Introduction
Social anxiety disorder (SAD) is characterised by persistent fear of social situations and of negative evaluation by others. It is a common disorder with a lifetime prevalence reported to be 11% (Kessler et al., Reference Kessler, Petukhova, Sampson, Zaslavsky and Wittchen2012). It usually develops in early adolescence, but is not uncommon in childhood (Kessler, Reference Kessler2003). SAD is also a particularly persistent and treatment-resistant anxiety disorder (e.g. Kodal et al., Reference Kodal, Fjermestad, Bjelland, Gjestad, Öst, Bjaastad and Wergeland2018) and often precedes other psychiatric conditions such as depression (Beesdo et al., Reference Beesdo, Bittner, Pine, Stein, Höfler, Lieb and Wittchen2007). Therefore, research has focused on understanding mechanisms underlying the disorder. To date, the majority of SAD studies have investigated the condition in adult populations.
The most influential models of SAD in adults have been developed by Clark and Wells (Reference Clark, Wells, Heimberg, Liebowitz, Hope and Schneier1995) and Rapee and Heimberg (Reference Rapee and Heimberg1997). Both have received considerable empirical support (e.g. McManus et al., Reference McManus, Sacadura and Clark2008). Overall, both models propose that SAD is maintained by an interaction between cognitive biases and maladaptive coping strategies. Cognitive biases include dysfunctional assumptions and beliefs about the world and self as a social being (Clark and Wells, Reference Clark, Wells, Heimberg, Liebowitz, Hope and Schneier1995). Maladaptive behavioural and cognitive-coping strategies strengthen social fears and prevent cognitive biases from being disconfirmed (Clark and Wells, Reference Clark, Wells, Heimberg, Liebowitz, Hope and Schneier1995; Rapee and Heimberg, Reference Rapee and Heimberg1997). Cognitive coping strategies include threat monitoring, i.e. paying attention to internal signals of anxiety in search of indicators of threat or poor social performance, as well as negative anticipatory and post-event processing. Prior to social events individuals with SAD will engage in negative anticipatory processing to prepare mentally for how to prevent and handle such feared scenarios. Following the social event, they will review it and ruminate about their performance and the meaning of social feedback cues. Negative anticipatory processing and post-event processing thereby justify the social fears by confirming negative mental self-representations, and by linking a socially anxious past to a socially anxious future (Heimberg et al., Reference Heimberg, Brozovich and Rapee2010).
A different approach to understanding the psychopathology of SAD is found in the metacognitive model. This model holds that emotional disorders are rooted in dysfunctional metacognitions, rather than negative thoughts themselves (Wells, Reference Wells2011). Metacognitions include positive and negative beliefs about worry, cognitive self-consciousness, a need for cognitive control, and a lack of confidence in own memory (Cartwright-Hatton and Wells, Reference Cartwright-Hatton and Wells1997). Although originally developed for understanding generalised anxiety disorder (GAD; Wells, Reference Wells1995), the metacognitive model may be applicable to other emotional disorders, including SAD (Fisak and Hammond, Reference Fisak and Hammond2013; Nordahl and Wells, Reference Nordahl and Wells2017). The model posits that all individuals hold positive metacognitive beliefs, whereas negative metacognitive beliefs distinguish individuals with pathological anxiety from those with no pathology (Wells, Reference Wells2011). Some studies, however, also find that positive metacognitions predict levels of worry (e.g. Spada et al., Reference Spada, Caselli, Manfredi, Rebecchi, Rovetto, Ruggiero and Sassaroli2012), suggesting that the role of positive metacognitions is ambiguous.
Although the mentioned cognitive models primarily focus on negative thoughts of a social nature, or negative metacognitive beliefs as maintaining mechanisms, it has also been suggested that positive cognitions may be significant for mental health (Beck and Haigh, Reference Beck and Haigh2014).
