Introduction
The high co-morbidity between depressive symptoms and paediatric chronic fatigue syndrome (CFS), or myalgic encephalomyelitis (ME), has long since been recognized (Garralda, Reference Garralda1992; Jordan et al., Reference Jordan, Landis, Downey, Osterman, Thurm and Jason1998). At least 30% of children and young people with CFS/ME also have probable depression (Bould et al., Reference Bould, Collin, Lewis, Rimes and Crawley2013), which is significantly higher than the point prevalence of depression in the healthy adolescent population of between 2 and 5% (Zhou et al., Reference Zhou, Michael, Liu, Del Giovane, Qin and Cohen2014). Rates of depression in children with CFS/ME are also higher than the rates of depression in children with other chronic illnesses, for example cystic fibrosis (Walford et al., Reference Walford, Nelson and McCluskey1993) and migraine (Smith et al., Reference Smith, Martin-Herz, Womack and Marsigan2003).
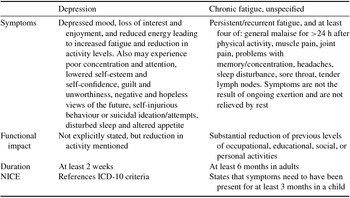
There is diagnostic overlap between depression and CFS/ME. The key diagnostic feature of depression is low mood and/or loss of pleasure in most activities (NICE, 2005). To formally diagnose ‘major depressive disorder’ (APA, 2013), the depressed mood should be significantly different from the individual's baseline functioning, and have lasted for at least 2 weeks, with evidence of clinically significant distress or reduction in functioning. Fatigue is listed in the diagnostic criteria for depression. Paediatric CFS/ME is defined as ‘generalized’ fatigue persisting after routine tests and investigations have failed to identify an obvious underlying ‘cause’ (RCPCH, 2004, p. 28). CFS/ME is characterized by persistent fatigue, which has a significant impact on functioning and is not alleviated by rest; it may be accompanied by joint and muscle pain, headaches, poor concentration, a recurrent sore throat, and flu-like malaise (NICE, 2007). Table 1 provides a comparison of the diagnostic criteria for depression and chronic fatigue syndrome, using the ICD-10 diagnostic criteria published by the World Health Organization (1993).
Table 1. Comparison of ICD-10 diagnostic criteria and NICE
The temporal relationship between low mood/depression and CFS/ME is unclear. Rimes et al. (Reference Rimes, Goodman, Hotopf, Wessely, Meltzer and Chalder2007) reported on four young people who developed CFS/ME, three of whom had at least one psychiatric diagnosis at baseline, and ter Wolbeek et al. (Reference ter Wolbeek, van Doornen, Kavelaars and Heijnen2008) found that fatigue development in adolescent girls at follow-up (4.5 years) was preceded by depressive symptoms at baseline. These studies suggest that depression may temporally predate CFS/ME. However, narrative accounts of young people with CFS/ME who have experienced low mood suggest that it is experienced as resulting from the impact of CFS/ME symptoms on functioning (Taylor et al., Reference Taylor, Loades, Brigden, Collin and Crawley2016).
