Introduction
Experiential avoidance (EA), an unwillingness to experience uncomfortable internal stimuli, has been found to be associated with many psychiatric symptoms including higher levels of psychopathology, anxiety, depression, trauma symptoms, and lower quality of life (Hayes et al., Reference Hayes, Strosahl, Wilson, Bissett, Pistorello, Toarmino, Polusny, Dykstra, Batten, Bergan, Stewart, Zvolensky, Eifert, Bond, Forsyth, Karekla and McCurry2004). As Hayes et al. (Reference Hayes, Strosahl, Wilson, Bissett, Pistorello, Toarmino, Polusny, Dykstra, Batten, Bergan, Stewart, Zvolensky, Eifert, Bond, Forsyth, Karekla and McCurry2004) reviewed, EA is a process of taking steps to avoid those stimuli even though avoidance is not always beneficial in the long run. They suggest psychological discomfort is often a necessary part of healthy behaviour change, and these attempts to avoid uncomfortable events (i.e. experiential avoidance) often end up increasing the private events such as the negative evaluations of inner experiences like anxiety and uncomfortable thoughts (Hayes et al., Reference Hayes, Strosahl, Wilson, Bissett, Pistorello, Toarmino, Polusny, Dykstra, Batten, Bergan, Stewart, Zvolensky, Eifert, Bond, Forsyth, Karekla and McCurry2004). These increases in uncomfortable thoughts and feelings often make it challenging for individuals to take values-based action, making EA harmful and related to psychopathology (Hayes et al., Reference Hayes, Strosahl, Wilson, Bissett, Pistorello, Toarmino, Polusny, Dykstra, Batten, Bergan, Stewart, Zvolensky, Eifert, Bond, Forsyth, Karekla and McCurry2004).
The treatment outcome literature has provided additional support regarding EA as an important contributing factor to psychopathology. For example, Dalrymple and Herbert’s (Reference Dalrymple and Herbert2007) findings suggest that targeting EA may positively influence overall avoidance, treatment acceptability, quality of life, and specific anxiety disorder symptoms. In their trial integrating CBT with ACT for patients with social anxiety disorder (SAD), patients demonstrated improved symptoms and quality of life, and decreased experiential avoidance (Dalrymple and Herbert, Reference Dalrymple and Herbert2007). Furthermore, the authors found that early changes in experiential avoidance predicted later changes in SAD symptoms, while controlling for symptom changes and perceived control over emotional reactions (Dalrymple and Herbert, Reference Dalrymple and Herbert2007).
Recent findings have highlighted EA’s potential as an important contributing factor when looking at co-morbid depressive symptoms within emotional disorders (Rueda and Valls, Reference Rueda and Valls2016; Spinhoven et al., Reference Spinhoven, Drost, Rooij, Hemert and Penninx2014). This is important work to continue, as major depressive disorder (MDD) is considered to be a top global cause of disability (Torres et al., Reference Torres, Fontenelle, Shavitt, Ferrão, Rosário, Storch and Miguel2016; World Health Organization, 2017). EA has been found to be a unique contributor to depression symptoms, across a variety of studies and settings (Wenzlaff and Eisenberg, Reference Wenzlaff and Eisenberg2001; Wenzlaff et al., Reference Wenzlaff, Wegner and Roper1988). This includes when measured using the AAQ to operationalize experiential avoidance (Cribb et al., Reference Cribb, Moulds and Carter2006). EA may also be a mechanism that relates with other cognitive and emotional constructs like anxiety sensitivity to depression, making it important to study for greater understanding of depression and co-occurring diagnoses (Tull and Gratz, Reference Tull and Gratz2008).