In general, the understanding of SAD in youth is inferior to that of our knowledge about adult individuals. Only recently have researchers begun to examine if models similar to those applied to adults may be applicable to adolescents and children (Halldorsson and Creswell, Reference Halldorsson and Creswell2017). Halldorsson and Creswell (Reference Halldorsson and Creswell2017) created a model of SAD in young people, which incorporates both Clark and Wells’ (Reference Clark, Wells, Heimberg, Liebowitz, Hope and Schneier1995) and Rapee and Heimberg’s (Reference Rapee and Heimberg1997) models. In this model, perceived social danger is a central maintenance mechanism. If the model applies to children, then social threat perception biases must contribute to the maintenance of social anxiety in children. Supporting the model, Muris et al. (Reference Muris, Merckelbach and Damsma2000) found that socially anxious children interpreted social stories as more scary than non-socially anxious children. Furthermore, negative automatic thoughts (NATs) have also been associated with social anxiety in youth (Calvete et al., Reference Calvete, Orue and Hankin2013). Specific associations between socially threatening NATs and SAD symptoms have been found in children (Niekerk et al., Reference Niekerk, van, Klein, Dam, Hudson, Rinck, Hutschemaekers and Becker2017), suggesting that perceived social danger also contributes to maintaining SAD in children. Thus, there is some evidence for a link between social threat NATs and social anxiety in children.
Studies of childhood samples examining other aspects of the models, such as negative anticipatory processing and post-event processing of social events, suggest that these may be involved in maintaining SAD in children (Schmitz et al., Reference Schmitz, Krämer and Tuschen-Caffier2011; Vassilopoulos et al., Reference Vassilopoulos, Moberly and Tsoumanis2014) with negative anticipatory processing and post-event processing correlating strongly with each other (Vassilopoulos et al., Reference Vassilopoulos, Brouzos, Moberly, Tsorbatzoudis and Tziouma2017a; Vassilopoulos et al., Reference Vassilopoulos, Brouzos, Tsorbatzoudis and Tziouma2017b). Overall, Halldorsson and Creswell’s (Reference Halldorsson and Creswell2017) review on SAD in children concluded that negative anticipatory processing and post-event processing may, however, not be disorder-specific mechanisms of childhood SAD. Rather it has been suggested that the thinking pattern of repetitive negative thinking (RNT) may underlie the more content-specific worry about social interactions (Ehring et al., Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011), for example when the person engages in negative anticipatory processing or post-event processing of social events. Negative anticipatory processing and post-event processing may thus be regarded as part of worry, a cognitive process that has been found to predict both SAD and GAD in youth (Hearn et al., Reference Hearn, Donovan, Spence and March2018). Although excessive worry constitutes the core symptom of GAD, it has also been suggested that it maintains SAD in young people (Hearn et al., Reference Hearn, Donovan, Spence and March2018). Although it has been found that children engage in RNT (Bijttebier et al., Reference Bijttebier, Raes, Vasey, Bastin and Ehring2015), the role of this thinking style as a potential maintenance mechanism of childhood SAD is largely unexplored. One study, however, investigated the prediction of SAD and depressive symptoms in adolescents based on RNT as a transdiagnostic factor, compared with worry or rumination as separate predictors of SAD or depressive symptoms in a large group of adolescents. RNT was found to provide a better model fit in predicting SAD and depressive symptoms than a model including worry or rumination as separate predictors (Klemanski et al., Reference Klemanski, Curtiss, McLaughlin and Nolen-Hoeksema2017).
In terms of the content of post-event processing, one study revealed that children with SAD reported more negative and less positive post-event processing than non-anxious children (Schmitz et al., Reference Schmitz, Krämer, Blechert and Tuschen-Caffier2010). This could potentially reflect a tendency for reduced positive thinking in children with SAD and more worry. A second study of children with high and low levels of social anxiety symptoms, however, did not differ with relation to positive post-event processing (Schmitz et al., Reference Schmitz, Krämer and Tuschen-Caffier2011). Yet another research group has found that anxious youths reported less positive automatic thoughts (PATs) than non-anxious youths (Hogendoorn et al., Reference Hogendoorn, Prins, Vervoort, Wolters, Nauta, Hartman and Boer2012), and increases in PATs preceded decreases in anxiety symptoms in anxious youths undergoing CBT (Hogendoorn et al., Reference Hogendoorn, Prins, Boer, Vervoort, Wolters, Moorlag and de Haan2014). Nonetheless, in terms of a potential link between less positive thinking and SAD, Stallard (Reference Stallard2014) argues that at present there is insufficient evidence to claim that anxious children have fewer positive thoughts than non-anxious children. Thus, investigations of the role of positive cognitions in relation to childhood SAD are still warranted.