The combination of low mood and CFS/ME is likely to be detrimental to young people, although the specific consequences are as yet unknown. In adolescents without CFS/ME, experiencing depression is known to increase the likelihood of subsequent depressive episodes, interpersonal difficulties and suicide in adulthood (Fombonne et al., Reference Fombonne, Wostear, Cooper, Harrington and Rutter2001). Although longitudinal studies are lacking, young people with CFS/ME and low mood appear more disabled and experience worse fatigue and more pain than those without depression (Bould et al., Reference Bould, Collin, Lewis, Rimes and Crawley2013). Adults with CFS/ME have a higher risk of completed suicide than the general population, especially in those with a lifetime diagnosis of depression (Roberts et al., Reference Roberts, Wessely, Chalder, Chang and Hotopf2016). The evidence base does not currently enable any conclusions to be drawn about the impact of low mood and depression on recovery from paediatric CFS/ME (Loades et al., Reference Loades, Sheils and Crawley2016). In adults with CFS/ME, depression has been associated with a worse prognosis in some studies (Darbishire et al., Reference Darbishire, Ridsdale and Seed2003; Flo and Chalder, Reference Flo and Chalder2014; Kempke et al., Reference Kempke, Goossens, Luyten, Bekaert, Van Houdenhove and Van Wambeke2010; Tummers et al., Reference Tummers, Knoop, Van Dam and Bleijenberg2013; Wearden et al., Reference Wearden, Dunn, Dowrick and Morriss2012; White and Naish, Reference White and Naish2001), but not in others (Matsuda et al., Reference Matsuda, Matsui, Kataoka, Fukada, Fukuda and Kuratsune2009; Prins et al., Reference Prins, Bleuenberg, Rouweler and Van der Meer2005; Schreurs et al., Reference Schreurs, Veehof, Passade and Vollenbroek-Hutten2011). Furthermore, some CFS/ME treatment approaches may be more favourable for adults with co-morbid depression; a meta-analysis of the effectiveness of CBT and graded exercise therapy (GET) showed no significant difference between the treatments in reducing fatigue and remediating functional impairment, although CBT tended to result in greater reductions in depression than GET.
There are similarities and differences in the treatment approaches for CFS/ME and depression in children and young people. In young people with CFS/ME, there is evidence that CBT is an effective treatment, although at least 20% of children do not get better within 6 months (Chalder et al., Reference Chalder, Deary, Husain and Walwyn2010; Gordon et al., Reference Gordon, Knapman and Lubitz2010; Nijhof et al., Reference Nijhof, Bleijenberg, Uiterwaal, Kimpen and van de Putte2012; Stulemeijer et al., Reference Stulemeijer, de Jong, Fiselier, Hoogveld and Bleijenberg2005). NICE also recommends graded exercise therapy (NICE, 2007). Commensurate with the evidence base, the guidelines for treatment for moderate to severe depression (in the absence of CFS/ME) state that young people should be offered ‘a specific psychological therapy (individual CBT, interpersonal therapy, family therapy or psychodynamic psychotherapy) that runs for at least 3 months’ (NICE, 2015, p. 8). To date, CBT has not proved unequivocally more effective for treating depression in adults than other therapies (Johnsen and Friborg, Reference Johnsen and Friborg2015) and behaviour therapy, for example, may be at least as effective for both adults (Cuijpers et al., Reference Cuijpers, van Straten and Warmerdam2007) and young people (Hetrick et al., Reference Hetrick, Cox, Fisher, Bhar, Rice, Davey and Parker2015).
Thus the commonality between the evidence-based NICE guidelines for CFS/ME (NICE, 2007) and paediatric depression (NICE, 2015) is that both suggest the use of CBT. This article aims to provide a conceptual and clinical review of the similarities and differences between CBT for CFS/ME and CBT for depression in children and young people. Both formulation and intervention will be considered.
CBT for depression
The cognitive model of depression (Beck, Reference Beck1979) posits that depression develops as a result of the activation of negative, unhelpful core beliefs by a precipitating critical incident. These core beliefs are formed as a result of early childhood experiences and pertain to how the individual perceives themselves, others and the world. For example, an experience of critical parenting may lead a child to develop beliefs that they are unlovable and that others are critical. To navigate the world within the constraints of these beliefs, the individual develops a host of dysfunctional assumptions or rules for living (Fennell, Reference Fennell1997) which act as compensatory or protective strategies. The child who believes that they are unlovable may assume that if they can be perfect, then people will love them and not reject them. The precipitating incident is likely to prevent the dysfunctional assumption from being adhered to, therefore activating the negative and unhelpful core belief(s). The core beliefs are reflected in situation specific cognitions, triggered by a range of situations which, through the lens of the core belief, the individual interprets negatively, resulting in negative affect (typically low mood/sadness, but particularly in adolescents, also irritability), unhelpful physiological and cognitive symptoms (e.g. fatigue, anhedonia, lack of concentration) and unhelpful, reinforcing behaviours such as withdrawal from social interactions or from enjoyable and pleasant activities. A vicious cycle of negative thoughts, feelings, behaviours and physiological responses therefore perpetuates the depression, and feedback loops result in the core belief being strengthened (Fig. 1). Thus Beck (Reference Beck1979) postulated that the cognitive symptoms of depression (i.e. depressed thinking) precede the affective symptoms of depression; what is considered central to depression in this model are negative thoughts and beliefs.