Multiple studies have extended this work and explored the impact of experiencing depressive symptoms alongside other psychiatric diagnoses, including borderline personality disorder, bipolar disorder, and post-traumatic stress disorder (Berking et al., Reference Berking, Neacsiu, Comtois and Linehan2009; Rueda and Valls, Reference Rueda and Valls2016; Tull et al., Reference Tull, Gratz, Salters and Roemer2004; Wenze et al., Reference Wenze, Kats and Gaudiano2018). In general, they found EA to be associated with depression symptom severity while controlling for the other diagnosis’ symptoms (Berking et al., Reference Berking, Neacsiu, Comtois and Linehan2009; Rueda and Valls, Reference Rueda and Valls2016; Tull et al., Reference Tull, Gratz, Salters and Roemer2004; Wenze et al., Reference Wenze, Kats and Gaudiano2018). More specifically, Berking et al. (Reference Berking, Neacsiu, Comtois and Linehan2009) found that reductions in EA influenced later reductions in depression, while Wenze et al. (Reference Wenze, Kats and Gaudiano2018) noted that blunted mood led to increased EA. The results of Berking et al. (Reference Berking, Neacsiu, Comtois and Linehan2009) came when a potential overlap between depression and EA was controlled for, supporting the distinct nature of these constructs.
A similar pattern has been found within the literature surrounding OCD. OCD and depression are commonly co-morbid, with almost 70% of people with OCD also having major depressive disorder diagnoses (Miguel et al., Reference Miguel, Ferrão, Rosário, Mathis, Torres, Fontenelle, Hounie, Shavitt, Cordioli, Gonzalez, Petribú, Diniz, Malavazzi, Torresan, Raffin, Meyer, Braga, Borcato, Valério and Silva2008). Depression has been found to be associated with lower quality of life in those with OCD (Eisen et al., Reference Eisen, Mancebo, Pinto, Coles, Pagano, Stouf and Rasmussen2006; Fontenelle et al., Reference Fontenelle, Fontenelle, Borges, Prazeres, Range, Mendlowicz and Versiani2010; Jacoby et al., Reference Jacoby, Leonard, Riemann and Abramowitz2014; Velloso et al., Reference Velloso, Piccinato, Ferrão, Perin, Cesar, Fontenelle, Hounie and Rosário2018; Vorstenbosch et al., Reference Vorstenbosch, Hood, Rogojanski, Antony, Summerfeldt and McCabe2012). Similarly, Meyer et al. (Reference Meyer, McNamara, Reid, Storch, Geffken, Mason, Murphy and Bussing2013) found that lower OCD symptom severity was predictive of lower depression symptoms for children and adolescents enrolled in a cognitive behaviour therapy and pharmacological treatment trial. Furthermore, in an adult sample, changes in OCD symptoms predicted changes in depressive symptoms (Anholt et al., Reference Anholt, Aderka, Balkom, Smit, Hermesh, Haan and Oppen2011; Tibi et al., Reference Tibi, Oppen, Balkom, Eikelenboom, Rickelt, Schruers and Anholt2017; Zandberg et al., Reference Zandberg, Zang, McLean, Yeh, Simpson and Foa2015). There have been some studies finding results in the opposite direction, including the work of Anholt et al. (Reference Anholt, Aderka, Balkom, Smit, Hermesh, Haan and Oppen2011) and Zandberg et al. (Reference Zandberg, Zang, McLean, Yeh, Simpson and Foa2015) who found that changes in OCD predicted large percentages of changes in depression, but also found that changes in depression partially mediated changes in OCD. Additionally, Toledano et al. (Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020) found in their study of self-esteem throughout treatment for OCD that self-esteem across treatment, variability in self-esteem, and depressive symptoms were related to OCD severity at post-treatment. They also found that self-esteem affected the rate of depressive symptom change but not OCD symptom change, and that self-esteem significantly increased before and after each session of ERP (Toledano et al., Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020). They discuss that their finding builds on work stating that ERP for OCD results in improvements for depression symptoms, summarizing that ERP treatment may help patients come into contact with positive reinforcement through a sort of behavioural activation, and that reduced OCD symptoms may help build self-efficacy and mastery and decrease hopelessness (for a summary and relevant studies, see Toledano et al., Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020). They suggest that ERP may provide patients with opportunities to confront fears or obsessions, which helps improve global-self-esteem and then leads to reduced depression (Toledano et al., Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020).
These facts, combined with the high degree of co-morbidity between OCD and depression symptoms reinforce the importance of exploring what underlies depressive symptoms in the context of OCD. While the current literature suggests the strong relationship between OCD and depression symptoms, along with the influence of changes in OCD symptoms on co-morbid depression, limited focus has been given to better understanding what mechanisms may influence these changes in depressive symptoms.
As described above, the role of EA has found support for its role in this relationship within other psychiatric diagnoses; however, evaluation of the relationship between EA and depression symptoms in samples with a primary diagnosis of OCD has been limited.