Similarly, more knowledge about the role of metacognitions in young people is needed. Several studies suggest that clinically anxious youths report higher levels of metacognitions than non-anxious youths, regardless of anxiety disorder (Ellis and Hudson, Reference Ellis and Hudson2011; Lønfeldt et al., Reference Lønfeldt, Silverman and Esbjørn2017). In line with this, Hearn and colleagues (Reference Hearn, Donovan, Spence, March and Holmes2017) found that negative beliefs about worry were linked to social anxiety symptoms, severity and functioning in anxious youth. However, Hearn et al. (Reference Hearn, Donovan, Spence, March and Holmes2017) also reported that children with SAD without co-morbid GAD and children with GAD without co-morbid SAD did not differ significantly in the level of negative beliefs about worry. However, a small sample size and the exclusion of children with co-morbid SAD and GAD, despite this co-morbidity being common, may limit the generalisability of these findings. Overall, the scarcity of studies within this area suggests that the role of metacognitions in SAD in children requires further examination.
The present study aims to contribute to the understanding of maintenance mechanisms of childhood SAD by investigating the relative contribution of social threat NATs, PATs, RNT, negative and positive metacognitions in a clinical child sample presenting with different types of anxiety disorders. Based on theory and existing studies, we propose four hypotheses. First, we hypothesise that a higher degree of social threat NATs, repetitive negative thinking, and negative metacognitions will be associated with higher levels of social anxiety symptoms in clinically anxious children. Second, we hypothesise that children with a SAD diagnosis will experience more social threat NATs than anxious children without SAD, but that there will be no differences regarding repetitive negative thinking or negative metacognitions between groups presenting with different types of anxiety disorders. Third, we hypothesise that social threat NATs, repetitive negative thinking and negative metacognitions will independently predict social anxiety symptoms when controlling for age, gender and number of diagnoses. Fourth, we hypothesise that social threat NATs, but not repetitive negative thinking and negative metacognitions, play a specific role in predicting a SAD diagnosis. As present evidence for PATs and positive metacognitions in childhood SAD is scarce, we only explore the role of these potential predictors.
Method
Participants and procedure
Participants were 122 clinically anxious children aged 7 to 13 years (mean = 9.9, SD = 1.8). Of these, 60 (49%) were female. All children fulfilled the criteria for an anxiety diagnosis [SAD, GAD, separation anxiety disorder (SEP), specific phobia (SP)] as their primary disorder. Of these, 33 fulfilled the diagnostic criteria for SAD diagnosis. SAD was the primary diagnosis for nine children (27.2%), the secondary diagnosis for 12 children (36.4%), and 12 children (36.4%) had SAD as their tertiary diagnosis. All children with SAD, and most without SAD, had co-morbid diagnoses (see Table 1). Children with SAD had significantly more diagnoses than children without SAD (medians: 3 and 2, respectively).
Table 1. Sample characteristics

GAD, generalised anxiety disorder; SEP, separation anxiety disorder; SP, specific phobia; SAD, social anxiety disorder; ODD, oppositional defiant disorder; OCD, obsessive compulsive disorder; ADHD, attention deficit/hyperactivity disorder; CD, conduct disorder; PD, panic disorder; PTSD, post-traumatic stress disorder; STD, sleep terror disorder.
The participants were recruited through the Centre for Anxiety (CfA), a specialised clinic and research centre at the University of Copenhagen, to which parents self-referred their child. To participate in the study, children had to have a primary anxiety disorder and an IQ>70. Diagnostic status was assessed using clinical interviews, and questionnaire data were completed digitally at home, using a secure online platform. Only children with SAD as their primary, secondary or tertiary diagnosis, and children with GAD, SEP or SP without SAD were included in the present study. All data were collected between October 2014 and January 2016. Parents gave written, informed consent to participate in the study. Ethical approval for using the data for research at the CfA had been granted by the Institutional Review Board at the University of Copenhagen.
