Introduction
Traditionally, repetitive negative thinking (RNT) has been studied in emotional disorders such as depression (e.g. Spasojević and Alloy, Reference Spasojević and Alloy2001) but in recent years there has been increasing interest in this thinking style influencing psychotic experiences such as paranoia (e.g. Simpson, MacGregor, Cavanagh and Dudley, Reference Simpson, MacGregor, Cavanagh and Dudley2012; Freeman et al., Reference Freeman, Dunn, Startup, Pugh, Cordwell and Mander2015). In this paper we report on psychometric properties of a relatively new measure of RNT. This measure was originally developed in non-clinical (internet and university student) groups and clinical groups comprised primarily of mood disorder and eating disorder patients.
The Perseverative Thinking Questionnaire (PTQ; Ehring et al., Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) is a self-report measure of negative ruminative thinking (RNT). It is a “content-free” measure, which includes items such as “my thoughts are not much help to me” and “I keep thinking about the same issues all the time”. This is of note, since previous measures of rumination, such as the Response Style Questionnaire (RSQ; Nolen-Hoeksema and Morrow, Reference Nolen-Hoeksema and Morrow1991) and the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger and Borkovec, Reference Meyer, Miller, Metzger and Borkovec1990) use disorder-specific content in their items (in the case of the RSQ and PSWQ, depressive rumination and Generalized Anxiety Disorder content, respectively, is used). The PSWQ is described here as a measure of rumination as well as worry, since worry is a content-specific form of RNT (Topper, Molenaar, Emmelkamp and Ehring, Reference Topper, Molenaar, Emmelkamp and Ehring2014).
Since RNT is a process that has been demonstrated to underlie a number of different disorders, with key characteristics common between disorders, and only the content showing disorder specificity (Ehring and Watkins, Reference Ehring and Watkins2008), a reliable transdiagnostic measure is a valuable tool for research in this area. The PTQ, with its “content-free” items is a promising candidate, but has yet to be validated in a psychosis sample.
Ehring et al. (Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) developed the PTQ using data from non-clinical, mood disorder, and eating disorder groups. During its development, confirmatory factor analyses found a second-order model structure with three lower-order factors. These are described as “Core characteristics” of RNT (e.g. “The same thought keeps going through my mind again and again”); “Perceived unproductiveness” of RNT (e.g. “I think about many problems without solving any of them”), and “Capturing mental capacity” (e.g. “My thoughts prevent me from focusing on other things”).
When validating the PTQ, Ehring et al. (Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) called for future research to use different carefully diagnosed groups to validate the PTQ. However, to date, the few studies published that use the PTQ have mainly focused on depression or used non-clinical samples. For example, Raes (Reference Raes2012) demonstrated that the PTQ was a significant predictor of depressive symptoms 3 years later in a sample of 81 university students and Teismann et al. (Reference Teismann, von Brachel, Hanning, Grillenberger, Hebermehl and Hornstein2014) found that a group therapy aimed at reducing rumination (as measured by the PTQ) improved depressed mood in patients with residual depressive symptoms. Using non-clinical participant groups, Teismann, Het, Grillenberger, Willutzki and Wolf (Reference Teismann, Het, Grillenberger, Willutzki and Wolf2013) found that writing about life goals reduced ruminative thinking in a general population sample; and Burg and Michalak (Reference Burg and Michalak2011) showed that maintaining mindful contact with the breath was negatively correlated with RNT in undergraduate students. Müller, Teismann, Havemann, Michalak and Seehagen (Reference Müller, Teismann, Havemann, Michalak and Seehagen2013) found that antenatal scores on the PTQ assessed in 66 mothers had predictive value for impaired bonding with, and anxiety about caring for, the child. Vossbeck-Elsebusch, Freisfeld and Ehring (Reference Vossbeck-Elsebusch, Freisfeld and Ehring2014) found a correlation between new mothers’ PTQ scores and their symptoms of post-traumatic stress disorder following childbirth.