Experiential avoidance and intolerance of internal experiences
EA has been previously studied within the broader context of intolerance of internal experiences (IIE), which has more generally been found to be related to OCD symptoms (Blakey et al., Reference Blakey, Jacoby, Reuman and Abramowitz2015; Robinson and Freeston, Reference Robinson and Freeston2014). IIE is conceptualized as a difficulty managing unwanted thoughts and emotions, and contains EA and distress tolerance (DT) as subsets of IIE. While there is some variation in the literature in this area, generally, EA and DT are considered related, yet distinct constructs (Blakey et al., Reference Blakey, Jacoby, Reuman and Abramowitz2015; Robinson and Freeston, Reference Robinson and Freeston2014; Leyro et al., Reference Leyro, Zvolensky and Bernstein2010). Compared with EA, which has been previously described as an unwillingness to experience uncomfortable emotions, DT refers to an ability to endure these uncomfortable emotions (Blakey et al., Reference Blakey, Jacoby, Reuman and Abramowitz2015). Both EA and DT involve inhibitory processes, although they are not identical processes. EA is a strategy/skill that attempts to influence uncomfortable responses to the context/person’s surroundings. Low DT may be associated with similar avoidant behaviour, but is not the same as EA (Leyro et al., Reference Leyro, Zvolensky and Bernstein2010). Blakey et al. (Reference Blakey, Jacoby, Reuman and Abramowitz2015) differentiated between DT and EA, stating that DT relates to an ability to tolerate distress versus EA reflecting a willingness to tolerate it. Furthermore, they found EA to influence obsessional symptoms above and beyond DT and depressive symptoms (Blakey et al., Reference Blakey, Jacoby, Reuman and Abramowitz2015). Unfortunately, there are limited existing studies in the DT literature evaluating the links between DT and conceptually overlapping/related constructs such as EA, thus further work is necessary to advance our understanding of these constructs and their relation to psychopathology (Leyro et al., Reference Leyro, Zvolensky and Bernstein2010). In line with this need, the following study controlled for DT when observing the role of EA in depression symptoms within the context of OCD.
Aims and hypotheses
This study sought to explore the relationship between EA and depression symptoms (when controlling for DT and OCD symptom severity) within patients with severe OCD engaged in IRT. The first aim of the study was to examine the relationships between depressive symptoms, OCD symptom severity, DT and EA both at admission and discharge from IRT. It was hypothesized that all the variables would be significantly related to each other at moderate levels, both at admission and discharge time points. The second aim of the study was to examine EA as a potential contributing factor to depressive symptoms in those with a primary diagnosis of OCD while controlling for change in DT and OCD symptom severity. In line with the findings by Rueda and Valls (Reference Rueda and Valls2016), it was hypothesized that EA would emerge as a significant contributing factor to co-morbid depressive symptom severity and change in depression symptoms across IRT.
Method
Participants
This study included 311 adults seeking IRT for OCD and related disorders. Each participant had a primary DSM IV-TR diagnosis of OCD based on structured clinical interview. They consented to being involved in research between 2014 and 2017.
During IRT for OCD, these patients received an intensive CBT-based approach built on exposure with response prevention (ERP). Additional empirically based treatment strategies, including acceptance and commitment therapy (ACT), emotion regulation skills, and interpersonal effectiveness were integrated as warranted. Each participant worked with a multidisciplinary treatment team, which included a primary behaviour therapist, family therapist and psychiatrist, along with attending daily group therapy. Patients are typically referred for intensive/residential treatment by their out-patient teams when a need for a higher dosage of ERP is necessary. This may be due to a variety of factors, including symptom severity, challenges with implementation of independent exposure practices, identified need for more wrap-around support, and/or challenges related to co-morbid conditions that may impede ability to access skills being taught in an out-patient setting. The co-morbidities of this sample are reflected in more detail in the following paragraphs.