Measures
Anxiety Disorders Interview Schedule for DSM-IV – parent/child version (ADIS-c/p; Silverman and Albano, Reference Silverman and Albano1996)
Diagnostic status was determined using ADIS-c/p, which is a reliable and much used semi-structured diagnostic interview based on diagnostic DSM-IV criteria. Children and parents were interviewed separately by a clinical psychologist or a psychology student who received supervision by trained psychologists throughout the process to ensure reliability. Diagnoses and clinical severity ratings were given for both interviews. Clinical severity ratings ranged from 0 to 8, with a score of 4 or higher indicating a clinical level of difficulties. Composite scores from both interviews were used to determine the children’s diagnostic status. Based on ADIS-c/p, a categorical outcome measure was created. Children who fulfilled the criteria for SAD as their primary, secondary or tertiary diagnosis were categorised as ‘SAD’, whereas children who fulfilled the criteria for any anxiety disorder were categorised as a comparison group. A similar categorisation was conducted for the presence of GAD, SEP and SP who were all compared with children with all other anxiety disorders than the one in question.
Revised Child Anxiety and Depression Scale – Child version (RCADS-c; Chorpita et al., Reference Chorpita, Yim, Moffitt, Umemoto and Francis2000)
The self-report questionnaire measures the frequency of depression and anxiety symptoms based on diagnostic DSM-IV criteria. RCADS-c contains 47 items. It consists of six subscales, measuring symptoms of depression, SEP, GAD, obsessive compulsive disorder, panic disorder and SAD. Responses are given on a 4-point Likert scale ranging from 0 (never) to 3 (always). Subscale scores are calculated by adding scores for each item within the subscale. The sum of scores on all items provides an index of internalising symptoms, ranging from 0 to 141. The Danish version of RCADS-c has demonstrated adequate psychometric properties, including convergent validity and internal reliability for all subscales (Esbjørn et al., Reference Esbjørn, Sømhovd, Turnstedt and Reinholdt-Dunne2012). This version was used in the present study. In the present sample, Cronbach’s α values were .93 for total RCADS scores and .85 for the SAD subscale, indicating good to excellent internal consistency.
Children’s Automatic Thoughts Scale – Negative/Positive (CATS-N/P; Hogendoorn et al., Reference Hogendoorn, Wolters, Vervoort, Prins, Boer, Kooij and de Haan2010)
CATS-N/P is a self-report questionnaire that measures the frequency of positive automatic thoughts (PAT) and four domains of negative automatic thoughts (NAT) in children, namely personal failure, social threat, physical threat and hostility. The subscales measuring social threat NATs (e.g. I look like an idiot) and PATs (e.g. I feel great) were used in the present study. Responses are scored on a 5-point Likert scale ranging from 0 (not at all) to 4 (all the time). Each subscale contains 10 items. Total subscale scores (range 0–40) are calculated by adding responses for all items on a subscale (Hogendoorn et al., Reference Hogendoorn, Wolters, Vervoort, Prins, Boer, Kooij and de Haan2010). Higher scores reflect more positive or negative automatic thoughts, respectively. A Danish version of CATS-N/P was used in this study. Cronbach’s α values for the subscales measuring social threat NATs and PATs were .89 and .88, respectively.
Perseverative Thinking Questionnaire – Child version (PTQ-c; Bijttebier et al., Reference Bijttebier, Raes, Vasey, Bastin and Ehring2015)
PTQ-c is a recently developed self-report scale for measuring content-independent dysfunctional RNT in children. The PTQ-c consists of 15 items. Responses are scored on a 5-point Likert scale ranging from 0 (never) to 4 (almost always). A total RNT index is calculated by adding scores on all items. The PTQ-c has shown excellent internal consistency as well as convergent and divergent validity (Bijttebier et al., Reference Bijttebier, Raes, Vasey, Bastin and Ehring2015). A Danish translation of the English PTQ-c was used in the present study. In the present sample, internal consistency for this scale was excellent (Cronbach’s α = .95).
Metacognitions Questionnaire for Children – 30-item Version (MCQ-C30; Esbjørn et al., Reference Esbjørn, Sømhovd, Holm, Lønfeldt, Bender, Nielsen and Reinholdt-Dunne2013)
This 30-item self-report child questionnaire measures different types of maladaptive metacognitions. It consists of five subscales (positive and negative beliefs about worry, need for cognitive control, cognitive confidence and cognitive self-consciousness). Each item is scored on a scale from 1 (not at all) to 4 (completely). Higher scores indicate more and stronger metacognitions. The Danish version of the MCQ-C30 has demonstrated adequate psychometric properties (Esbjørn et al., Reference Esbjørn, Sømhovd, Holm, Lønfeldt, Bender, Nielsen and Reinholdt-Dunne2013). In the present study, sum scores were calculated for the subscales of positive and negative metacognitive beliefs. Cronbach’s α values for the positive and negative metacognitions subscales were α = .69, and α = .75, respectively.