Whilst Martinelli, Cavanagh and Dudley (Reference Martinelli, Cavanagh and Dudley2013) have used the PTQ in a non-clinical sample to investigate the role of rumination in the maintenance of non-clinical paranoia, to our knowledge there has been no previous work using the PTQ in a clinical population with psychosis diagnoses. However, patients with current persecutory delusions have already been described as demonstrating clinical levels of rumination (i.e. comparative to scores of Generalised Anxiety Disorder patients) using the ruminative response scale of the Response Styles Questionnaire (Hepworth, Startup and Freeman, Reference Hepworth, Startup and Freeman2011) and worry using the PSWQ (e.g. Freeman, Pugh, Vorontsova, Antley and Slater, Reference Freeman, Pugh, Vorontsova, Antley and Slater2010). This is in keeping with Freeman, Garety, Kuipers, Fowler and Bebbington's (Reference Freeman, Garety, Kuipers, Fowler and Bebbington2002) cognitive model of persecutory delusions, which outlines worry as a key mechanism in the development and maintenance of the delusion. This model has been supported in many studies; most notably, Freeman et al. (Reference Freeman, Dunn, Startup, Pugh, Cordwell and Mander2015) demonstrated in a randomized controlled trial with 150 patients with persistent persecutory delusions that a brief CBT intervention targeting worry (a form of rumination) led to significant reductions in paranoia. A sophisticated mediation analysis showed that two-thirds of the changes in the persecutory delusions were accounted for by changes in worry. Significant changes in RNT as assessed by the PTQ were also found in the trial. This trial provides the strongest demonstration yet of a causal role of worry and paranoia. Using a non-clinical sample, Simpson et al. (Reference Simpson, MacGregor, Cavanagh and Dudley2012) found associations between trait paranoia and rumination in a non-clinical sample. It would therefore be beneficial to validate the structure of the PTQ in this patient group in order to assess whether it may be a reliable and valid measure of RNT for this population.
The current study therefore seeks to validate the PTQ by assessing its factor structure in this clinical population and by using the measure to establish criterion validity in comparison of a population of patients with current persecutory delusions against a sample from the general population. It was also planned to test the PTQ's internal reliability, as well as its convergent validity, with an existing rumination measure frequently used with this population: the PSWQ.
Since the PTQ is intended to be a measure of a transdiagnostic process, we hypothesize that its factor structure will be replicated in patients with persecutory delusions, as RNT in the form of worry is implicated in the maintenance of persecutory delusions. It is also predicted that a valid measure of RNT would show significant differences between the levels of perseverative thinking in this group in comparison to a general population (non-clinical) group (i.e. will show criterion validity). We predicted demonstration of convergent validity with the PSWQ. Further, since worry is a form of RNT that has been implicated in the development and maintenance of paranoia (Freeman et al., Reference Freeman, Garety, Kuipers, Fowler and Bebbington2002) and demonstrated to correlate with paranoia using the PSWQ (e.g. Freeman et al., Reference Freeman, Pugh, Antley, Slater, Bebbington and Gittins2008), we also predicted that PTQ scores will correlate with paranoia scores.
Method
Participants
One hundred and forty-two patients with persecutory delusions completed the PTQ during the baseline assessment, prior to randomization, of a clinical trial (ISRCTN23197625) (Freeman et al Reference Freeman, Dunn, Startup and Kingdon2012; Freeman et al., Reference Freeman, Dunn, Startup, Pugh, Cordwell and Mander2015). The participants were recruited from two mental health NHS Trusts: Oxford Health NHS Foundation Trust and Southern Health NHS Foundation Trust.
The inclusion criteria were: a current persecutory delusion as defined by Freeman and Garety (Reference Freeman and Garety2000); scoring at least 3 on the conviction scale of the PSYRATS delusions scale (i.e. at least 50% conviction in the delusion) (Haddock, McCarron, Tarrier and Faragher, Reference Haddock, McCarron, Tarrier and Faragher1999); that the delusion had persisted for at least 3 months; a clinical diagnosis of schizophrenia, schizoaffective disorder or delusional disorder; a clinically significant level of worry, as indicated by scores above 44 on the Penn State Worry Questionnaire (see Startup and Erickson, Reference Startup, Erickson, Davey and Wells2006); aged between 18 and 65; and no changes in medication in the past month. Criteria for exclusion were: a primary diagnosis of alcohol or substance dependency or personality disorder; organic syndrome or learning disability; a command of spoken English inadequate for engaging in therapy; and currently having individual CBT.
The non-clinical group was made up of 273 volunteers from the general population who filled in the measures via online survey software (Bristol Online Survey) during screening for suitability for other studies run by the Oxford Cognitive Approaches to Psychosis research group (Freeman et al., Reference Freeman, Dunn, Murray, Evans, Lister and Antley2014).