The sample had an average age of 30.26 years (range 16–83 years; SD = 13.02), primarily identified as Caucasian; there was a roughly even split of gender, and the majority lived in the United States (see Table 1 for further information on social demographics of the sample). Almost half of the sample had been experiencing symptoms since childhood (n = 149, 48.1%), and another 29% since adolescence (n = 90). For age of onset, the 25th percentile was age 8, the 50th percentile was age 12, the 75th percentile was age 17, the highest reported age of onset was 47 years, and 10 participants reported they could not estimate their age of onset. The sample had a co-morbidity rate of 84.9%, with the most common co-morbid disorder being MDD (n = 137, 44.1%), followed by social phobia (n = 28, 9%) and generalized anxiety disorder (n = 22, 7.1%). In addition, many participants were observed to have more than one co-morbid clinical diagnosis, with 186 participants (59.8%) meeting diagnostic criteria for a second co-morbid diagnosis, and 86 participants (27.6%) having a third co-morbid diagnosis. The majority of the sample had sought therapy for OCD both currently and in the past (n = 201, 65%). A small section of the sample had never taken medication (n = 19, 6.2%), and most of the patients had taken it for one or more years (n = 284, 92.2%). The majority of patients were residential patients (n = 238, 76.5%). About a third of participants had been hospitalized at least once for OCD (n = 119, 38.2%) and at least once for other psychiatric reasons (n = 102, 32.8%). See Table 2 for a summary of treatment demographics of the sample.
Table 1. Social demographics of the sample
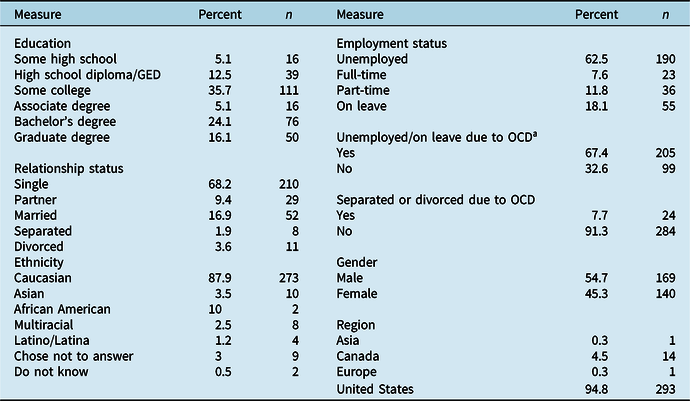
Varying numbers of participants answered each question set.
a Unemployed or on leave from work or school due to OCD symptoms.
Table 2. Treatment characteristics of the sample
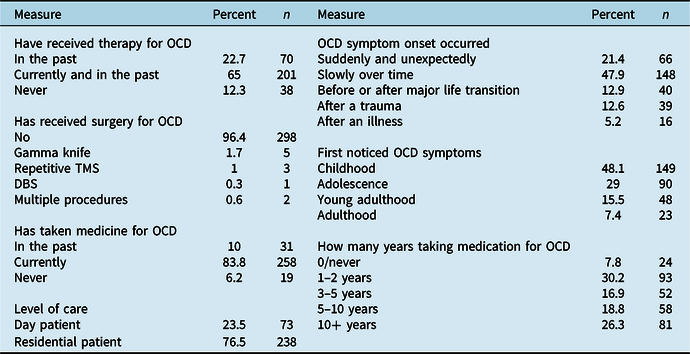
Varying numbers of participants answered each question set.
Measures
Structured Clinical Interview for DSM Disorders-I (SCID-I) for DSM-IV-TR Axis I Disorders
In order to confirm a primary diagnosis of OCD, patients were administered the Net SCID (Brodey et al., Reference Brodey, First, Linthicum, Haman, Sasiela and Ayer2016) following admission. The SCID is a structured clinical interview that is used to determine if a patient has any Axis I disorders according to the DSM-IV-TR (First et al., Reference First, Spitzer, Gibbon and Williams2007). The Net SCID is a web-based version of the SCID that is validated and comparable to the paper SCID (Brodey et al., Reference Brodey, First, Linthicum, Haman, Sasiela and Ayer2016). The Net SCID was administered by trained research assistants and graduate students, who were under the supervision of a post-doctoral fellow and/or licensed clinical psychologist. In addition, assessors engaged in weekly assessment supervision where the clinical assessments and diagnostic impressions were reviewed.