Data analysis plan
Prior to conducting statistical analyses, the data were explored graphically. Several variables were non-normally distributed, and irremovable outliers were identified. Additionally, the group sizes of children with and without SAD were unequal; therefore, non-parametric statistical analyses using the continuous outcome measure (RCADS-c) were conducted. In line with Fields’ (Reference Fields2015) recommendations, Spearman’s rho was used to investigate correlations between variables, the Mann–Whitney U-test was used to test for group differences between children with and without SAD. Subsequent hierarchical linear regression analyses of the prediction of SAD symptoms as measured by the social anxiety subscale on RCADS were based on bootstrap samples. A series of binary logistic regression analyses was conducted to investigate the specificity of the variables of interest in predicting the presence of a social anxiety diagnosis versus other anxiety diagnoses. First, the model for SAD was run, followed by models predicting the presence of each of the other anxiety disorders. The IBM SPSS Statistics software version 25 (IBM Corporation, 2017) was used to carry out the statistical analyses.
Results
Multiple simple correlation analyses were conducted to explore the degree to which predictor variables were associated with social anxiety symptoms, internalising symptoms, and with each other. As shown in Table 2, Total RCADS scores correlated moderately with RCADS SAD symptoms, social threat NATs, repetitive negative thinking and negative metacognitions, but not with PATs and positive metacognitions. A similar strength in correlation was found between the SAD symptoms and social threat NATs, whereas although significant, the correlations between social anxiety symptoms, repetitive negative thinking and negative metacognitions, were weak. A weak negative association was also found between SAD symptoms and PATs, while positive metacognitions did not significantly correlate with SAD symptoms.
Table 2. Zero-order correlation coefficients (Spearman’s rho) across the total sample

*p < .05; **p < .001. PTQ-C, Perseverative Thinking Questionnaire – Child Version; CATS-N, Children’s Automatic Thoughts Scale – Negative (social threat-subscale only); CATS-P, Children’s Automatic Thoughts Scale – Positive; MCQ-C30-Pos, Metacognitions Questionnaire for Children – 30 item version – positive metacognitions subscale; MCQ-C30-Neg, Metacognitions Questionnaire for Children – 30 item version – negative metacognitions subscale; RCADStotal, Revised Children’s Anxiety and Depression Scale, total score; RCADSsocial, RCADS social phobia subscale.
A series of Mann–Whitney U-tests and chi-squared tests was performed to test for differences in demographic and cognitive variables between anxious children with and without SAD. The groups did not differ significantly in age and gender distribution, but children with SAD had significantly more diagnoses than those without SAD. As expected, the children with SAD reported significantly more SAD symptoms and higher total RCADS scores than children without SAD. Children with SAD also reported significantly more social threat NATs than those without SAD (see Table 3). The groups did not differ in the remaining factors.
Table 3. Differences in anxiety symptomatology, social threat NATs, PATs, RNT and metacognitions between children with SAD and other anxiety disorders
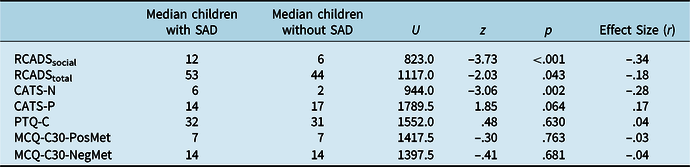
Medians and results based on Mann–Whitney U-test statistics. PTQ-C, Perseverative Thinking Questionnaire – Child Version; CATS-N, Children’s Automatic Thoughts Scale – Negative (social threat subscale only); CATS-P, Children’s Automatic Thoughts Scale – Positive; MCQ-C30-Pos, Metacognitions Questionnaire for Children – 30 item version – positive metacognitions subscale; MCQ-C30-Neg, Metacognitions Questionnaire for Children – 30 item version – negative metacognitions subscale; RCADStotal, Revised Children’s Anxiety and Depression Scale, total score; RCADSsocial, RCADS social phobia subscale.