Figure 1. Longitudinal formulation of depression (based on Beck, Reference Beck1979)
Based on the Beckian cognitive behavioural model of depression, CBT for depression typically follows a series of stages, although the rate of progress and form that these take varies according to the developmental stage and age of the adolescent (Verduyn et al., Reference Verduyn, Rogers and Wood2009). CBT begins with between one and three sessions of assessment and engagement, including collaborative problem formulation, goal setting, and psychoeducation about depression. The work proceeds to emotional recognition and management, and activity scheduling (approximately sessions 4 to 6). Activity scheduling, or behavioural activation, involves strategically scheduling activities from which an individual gains a sense of mastery, achievement or enjoyment (Veale, Reference Veale2008), thus addressing the behavioural responses that contribute to the maintenance of the depressed mood. At this stage of therapy, the work also includes developing an understanding of the relationship between thoughts, feelings and behaviours. From session 7 onwards, the focus shifts to cognitions, initially through the identification of common thinking biases, and subsequently, through learning to question and test unhelpful thinking (with a focus on hopelessness and helplessness), through Socratic dialogue and behavioural experiments. Problem-solving skills may also be included. Work on beliefs and dysfunctional assumptions may then proceed, with therapy ending with relapse prevention. Therapy would usually last for approximately 16 sessions (Verduyn et al., Reference Verduyn, Rogers and Wood2009), and at least nine sessions of CBT for depression has been shown to be 2.5 times more likely to result in adequate response to treatment (Emslie et al., Reference Emslie, Mayes, Porta, Vitiello, Clarke and Wagner2010).
An alternative cognitive model of depression is the hopelessness theory (Abramson et al., Reference Abramson, Metalsky and Alloy1989), based on Seligman's work on attributions and learned helplessness (Seligman, Reference Seligman1975). When a personally relevant negative event occurs, people who have a depressive attributional style (that is, a tendency to attribute negative life events to internal, stable and global causes) are more likely to develop low mood as a result of their inferential thinking that negative consequences will result from the negative event, and that the negative event occurring means that they are worthless or fundamentally flawed. This attributional style thereby poses a vulnerability for developing depression and serves to maintain it.
In contrast, behavioural models of depression (Lewinsohn and Graf, Reference Lewinsohn and Graf1973) emphasize the maintenance of low mood by the reinforcement of depressive behaviours, and lack of reinforcement of non-depressed behaviours. Vulnerability to developing depression and overcoming depression depend on social skill as well as environmental factors such as the range and availability of events that are potentially reinforcing. Behavioural Activation for Treating Depression (Lejuez et al., Reference Lejuez, Hopko, Acierno, Daughters and Pagoto2011) aims to lift mood and build resilience by increasing an individual's focus on their core values, and linking these to daily activities, which are explicitly planned and scheduled. This has been provisionally trialled in depressed adolescents with good outcomes (Pass et al., Reference Pass, Brisco and Reynolds2015, Reference Pass, Whitney and Reynolds2016).