Yale-Brown Obsessive-Compulsive Scale-Self Report Version (Y-BOCS)
The Y-BOCS is a 10-item scale designed to measure the severity of OCD symptoms (Goodman et al., Reference Goodman, Price and Rasmussen1989). Each item has options ranging from 0 to 4 (no symptoms to extreme symptoms), with total scores ranging from 0 to 40 and subscales for obsessions and compulsions (Goodman et al., Reference Goodman, Price and Rasmussen1989). The scale has been found to have excellent inter-rater reliability for the total score and each item, as well as high internal consistency (Goodman et al., Reference Goodman, Price and Rasmussen1989). The scale has also been found to have high convergent validity with other measures of OCD (Woody et al., Reference Woody, Steketee and Chambless1995). This study utilized the self-report version of the Y-BOCS, which has been shown to have good psychometric properties and convergent validity with the clinician administered Y-BOCS (Steketee et al., Reference Steketee, Frost and Bogart1996).
Distress Tolerance Scale (DTS)
The DTS is a 15-item self-report measure designed to capture distress tolerance, or the ability to endure and experience negative emotions (Simons and Gaher, Reference Simons and Gaher2005). It addresses agreement and disagreement with various items concerning core beliefs about being distressed (Simons and Gaher, Reference Simons and Gaher2005), utilizing a 5-point Likert scale (Simons and Gaher, Reference Simons and Gaher2005). The measure is scored across four subscales, Tolerance, Absorption, Appraisal, and Regulation, and a summary total score (Simons and Gaher, Reference Simons and Gaher2005). The measure has demonstrated good test–re-test reliability, along with good criterion, convergent and discriminant validity (Simons and Gaher, Reference Simons and Gaher2005). Cronbach’s alpha for this sample at admission was 0.90 and at discharge was 0.93.
Hamilton Rating Scale for Depression-6 (HAMD-6)
The HAMD-6 is a 6-item measure assessing depression that has been shown to have similar sensitivity to previous versions of the HAMD and allows for adequate assessment of depression (O’Sullivan et al., Reference O’Sullivan, Fava, Augustin, Baer and Rosenbaum1997). This measure consists of six items from the HAMD-17 surrounding mood, guilt, interests, psychomotor retardation, anxiety, and somatic symptoms (Bech et al., Reference Bech, Allerup, Gram, Reisby, Rosenberg, Jacobsen and Nagy1981). Cronbach’s alpha for this sample at admission was 0.86 and at discharge was 0.88.
Acceptance and Action Questionnaire II (AAQ-II)
The AAQ-II is a 7-item measure that assesses experiential avoidance, a concept sometimes referred to as acceptance or psychological inflexibility (Bond et al., Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011). The measure contains statements about internal feelings and emotions, and participants rate how much or how little they agree based on a 7-point Likert scale (Bond et al., Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011). The measure has demonstrated satisfactory structure, reliability and validity, and has shown across time to predict outcomes that line up with the underlying theory of the measure (Bond et al., Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011). Confirmatory factor analysis demonstrated adequate fit for the model treating AAQ-II scores as distinct from BDI-II; however, models combining them into a single factor did not show a good fit (Bond et al., Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011). Cronbach’s alpha for this sample at admission was 0.88 and at discharge was 0.91. The AAQ-II has been generally used as a measure of acceptance, experiential avoidance, and psychological inflexibility (Bond et al., Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011).
Analysis plan
All analyses were carried out using IBM SPSS Statistics for Macintosh, version 27 (IBM Corporation, 2020).
Missing data
The sample of 311 participants represents a subset of a larger data set that had consented to research during their intensive/residential treatment stay between 2014 and 2017. Participants included in this sample presented with a primary diagnosis was OCD. Missing data from the bootstrapped correlation analyses were as follows: correlations at admission (n = 7, 2.3%) and correlations at discharge (n = 34, 10.9%). Missing data from the regression models and paired sample t-tests were as follows: depression change (n = 34, 10.9%), OCD symptom severity change (n = 32, 10.3%), EA change (n = 39, 12.5%), and DT change (n = 40, 12.9%). Missing data for change variables occurred when the participant’s admission score, discharge score, or both were missing. Listwise deletion was utilized for all analyses.
Aim 1
Two sets of correlation analyses were carried out to study the relationships among depression, EA, DT and OCD symptom severity at both admission and discharge from IRT. Due to 12 tests being used, a Bonferroni correction was performed, and results were considered significant at the 0.004 level. Correlation analyses were carried out with 1000 bootstrapped samples and the bias-corrected and accelerated (BCa) method with 95% confidence intervals.