A hierarchical multiple linear regression analysis was performed to examine the degree to which the cognitive variables of interest predicted the levels of social anxiety symptoms. Assumptions of multiple regression were tested. Correlation analyses showed that predictors did not correlate highly with each other (all r s values <.9), and all variation inflation factor (VIF) values were <10 (range = 1.01–1.97), suggesting no multi-collinearity. A Durbin–Watson statistic close to 2 (i.e. 1.94) indicated unrelated residuals. Thus, the assumption of independent errors had been satisfied. A regression plot of residuals indicated that the assumption of linearity was met, but there is a possibility that the assumption of homoscedasticity was violated. Due to this, and non-normal distribution of some of the variables in the analysis, confidence intervals and standard errors for regression coefficients were based on bootstrap samples (Fields, Reference Fields2015).
Age, gender and number of diagnoses were entered in step 1 of the regression model. The number of anxiety diagnoses per child was used to control for severity in the present study, as this was found to be significantly higher in children with SAD in the present sample. Social threat NATs was entered into the regression model in step 2. All the remaining predictors (RNT, PATs, negative and positive metacognitions) were entered in the final step. The regression model including all the control variables and predictor variables was statistically significant (F 8,113 = 13.59, p < .001) and accounted for 48.6% of the total variance in SAD symptoms. However, the inclusion of RNT, PATs, negative and positive metacognitions into the model, did not significantly improve it (ΔF 4,113 = .90, p = .5). Taken together, RNT, PATs, negative and positive metacognitions only accounted for an additional 1.6% of the variance in SAD symptoms over and above that of the control variables and social threat NATs. In this final model only social threat NATs was a significant predictor of SAD symptoms (t 114 = 7.96, p < .001), accounting for 36% of the variance (see Table 4).
Table 4. Summary of hierarchical multiple linear regression of demographic and cognitive factors predicting social anxiety symptoms

** p < .01; *** p < .001. NATs, negative automatic thoughts (social threat only); PATs, positive automatic thoughts; RNT, repetitive negative thinking.
A post-hoc power analysis for multiple linear regression analysis was conducted using the statistical software program G*Power 3.1.9.2 for Windows XP (Faul et al., Reference Faul, Erdfelder, Buchner and Lang2009), to examine if the current finding could be due to lack of power in the present study. First, G*Power was used to determine the effect size f 2 (0.95) from R 2 (0.49) of the final regression model. Subsequently, the α-level (.05), total sample size (122) and total number of predictor variables (7) was plotted. The analysis showed that the present study had sufficient power (β error level = 1.00) to detect significant predictors.
We utilised binary logistic regression to test if social threat NATs, PATs, RNT, negative and positive metacognitions were specific predictors of SAD diagnosis. The variables were entered into the model as in the hierarchical regression analysis above (see Table 5). The model was statistically significant, indicating that the predictors as a set reliably distinguished between children with SAD and those with other anxiety disorders (χ2 = 46.7, p < .001, d.f. = 8). Nagelkerke’s R 2 of .46 indicated a moderate relationship between prediction and grouping, and a non-significant value of the Hosmer–Lemeshow test (p = .3) indicated a good overall model fit. Social threat NATs [Exp (B) = .86; 0.95 CI, .78 to .94; p = .001], a higher number of diagnoses [Exp (B) =.268; 0.95 CI, .15 to .49; p < .001], and negative metacognitive beliefs [Exp (B) =1.29; 0.95 CI, 1.03 to 1.62; p = .025] were found to be significant predictors of a SAD diagnosis, and they accounted for 46% of the variance.
Table 5. Summary of a binary logistic regression analysis of demographic and cognitive factors predicting a SAD diagnosis

R² = .461 (Nagelkerke); model χ² (8) = 46.67, p = .000. NATs, negative automatic thoughts (social threat only); PATs, positive automatic thoughts; RNT, repetitive negative thinking.
To test if the variables predicting a diagnosis of a SAD disorder are specific for that particular disorder, a series of logistic regressions were conducted, with the predictor variables entered in the same order as in the SAD model, but with different outcome variables (GAD vs other anxiety disorders, SEP vs other anxiety disorders, and SP vs other anxiety disorders). Repetitive negative thinking was found to add significantly the model of a GAD diagnosis [Exp (B) = .930; 0.95 CI, .88 to .98; p = .011]. However, this was the only significant predictor. The model testing predictors of a SEP diagnosis revealed that none of the cognitive variables was significant. Only younger age [Exp (B) = 1.348, 0.95 CI, 1.06 to 1.72; p = .016], and a higher number of diagnoses [Exp (B) =.455, 0.95 CI, .28 to .73; p = .001] reached significance. The analyses of predictors of a SP diagnosis revealed that lower levels of social threat NATs [Exp (B) = 1.097, 0.95 CI, 1.02 to 1.19; p = .019] reached significance.