CBT for CFS/ME
There are a number of cognitive behavioural models of CFS/ME. The cognitive behavioural model of CFS/ME (Browne and Chalder, Reference Browne and Chalder2006; Mackenzie and Wray, Reference Mackenzie and Wray2013) posits that physical factors (e.g. infections), social factors (e.g. lifestyle and stressful life events) and emotional factors (such as personality and mood) may contribute to the development of CFS/ME. The symptoms of CFS/ME, including for example fatigue and muscle pain, result in individuals avoiding activity in an attempt to feel better. Resting more and becoming more unfit through deconditioning can exacerbate symptoms, which, when combined with an increase focus on symptoms, lead to fear of undertaking activity which might exacerbate symptoms, and fears that the symptoms mean the individual is very ill, resulting in further reductions in activity. This can generate feelings of frustration and worry, as well as a sense of helplessness and loss of control, which may result in either over-activity or inactivity as a compensatory strategy, both of which result in a worsening of the symptoms. Wessely's model of CFS/ME postulates that a heightened focus on illness (and physiological symptoms perceived to be related to illness) reinforces an individual's belief that they have an acute and potentially dangerous disease, and as a result, they decrease their activity levels (Butler, Chalder, Ron and Wessely, Reference Butler, Chalder, Ron and Wessely1991). There is increasing evidence in adults that cognitions, such as the interpretation of the meaning of the symptoms and focusing on the symptoms, are associated with symptom severity (Fernie et al., Reference Fernie, Maher‐Edwards, Murphy, Nikčević and Spada2015; Maher-Edwards et al., Reference Maher-Edwards, Fernie, Murphy, Wells and Spada2011, Reference Maher‐Edwards, Fernie, Murphy, Nikcevic and Spada2012) although this research has yet to be extended to adolescent populations. There is also evidence for beliefs about emotions leading to emotional suppression in adults with CFS/ME (Rimes and Chalder, Reference Rimes and Chalder2010; Rimes et al., Reference Rimes, Ashcroft, Bryan and Chalder2016), which could contribute to vulnerability to problem development and to maintenance (Surawy et al., Reference Surawy, Hackmann, Hawton and Sharpe1995). Personality traits such as striving for high standards and neglecting one's own needs as predisposing vulnerability factors have been incorporated into this model (Surawy et al., Reference Surawy, Hackmann, Hawton and Sharpe1995).

Figure 2. Longitudinal formulation of CFS/ME (based on Browne and Chalder, Reference Browne and Chalder2006)
CBT for CFS/ME in adolescents typically consists of a behavioural element, which aims to gradually and consistently increase activity, and a cognitive component, which targets thoughts, assumptions and beliefs about the young person's illness and symptoms (Mackenzie and Wray, Reference Mackenzie and Wray2013). The behavioural component may focus on sleep habits and interventions to promote sleep quality (for example, anchoring the bedtime and wake-up time), as well as monitoring high energy activity and boom-and-bust cycles, aiming to do instead do a consistent amount of high energy activity every day, regardless of symptoms, and gradually increasing this (Browne and Chalder, Reference Browne and Chalder2006). The CBT approaches to CFS/ME in adolescents (Lloyd et al., Reference Lloyd, Chalder and Rimes2012; Nijhof et al., Reference Nijhof, Bleijenberg, Uiterwaal, Kimpen and van de Putte2012) have been predominantly behavioural; the focus is on behavioural change through activity management. Cognitive misinterpretations such as the exploration and challenging of the ‘meaning’ of the symptoms are addressed as and when necessary. This is in contrast to the centrality of cognition in traditional cognitive therapy (Beck, Reference Beck1979). CBT for CFS/ME may, where necessary, include work on anxiety and depression (Lloyd et al., Reference Lloyd, Chalder and Rimes2012), although this is not the predominant focus. Typical duration, based on published studies, varies significantly, from five sessions over 6 months (Kawatani et al., Reference Kawatani, Mizuno, Shiraishi, Takao, Joudoi and Fukuda2011) to 18 sessions (Al-Haggar et al., Reference Al-Haggar, Al-Naggar and Abdel-Salam2006), with European studies providing, for example, 21 interactive internet-delivered modules (Nijhof et al., Reference Nijhof, Bleijenberg, Uiterwaal, Kimpen and van de Putte2012) or 15 hourly face-to-face sessions (Chalder et al., Reference Chalder, Tong and Deary2002).