Measures
Perseverative Thinking Questionnaire (PTQ; Ehring et al., Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011)
The PTQ is a 15-item measure of repetitive negative thinking. Each item is rated on a 5-point scale, from 0 = “Never” to 4 = “almost always” and asks participants to indicate how they typically think about negative experiences or problems. Scores can range from 0 to 60, and higher scores indicate higher levels of repetitive thought.
Penn State Worry Questionnaire (PSWQ; Meyer et al., Reference Meyer, Miller, Metzger and Borkovec1990)
The PSWQ is the most established measure of trait worry style (“I have been a worrier all my life”) and has been used in non-clinical and clinical populations (see review by Startup and Erickson, Reference Startup, Erickson, Davey and Wells2006). Each of the 16 items is rated on a 5-point scale. Higher scores indicate a greater tendency worry.
Green et al. Paranoid Thoughts Scale (GPTS; Green et al., Reference Green, Freeman, Kuipers, Bebbington, Fowler and Dunn2008)
The GPTS is a 32-item measure of paranoid thinking. Part A assesses ideas of reference (e.g. “It was hard to stop thinking about people talking about me behind my back”) and Part B assesses ideas of persecution (e.g. “I was convinced there was a conspiracy against me”). Each item is rated on a 5-point scale. Higher scores indicate greater levels of paranoid thinking. The scale was completed for the period of the previous fortnight. The non-clinical group completed Part B only.
Analysis
The confirmatory factor analysis (CFA) was carried out using Mplus Version 7 (Muthén and Muthén, Reference Muthén and Muthén1998–2012). All other analyses were carried out using SPSS Version 20 (IBM, 2011) and all hypothesis testing was two-tailed.
First, the internal reliability of the PTQ was assessed by calculating Cronbach's alphas for each participant group. Next, a CFA for the patient group was performed to test for the proposed second order model of the PTQ: with one higher-order and three lower-order factors. This was assessed using chi-square (χ2) and Comparative Fit Index (CFI) statistics. With this approach, a good fit is indicated by non-significant chi-square statistics and CFI greater than 0.95. Then, PTQ scores for both participant groups were compared using t-tests to establish criterion validity.
Finally, convergent validity of the PTQ was assessed by correlating PTQ total scores for each participant group with their PSWQ total scores and with GPTS Part B scores.
Results
Demographics of the sample
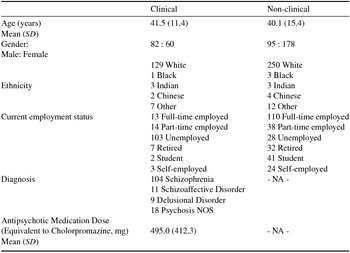
Basic demographic and clinical data for both the clinical and non-clinical participant groups are displayed in Table 1. Analysis with a t-test indicated no significant difference in age, and a chi-square test indicated no significant difference in ethnicity between the two groups, but there were proportionally more males in the clinical than the non-clinical group (χ2 = 20.11, p < .001).
Table 1. Demographics of the two participant groups, including clinical details for the clinical group. Analysis indicates no significant differences between groups in age or ethnicity, but the clinical group was found to include proportionally more male participants than the non-clinical group.
Internal reliability of scale
Cronbach's alphas were calculated for each group to determine the internal reliability of the PTQ measure. Internal reliability was found to be high (Clinical: Cronbach's alpha = 0.923; Non-clinical: Cronbach's alpha = 0.968).
Factor structure of the PTQ
The data from the 142 participants in the clinical group were analysed using a confirmatory factor analysis. Traditional CFA indicated a good fit of the data to Ehring et al.'s (Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) factor structure of one higher-order and three lower-order factors (χ2 = 332.40, df = 87, CFI = 0.96). Note that this CFI is comparable to that of Ehring et al.'s clinical sample, study 1 (CFI = 0.95).
Comparison of patients with the non-clinical controls
The total PTQ score and each of the three lower-order subscale scores were found to be significantly higher in the clinical than the non-clinical group. The results for these t-tests are shown in Table 2. For all comparison, Levene's tests of equal variance indicated that the standard deviations of the two groups could not be assumed to be equal, and therefore t-tests based on a Satterthwaite approximation were used.