Discussion
We set out to investigate the role of social threat NATs, PATs, RNT, negative and positive metacognitions in the maintenance of childhood SAD. As hypothesised, we found that higher levels of social threat NATs, RNT and negative metacognitions correlated significantly with a higher degree of SAD symptoms. We also found a significant correlation between lower levels of PATs and higher levels of SAD symptoms, although positive metacognitions were not associated with anxiety symptoms. In accordance with our hypothesis, social threat NATs were more strongly correlated with SAD symptoms than the other investigated variables. Children with SAD also reported significantly more social threat NATs than anxious children without SAD. This finding was expected as social threat NATs are content-congruent with the core feature of SAD (i.e. fear of negative evaluation). However, our finding is important because studies on maintenance mechanisms of childhood social anxiety often fail to consider any disorder-specificity of such mechanisms (Halldorsson and Creswell, Reference Halldorsson and Creswell2017). In line with a cognitive content-specificity hypothesis, which holds that anxiety disorders differentiate based on cognitive content (Lamberton and Oei, Reference Lamberton and Oei2008), these findings suggest that social threat NATs may be a disorder-specific maintenance mechanism of childhood SAD.
Although there was no difference between children with and without SAD in terms of RNT, the significant correlation between SAD symptoms and RNT is in line with previous studies reporting evidence for negative anticipatory processing and post-event processing as maintaining social anxiety in children (Schmitz et al., Reference Schmitz, Krämer, Blechert and Tuschen-Caffier2010, Reference Schmitz, Krämer and Tuschen-Caffier2011, Vassilopoulos et al., Reference Vassilopoulos, Moberly and Tsoumanis2014). Our finding of a significant correlation between SAD symptoms and negative metacognitions is also in line with previous studies suggesting that metacognitions play a role in social anxiety (Hearn et al., Reference Hearn, Donovan, Spence, March and Holmes2017; Muris et al., Reference Muris, Meesters and Gobel2001; Nordahl and Wells, Reference Nordahl and Wells2017). Although significant correlations may suggest that negative metacognitions and persistent negative thinking may play a maintaining role in SAD symptoms in children, these associations were relatively small.
The linear regression analysis with SAD symptoms as the outcome revealed that only social threat NATs significantly predicted SAD symptoms accounting for approximately one-third of the variance. Assuming that social threat NATs reflect perceived social danger in children, these results corroborate the theoretical assumption that a social threat perception bias is involved in maintaining SAD symptoms in children (Halldorsson and Creswell, Reference Halldorsson and Creswell2017). The findings are also in agreement with theoretical models of SAD in adults (Clark and Wells, Reference Clark, Wells, Heimberg, Liebowitz, Hope and Schneier1995; Rapee and Heimberg, Reference Rapee and Heimberg1997). Previous empirical studies have also reported evidence for a link between automatic social threat thoughts and social anxiety in youths (Calvete et al., Reference Calvete, Orue and Hankin2013; Hodson et al., Reference Hodson, McManus, Clark and Doll2008; Micco and Ehrenreich, Reference Micco and Ehrenreich2009; Niekerk et al., Reference Niekerk, van, Klein, Dam, Hudson, Rinck, Hutschemaekers and Becker2017). Using a validated measure of social threat NATs and a sample of clinically anxious Danish children, our study thereby strengthens previous findings.