In adults, various published CBT for CFS/ME treatment protocols have adopted different aims and foci, including cognitive and behavioural elements but placing differing emphasis on these components. For example, in the PACE trial, the CBT package aimed to improve levels of functioning as a primary outcome (Burgess and Chalder, Reference Burgess and Chalder2004). The cognitive component addresses fearful thoughts about activity, fear avoidance beliefs, and perfectionist thoughts and beliefs that feed boom-and-bust cycles. The behavioural component includes activity management and sleep hygiene, as well as graded exposure to anxiety-provoking situations where necessary. In contrast, a Dutch CBT treatment protocol, with the aim of recovery from fatigue, included a prescribed physical activity programme, addressing unhelpful thoughts and beliefs about exercise specifically within this (Knoop and Bleijenberg, Reference Knoop and Bleijenberg2010). It also emphasizes empowering patients, addressing low self-efficacy regarding fatigue, and tackles the role of symptom focus as a maintenance factor (Worm-Smeitink et al., Reference Worm-Smeitink, Nikolaus, Goldsmith, Wiborg, Ali, Knoop and Chalder2016). Although both packages had good outcomes, the Dutch approach was more effective (Worm-Smeitink et al., Reference Worm-Smeitink, Nikolaus, Goldsmith, Wiborg, Ali, Knoop and Chalder2016).
Comparison of CBT treatments
Commonalities
Both CBT for depression (CBT-D) and CBT for CFS/ME (CBT-CFS) share the same underpinning ethos. They are collaborative, working together with the young person and their family as a team, rather than taking an expert–patient stance (Stallard, Reference Stallard2005). Furthermore, the approach is one of empirical discovery; the therapist does not assume that they know the answers, but rather, works with the young person to seek to find out how the world works, for example through testing out an assumption via a behavioural experiment (Fuggle et al., Reference Fuggle, Dunsmuir and Curry2013).
There are further similarities with regard to what the therapist might be expected to do; therapy commences with engagement and alliance building behaviours such as validating feelings, active listening, being nice and expressing care (Baylis et al., Reference Baylis, Collins and Coleman2011), and involves psychoeducation and socialization to the CBT model. Therapy sessions are structured, using an agenda. At the end of each session, between-session tasks are collaboratively developed, emerging from the content of the session, with the aim of helping to generalize and apply learning from therapy in daily life. There is also an emphasis on self-monitoring to enable the young person to recognize patterns in thoughts/feelings/behaviour/physiological symptoms, and to spot triggers for specific difficulties, which would also further inform the shared formulation and enable the identification of treatment targets. Therapeutic work is goal focused (Verduyn et al., Reference Verduyn, Rogers and Wood2009). During therapy, parents are included when it is necessary and/or helpful to do so, and parental involvement may take a variety of forms including the roles of co-therapist or co-client (Stallard, Reference Stallard2005).
Differences
There are a number of differences between CBT-D and CBT-CFS that distinguish the approaches (see Table 2):
-
(1) Formulation of problem development is different, specifically with regard to precipitating factors. In CFS/ME, precipitating factors are assumed to include infections with an immune response, and subsequent physical deconditioning (White et al., Reference White, Thomas, Kangro, Bruce-Jones, Amess and Crawford2001). However, evidence for deconditioning is questionable as CFS/ME patients have been found to be similarly deconditioned to sedentary controls, and a recent mediation analysis showed that in adults, change in fear avoidance beliefs rather than physical function was the strongest mediator of treatment outcome (Chalder et al., Reference Chalder, Goldsmith, White, Sharpe and Pickles2015). Depression tends to be predicted by a combination of significant life events, an emotional personality and past psychiatric history.
-
(2) Therapeutic goals would be expected to be different in CBT-D versus CBT-CFS. In CBT-D, the overarching goal tends to be mood improvement, whilst CBT-CFS aims to remediate fatigue and/or improve functioning. However, commensurate with the collaborative CBT approach, goals are individualized, and therefore could be wide-reaching and overlapping.