Aim 2
A hierarchical linear regression was calculated to predict change in depression across treatment with change in OCD symptom severity and distress tolerance entered in the first step, and change in EA entered in the second step. Residualized change scores were utilized as dependent variables in this study given that they have been found to produce similar results to change scores when no distinct group differences exist and account for potential regression to the mean (Saito, Reference Saito2020).
Results
Descriptive analysis
This sample showed an average Y-BOCS score of 25 (SD = 5.68) at admission and an average score of 15 (SD = 6.47) at discharge. The sample showed an average decrease in depression scores of 4.5 points on the HAMD-6. Scores on the AAQ-II averaged 33.32 at admission and 27.46 at discharge. The sample showed an average increase of 0.45 points in distress tolerance, and showed a mean of 2.5 on the DTS at admission and a mean of 3 on the DTS at discharge.
Paired sample t-tests on admission and discharge scores demonstrated significant changes in EA, depression severity, OCD severity, and DT across treatment in clinically expected directions (see Table 3). More specifically, participants demonstrated significant decreases in EA, depression and OCD symptoms, along with increases in DT scores, with medium effect sizes for changes in EA and DT, and large effect sizes for changes in depression and OCD symptoms (Cohen, Reference Cohen1988).
Table 3. Mental health at admission and discharge and paired samples t-tests
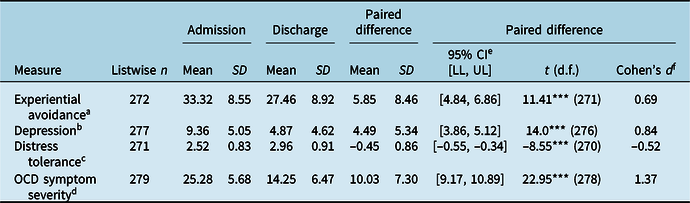
a Experiential avoidance as measured by the AAQ-II.
b Depression as measured by the HAMD-6.
c Distress tolerance as measured by the Distress Tolerance Scale.
d OCD symptom severity as measured by the Y-BOCS.
e CI, confidence interval; LL, lower limit; UL, upper limit.
f Cohen’s d corresponds to effect size of paired samples t-test.
*p<0.05; **p<0.01; ***p<0.001.
Aim 1
At both admission and discharge from IRT, higher EA, lower DT, and higher OCD symptom severity were associated with higher scores on the HAMD-6. At admission, EA was significantly moderately related to OCD symptom severity and strongly related to depression and DT. Depression was significantly moderately related to DT and OCD symptom severity, and DT was significantly weakly related to OCD symptom severity. At discharge, EA was significantly strongly related to depression, DT and OCD symptom severity. DT was significantly moderately related to depression and to OCD symptom severity. Depression was significantly strongly related to OCD symptom severity. Interpretations of magnitudes are based on Cohen’s (Reference Cohen1988) recommendations with correlations of 0.1 being weak, 0.3 being moderate, and 0.5 being strong. All correlations were also below 0.7, a common rule of thumb indicating multi-collinearity (Dormann et al., Reference Dormann, Elith, Bacher, Buchmann, Carl, Carré, Marquéz, Gruber, Lafourcade, Leitão, Münkemüller, McClean, Osborne, Reineking, Schröder, Skidmore, Zurell and Lautenbach2013). All results were significant at the α = 0.004 set for Aim 1. For further exploration of correlational relationships at admission and discharge, as well as 95% bootstrapped confidence intervals, see Table 4.
Table 4. Correlation analyses of symptoms at admission and discharge
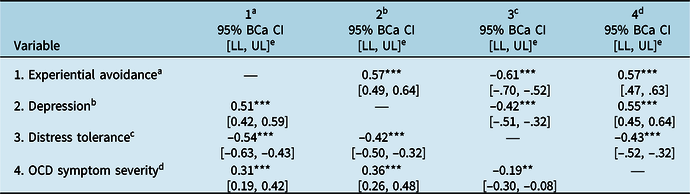
Bottom left triangle reflects admission correlations (listwise n = 304) and top right triangle reflects discharge (listwise n = 277).
a Experiential avoidance as measured by the AAQ-II.
b Depression as measured by the HAMD-6.
c Distress tolerance as measured by the Distress Tolerance Scale.
d OCD symptom severity as measured by the Y-BOCS.
e CI, confidence interval; LL, lower limit; UL, upper limit; confidence intervals created with 1000 bootstrapped samples and bias-corrected and accelerated method.