In contrast to our hypothesis, RNT and negative metacognitions did not provide significant contributions to the model predicting SAD symptoms. RNT, negative and positive metacognitions and PATs, taken together, explained little more than 1% of the variance in SAD symptoms over and above the control variables and social threat NATs. In our sample, children with SAD had a significantly higher level of internalising symptoms than the anxious children without SAD. Furthermore, the included children had a high degree of co-morbidity, with more than 80% of children with SAD also fulfilling the criteria for GAD. This may have influenced at least part of our findings. For instance, metacognitive theory suggests that negative metacognitions may be linked to severity of emotional disorders which would reduce the predictive power of negative metacognitions in our sample, as the level of emotional distress is high. Our findings that both RNT and negative metacognitions correlated more strongly with total RCADS scores than with SAD symptoms, supports the assumption that both factors may be linked to the severity of emotional disorders rather than SAD specifically. Moreover, both RNT (Bijttebier et al., Reference Bijttebier, Raes, Vasey, Bastin and Ehring2015; Ehring et al., Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) negative and positive metacognitions (Nordahl and Wells, Reference Nordahl and Wells2017; Normann and Morina, Reference Normann and Morina2018) may underlie several emotional disorders. In line with this, a previous study of young people found higher levels of negative beliefs about worry to be associated with both SAD and GAD (Hearn et al., Reference Hearn, Donovan, Spence, March and Holmes2017). Our investigation of the specificity of the control and cognitive variables in predicting the presence of SAD diagnosis versus other anxiety diagnoses rather than SAD symptoms revealed that the number of diagnoses as well as negative metacognitions were significant, alongside social threat NATs. One explanation for these differences may be that social threat NATs and negative metacognitions predict different aspects of the disorder. Social threat NATs may be specific for social anxiety symptoms, whereas the level negative metacognitions are a general predictor of severity level, i.e. that symptoms reach the clinical threshold for a diagnosis.
The repetitive negative thinking pattern, however, but not negative metacognitions was a predictor of GAD. This finding was surprising as a previous review points to the importance of negative metacognitions for GAD (Ellis and Hudson, Reference Ellis and Hudson2010). Furthermore, a previous study of a similar Danish sample of children with GAD reported that they had significantly higher levels of negative metacognitions than children with other anxiety disorders (Esbjørn et al., Reference Esbjørn, Lønfeldt, Nielsen, Reinholdt-Dunne, Sømhovd and Cartwright-Hatton2015). This finding may in part be due to shared variance between negative metacognitions and repetitive negative thinking in our sample. Children who engage in higher levels of repetitive negative thinking may do so as they do not believe that they are capable of stopping the worry process, and vice versa. These types of cognitive processes thereby appear to be general rather than specific for these two disorders. However, our findings suggest that different mechanisms may be enrolled in explaining the symptom levels or presence of a diagnosis, suggesting caution when transferring results from the one to the other.
Finally, our exploration of the role of PATs and positive metacognitions revealed a small negative correlation between SAD symptoms and PATs. However, PATs and positive metacognitions were the only variables that did not correlate significantly with total RCADS scores, suggesting that low levels of PATs and high degrees of positive metacognitions are not a central mechanism of the maintenance of the disorder in children diagnosed with an anxiety disorder.
Results from the present study should be interpreted in light of its limitations. First, as the study is cross-sectional, causality cannot be inferred despite significant effects. Second, this study relied primarily on children’s self-reported questionnaire data, although diagnoses were determined based on both parent and child reports. The use of child report for all predictor variables of interest carries a risk of inflated shared variance between variables. Finally, as the sample consisted of clinically anxious Danish children aged 7–13 years with a high degree of GAD, the results may not generalise to other childhood samples. Future studies could benefit from including both community samples and clinical control samples, when testing the specificity of predictors for social anxiety symptoms and diagnoses. Further studies are needed following a longitudinal sample, with specific measures of negative anticipatory processing and post-event processing before firm conclusions can be drawn regarding the specificity of this process in relation to children with SAD. Future research should therefore investigate maintaining mechanisms of childhood SAD whilst addressing the limitations of existing studies in this field.
In conclusion, our study provides evidence for an association between SAD symptoms in anxious children and social threat NATs, repetitive negative thinking, negative metacognitions, and reduced levels of PATs. Perceived social danger, expressed as social threat NATs, emerged as a particularly central and disorder-specific mechanism in the present study. This corroborates previous studies suggesting that this element of main cognitive maintenance models of SAD in adults may apply to children.
Acknowledgements
We would like to thank all the participating children and families, as well as all staff assisting in data collection and treatment.
Financial support
This research received no specific grant from any funding agency, commercial or not-to-profit sectors.
Conflicts of interest
The authors have no conflicts of interest with respect to this publication.
Ethical statement
The authors have abided by the Ethical Principles of Psychologists and the Code of Ethics.








Comments
No Comments have been published for this article.