-
(3) The impact of activity in CFS/ME is different to what would be expected in depression. Although fatigue and lack of energy are expected in both, fatigue in depression (mental and physical) can be alleviated by activity and exercise, whereas in CFS/ME, excessive physical exertion tends to cause symptom exacerbation, resulting in activities that may previously have been pleasurable and positively reinforcing being experienced as aversive and negatively reinforcing (Taylor et al. Reference Taylor, Loades, Brigden, Collin and Crawley2016).
-
(4) The way in which activity is tackled is different. In CBT-D, the aim is to increase activity early on in therapy with behavioural activation (Verduyn et al., Reference Verduyn, Rogers and Wood2009). This breaks the negative cycle of inactivity and lack of motivation, thereby improving mood. Activity scheduling initially involves monitoring to determine the current activity levels, alongside rating mood. Subsequently, activities that give a sense of enjoyment and/or achievement are purposefully planned and undertaken. In CBT-CFS, the initial focus is also on activity, which is initially monitored, with the emphasis on distinguishing high-energy versus low-energy activities (without necessarily monitoring mood). The activity management approach (Browne and Chalder, Reference Browne and Chalder2006; NICE, 2007) aims to establish a baseline of activities that a young person is able to do every day, by determining the midpoint between what they are able to do on the best day and what they are able to do on the worst day. Once this baseline has been established, the young person would then gradually increase the amount of activity, by approximately 10% every fortnight. This may initially mean reducing the amount of activities they are doing, at least on some days of the week, to achieve a consistent level of activity across days. Activity scheduling (Rimes and Chalder, Reference Rimes and Chalder2015) would focus on planning rests and including a range of different activities in the programme.
-
(5) The cognitive focus of the work is also different. In CBT-D, the focus is on negative automatic thoughts, assumptions and beliefs that would most closely be associated with depression such as negative thoughts about the self, others and the future (Beck, Reference Beck1979), whilst in CBT-CFS, the focus is on negative automatic thoughts, assumptions and beliefs that may be maintaining disability and symptoms, such as fear avoidance beliefs and catastrophic thinking about symptoms and the impact of activity (Rimes et al., Reference Rimes, Wingrove, Moss-Morris and Chalder2014). Consistent with this, in adults, CFS/ME patients have been found to be primarily concerned with their health problems (Hughes et al., Reference Hughes, Hirsch, Chalder and Moss-Morris2016), whereas depressed patients’ cognitions were found to be focused on negative views of themselves (Moss-Morris and Petrie, Reference Moss-Morris and Petrie2001). It is not known to what extent the same trends exist in young people. Furthermore, cognitive biases such as symptom focusing in CFS/ME can be tackled directly with attentional training (Worm-Smeitink et al., Reference Worm-Smeitink, Nikolaus, Goldsmith, Wiborg, Ali, Knoop and Chalder2016), whereas the biases in depression are more typically addressed by noticing, labelling and challenging the thinking patterns in specific situations (Verduyn et al., Reference Verduyn, Rogers and Wood2009).
Table 2. Distinguishing factors of CBT-CFS versus CBT-D

Discussion
Despite differences in the cognitive behavioural models of CFS and depression, primarily the extent to which cognitions are seen as precipitating the problem, there are fundamental underlying similarities with regard to the perpetuation of the difficulties in both models with interactions between cognitions, behaviour, emotions and physiological symptoms serving to reinforce and exacerbate each other. These differences imply that the process of collaborative formulation, whilst similar at maintainence level, would be different in terms of understanding problem onset and vulnerability. Given the significant impact that CFS/ME has on functioning (i.e. behaviour) of young people, incorporating elements of the behavioural model of depression and the impact of the physical illness on reinforcement from the environment could be useful. An added benefit of this approach is that it could help a young person to avoid or challenge internal, global and stable attributions, instead formulating their difficulties as a temporary and understandable consequence of a chronic illness which has a significant impact on their behaviour (activity) in their lives and for which they are not to blame. This important former attributional style has been found to be related to both fatigue and the severity of depression in a community sample of adults (Chalder et al., Reference Chalder, Power and Wessely1996). When working with young people with both depression and CFS/ME, a shared and idiosyncratic formulation approach would seem judicious, drawing on elements of the cognitive and behavioural models and integrating them in a meaningful way (see Fig. 3 for an example).