Table 2. Showing the statistics for the t-tests carried out to test for statistically significant differences between the two groups’ scores on the PTQ (total and subscales)

The PTQ total scores for both groups are consistent with previous research: Martinelli et al. (Reference Martinelli, Cavanagh and Dudley2013) report a mean total of 28.91 (SD = 11.77) on the PTQ in their student sample, whilst Raes’ (Reference Raes2012) and Burg and Michalak's (Reference Burg and Michalak2011) student groups scored a mean of 28.85 (SD = 8.31) and 26.78 (SD = 9.57) respectively. The clinical group here score similarly to Teismann et al.'s (Reference Teismann, von Brachel, Hanning, Grillenberger, Hebermehl and Hornstein2014) two depression groups (baseline results for active group: mean = 41.32, SD = 8.80; baseline for control group: mean = 43.11, SD = 7.66).
Convergent validity
The convergent validity between the PTQ and PSWQ was found to be high for each participant group (Non clinical: r = 0.79, p < .001; Clinical: r = 0.50, p < .001).
Convergent validity with the GPTS Part B was also significant (Nonclinical: r = 0.457, p < .001; Clinical: r = 0.299, p < .001).
Discussion
The current study sought to validate Ehring et al.'s Perseverative Thinking Questionnaire (PTQ) in a different patient group: people with persecutory delusions. Validating the PTQ in this group would support Ehring et al.'s view that the PTQ is likely to be a transdiagnostic, “content-free” measure of repetitive negative thinking (RNT), which is proposed to maintain a range of psychological disorders. The one higher-order, three lower-order factor structure of the PTQ has been confirmed here, with values comparable to those in Ehring et al.'s (Reference Ehring, Zetsche, Weidacker, Wahl, Schönfeld and Ehlers2011) validation of the measure.
Analysis has also shown the ability of the PTQ to distinguish between a clinical and non-clinical sample, demonstrating its criterion validity. The clinical group scored significantly higher than the non-clinical participants on every subscale of the measure.
The results of the current study lend support to the theoretical conceptualization of the PTQ as a transdiagnostic measure of RNT. By replicating the factor structure with a novel clinical group, the assertion that the PTQ measures a transdiagnostic process is supported; whilst finding significant differences in PTQ scores between groups of participants with and without a clinical symptom theorised to be maintained by worry (a ruminative process) establishes the validity of the PTQ. The convergent validity of the PTQ with the PSWQ is also positive, as it suggests that the PTQ is measuring sequelae also assessed by the PSWQ, thus supporting its validity as a measure of RNT.
A further strength of the PTQ is its relative ease of use for patients, particularly in comparison to the PSWQ, which includes a number of fairly complex-worded reverse items. The PTQ uses items that are short and easily understood, with no reversed items. This is a benefit when working with a psychosis population as cognitive difficulties are common in this group and therefore more accessible questionnaires are preferable.
Limitations
There are limitations to the current study that should be addressed in further evaluation of the PTQ in a psychosis population. First, we have not completed a test-retest reliability analysis. This would be a valuable addition to future research in this area.
A further weakness of the study is that the PTQ was only compared against the PSWQ and not a standard depressive rumination measure, which would have offered a more complete understanding of the value of the PTQ in comparison to existing measures of RNT.
It could also be argued that the clinical sample used in this study is not representative, since the clinical trial they were being assessed for has an entry criterion of a high PSWQ score. This therefore selects the highest worriers in the population and it would naturally follow that these participants would show high scores on the PTQ, since worry and RNT are related concepts. However, in the recruitment of 150 participants with a persecutory delusion for the clinical trial, only 8 people were excluded on the basis of scoring below cut-off on the PSWQ. Hence it could be said that high worry is a typical feature in the overwhelming majority of people with current persecutory delusions, and therefore that this high-worry sample is representative. Nevertheless, future research may wish to consider using a comparison group of patients without persecutory delusions. Overall, this study supports the use of the PTQ in psychosis populations.
Acknowledgements
This study was carried out within a project (09/160/06) awarded by the Efficacy and Mechanism Evaluation (EME) Programme, and is funded by the UK Medical Research Council (MRC) and managed by the UK NHS National Institute for Health Research (NIHR) on behalf of the MRC-NIHR partnership. DF is supported by a UK Medical Research Council (MRC) Senior Clinical Fellowship (G0902308). Methodological research by GD is supported by the MRC (MR/K006185/1).
Ethical standards: The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflict of interest: The authors have no conflicts of interest with respect to this publication.





Comments
No Comments have been published for this article.