see Table 2).
FIM scores of older and younger adults aged 19 to 64 were also compared. Among patients with TBI, overall FIM scores at admission (p < .0001) and at discharge (p < .0001) were significantly higher among younger adults. However, scores at admission (p < .001) and at discharge (p < .05) among older adults discharged to residential care were significantly higher than the score of younger adults discharged to this destination. Although the absolute change in overall FIM score was significantly different among younger and older adults (p < .05), the absolute change among patients discharged home and to residential care were not significantly different (p = 0.1680 and p = 0.2994 respectively) (see Table 4).
Table 4: Comparison of FIM scores between younger adults (19–64 years) and older adults (65+ years)

FIM = total function
TBI = traumatic brain injury
SD = standard deviation
Among patients with nTBI, overall FIM score at admission (p < .0001) and at discharge (p < .0001) were significantly higher among younger adults. T-tests showed that the overall absolute change in FIM score was not significant (p = 0.6192). The absolute change in FIM score among patients discharged home and to residential care were also not significantly different (p = 0.1131 and p = 0.8709 respectively) (see Table 4).
Discussion
This is the first study, to our knowledge, to compare the functional outcome of older adults (aged 65 and older) with TBI and nTBI in in-patient rehabilitation with a previous acute care admission from a publicly insured sample using the FIM(TM) Instrument. This study demonstrated that both TBI and nTBI patients made significant gains in FIM in in-patient rehabilitation overall and across different in-patient rehabilitation referral destinations. There is a paucity of studies on older adults with nTBI; accordingly, only studies outside of the older-adult literature have been found to compare FIM of TBI and nTBI patients at admission and at discharge. Consistent with these findings (Cullen et al., Reference Cullen, Park and Bayley2008; Cullen & Weisz, Reference Cullen and Weisz2011), this study revealed that TBI patients had significantly higher FIM scores at both admission and at discharge, and this was true across all referral destinations. Finally, studies outside the older-adult literature comparing the FIM gain between TBI and nTBI patients have been inconclusive. Findings from this study showed that the FIM gain between older adults with TBI and nTBI was not significantly different, suggesting that both groups of patients made similar gains in in-patient rehabilitation and that significant differences in FIM score may be due to differences in characteristics intrinsic to TBI or nTBI patients.
Significantly more nTBI patients had higher CCI scores and longer lengths of stay in in-patient rehabilitation, suggesting that nTBI patients had more severe co-morbidities and that their diagnosis was more severe (longer lengths of stay is an indicator of the severity of condition) (Canadian Institute for Health Information, 2009; Newgard et al., Reference Newgard, Fleischman, Choo, Ma, Hedges and McConnell2010). However, other factors such as the lack of rehabilitation services specifically for nTBI patients or the underlying cause of brain injury itself may also play a role in the differences between TBI and nTBI patients in FIM scores at admission and discharge. As such, additional research is required to determine the cause of the differences between these two groups of patients. Our analysis also informs what clinical staff can likely expect in treating a broader range of brain injury patients and how to prepare accordingly – for more medically complex patients for instance. In particular, our work suggests that nTBI patients enter in-patient rehabilitation with lower functional status overall and with more severe comorbidities.
Findings on FIM scores by discharge destination revealed that older adults with TBI and nTBI made significant gains in FIM scores regardless of their subsequent referral destination at discharge from in-patient rehabilitation. Thus, targeted ABI services for older adults discharged to non-home settings are important, as they may provide these patients with an opportunity to continue to improve. Moreover, the work described in this article provides health care professionals working in in-patient rehabilitation and subsequent referral destinations with an idea of the functional status of the patients they can expect to see in their health care setting. For example, health care providers in other in-patient rehabilitation units can expect to see older adults with lower discharge FIM scores.
Of particular importance is that even though younger adults with TBI and nTBI who were discharged home from in-patient rehabilitation had significantly higher FIM scores at admission and at discharge compared to older adults discharged home, the absolute change in FIM score was not significantly different, suggesting that these patients make similar gains in rehabilitation. This finding provides support for the referral of older adults to in-patient rehabilitation.
Our study utilized data from the Ontario ABI Dataset, which captures information on both traumatic and non-traumatic brain injury across the entire population. The National Rehabilitation Reporting System (NRS) data used to capture in-patient rehabilitation is not based exclusively on data from large rehabilitation hospitals but also includes data from rehabilitation units within acute care hospitals. Thus, the NRS includes information on every rehabilitation bed in the province of Ontario including both free-standing centres and rehabilitation beds in acute care settings. Also, older adults included in our study were those who were discharged to in-patient rehabilitation from acute care. This distinction is important because in-patient rehabilitation data captured in the NRS use Rehabilitation Client Groupings (RCGs). RCG 2 identifies patients with brain dysfunction, which includes traumatic and non-traumatic brain injury. However, sensitivity analyses showed that these patients are also captured in other diagnoses such as stroke, spinal cord dysfunction, or major multiple trauma. Therefore, if only RCG 2 were used to identify our sample in the NRS, some patients could be missed. By identifying cases according to patients that had an acute care stay in in-patient rehabilitation, we are more likely to capture all ABI patients within our years of study. Finally, because Ontario accounts for 40 per cent of all Canadians (Statistics Canada, 2012c), findings from this study are highly generalizable and can inform other provinces in Canada.
However, limitations associated with the use of administrative data must be recognized. Although patients with nTBI were significantly older than TBI patients in this study, the sample size is large. This difference is thus unlikely to be clinically significant. Also, we used a relatively conservative definition of TBI compared to other studies (Faul et al., Reference Faul, Xu, Wald and Coronado2010); therefore, comparisons to the international literature should be made with this in mind. There is, however, no international consensus on the definition of both TBI and nTBI using ICD codes, which makes cross-study comparisons difficult. It is acknowledged that patients discharged to in-patient rehabilitation in this sample are likely those who are considered to most benefit from in-patient rehabilitation by clinicians and, thus, are potentially a select group of older patients. Finally, differences in FIM scores at admission and discharge between TBI and nTBI are smaller than the standard deviation of FIM scores among TBI and nTBI patients. Accordingly, it is acknowledged that the TBI and nTBI patients in this study are a diverse group.
Nonetheless, this study provided evidence to suggest that older age should not be a barrier to accessing in-patient rehabilitation services for patients with ABI, as they have the potential to achieve significant changes in functional status. This is supported by the finding that older and younger adults discharged home from rehabilitation make similar gains, despite younger adults having significantly higher FIM scores at admission and at discharge. Older adults are the fastest growing segment of the population, and they should be considered candidates for in-patient rehabilitation on the basis of this evidence. Also, research into understanding why nTBI patients have significantly lower FIM scores should be conducted, and rehabilitation services for patients with brain injury should take into account these differences in order to provide the best service possible for patients with TBI and nTBI. Finally, research specific to older adults is important and can inform the need for capacity of rehabilitation services for this age group.