Figure 3. Proposed maintenance cycle of CFS and low mood incorporating elements of the cognitive behavioural models of CFS/ME, Beckian cognitive model of depression and behavioural models of depression
The current evidence does not allow robust conclusions to be drawn about whether tackling CFS/ME might alleviate depression, or whether a more integrated treatment approach is preferable. No studies have rigorously tested CBT for co-morbid depression in paediatric CFS/ME (Loades et al., Reference Loades, Sheils and Crawley2016), although there are initial indications from a case study (Loades, Reference Loades2015) that good outcomes can be achieved using a formulation-driven approach. Pragmatically, if a young person is low in mood but feels motivated, able to engage in, and hopeful about the outcome of CBT-CFS, then treatment could start with this focus. If the level of depression, and the associated lack of motivation and degree of hopelessness and helplessness is such that it is likely to impact on a young person's ability to engage in CBT-CFS, then it would be important to address both CFS/ME and depression concomitantly. In instances where a young person's depression is overwhelming and includes a significant degree of suicidal ideation, treating the depression and alleviating the risk would be the most judicious course of action, before attempting to treat the CFS/ME.
There are possible ways to integrate the two treatment approaches. For example, in CBT for CFS/ME, high-energy activity would be limited to a certain amount that an individual could manage to do every day, regardless of whether it was a good or bad day. Behaviour activation (CBT-D) could still be utilized by taking account of (1) scheduling high-energy activites that give a sense of enjoyment and/or achievement to fit within this daily limit, and (2) identifying low-energy activites that give a sense of enjoyment and achievement. Focusing on a broader range of negative cognitions than usual in CBT-CFS, beyond those specifically related to illness and activity, would be an important adaptation to incorporate more standard CBT-D thought catching and challenging. Adapting CBT for fatigue, which may well be an issue in depression as well as in CFS/ME, for example by reducing the length of sessions, taking breaks during sessions, more repetition of material and supplementing verbal discussions with written summaries, would also be important. There are overlaps between the Surawy model of CFS and models of depression, and it may be that if core beliefs were more explicitly tackled within a CFS/ME approach, individuals would be less prone to relapse. Mindfulness-based CBT (MBCT), which has good evidence of effectiveness as a treatment for relapsing depression in adults (Piet and Hougaard, Reference Piet and Hougaard2011), has been applied in CFS/ME patients still experiencing excessive fatigue following CBT for CFS (Rimes and Wingrove, Reference Rimes and Wingrove2013). The latter study found that unhelpful beliefs about emotions, catastrophic thinking about fatigue and all-or-nothing thinking patterns improved more in the MBCT group compared with waiting list controls. These factors might reasonably be expected to be more problematic in those CFS/ME patients who are also depressed, and therefore MBCT could make a promising avenue for intervention, but is yet to be applied to young people with CFS/ME.
Conclusion
In this paper, we have argued that CBT is an evidence-based treatment for both CFS/ME and depression in children and young people. There are both similarities in the approaches, but also key differences, such as onset formulation, how activity is managed, and which cognitions are targeted. When working with a young person with depression and CFS/ME, clinicians should take a formulation-driven approach to determining where to intervene, and to approach behavioural activation cautiously, incorporating the principles of a graded activity management programme to circumvent boom-and-bust cycles. It is also important for clinicians to consider broadening their focus on negative cognitions beyound those about activity, physical symptoms and illness, to include more global patterns of negative thinking about the self, others, the world and the future.
Acknowledgements
None.
Financial support: M.L. received research capability funding from the Royal United Hospital in Bath.
Conflicts of interest: Maria Loades and Trudie Chalder have no conflicts of interest with respect to this publication.








Comments
No Comments have been published for this article.