*p<0.05; **p<0.01; ***p<0.001.
Aim 2
The first step of the regression model was significant, with change in OCD symptom severity and change in distress tolerance accounting for 27.3% of the variance associated with residualized change in depression symptoms across IRT (F 2,268 = 50.296, p = .000, R 2 = 0.273). In this step, change in Y-BOCS score was significantly associated with residualized change in depression (β = 0.40, p = .000) and change in distress tolerance demonstrated a significant negative relationship with residualized reduction in HAMD-6 score across treatment (β = –0.21, p = .000). In model 2, adding change in EA explained an additional 7.1% of variance in change in depression (F 1,267 = 28.836, p = .000, ΔR 2 = .071). Change in OCD symptom severity (β = 0.32, p = .000) remained significant and change in distress tolerance (β = –0.09, p = .146) fell out of significance. Change in experiential avoidance was positively associated with residualized change in depression scores (β = 0.32, p = .000). Change in EA explained 34.4% of the variance in residualized change in depression (F 3,270 = 46.63, p = .000, R 2 = .344) after controlling for change in OCD symptom severity and change in DT. See Table 5 for details on the regression analyses.
Table 5. Regression of experiential avoidance on residualized depression change across IRT for OCD
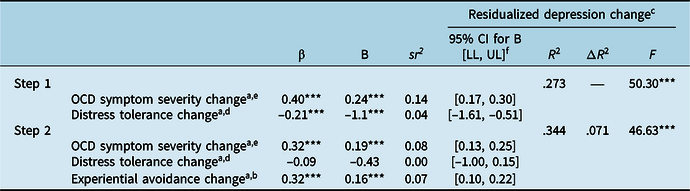
Listwise n = 271.
a Change scores created by subtracting admission scores from discharge.
b Experiential avoidance as measured by the AAQ-II.
c Depression as measured by the HAMD-6.
d Distress tolerance as measured by the Distress Tolerance Scale.
e OCD symptom severity as measured by the Y-BOCS.
f CI, confidence interval; LL, lower limit; UL, upper limit; CI refers to unstandardized B coefficient output from IBM SPSS Statistics V27.
*p<0.05; **p<0.01; ***p<0.001.
In order to further probe the distinctness of EA from other constructs in the model (DT, depression and OCD symptoms), we used a two-step hierarchical regression to predict the residualized change score of OCD symptoms from admission to discharge with DT and depression change in the first step and the addition of EA change in the second step. Adding change in EA explained an additional 3.7% of variance in residualized change in OCD symptoms (F 1,267 = 13.26, p = .000, ΔR 2 = .037), and together change in EA, change in depression, and change in DT explained 25.5% of the variance in residualized change in OCD symptoms (F 3,270 = 30.45, p = .000, R 2 = .255).
Summary of results
At admission and discharge, all constructs were significantly related such that higher EA, lower DT, and higher OCD symptom severity were associated with more depressive symptoms.
Change in OCD symptom severity significantly predicted residualized change in depression across treatment, and change in distress tolerance fell out of significance with the addition of change in experiential avoidance to predict residualized change in depression. Adding change in experiential avoidance significantly increased model fit when explaining residualized change in depression scores, and when the model was flipped to examine residualized change in OCD severity as the dependent variable.
Discussion
This study sought to explore the role of experiential avoidance in depression symptoms within patients with severe OCD seeking IRT. Furthermore, the relationship between change in EA, OCD symptom change, and depression symptoms across treatment was examined.
In terms of Aim 1, our hypotheses were mostly supported in that all of the variables would have significant moderate relationships with each other. There were relationships of varying strength. Results suggest that higher EA, lower DT, and greater OCD severity are all associated with greater depression severity, in line with previous research from Blakey et al. (Reference Blakey, Jacoby, Reuman and Abramowitz2015), who found these same relationships in their study of patients with OCD utilizing measures of EA, DT, OCD, and psychological distress instead of specifically depression.
Results also extended past research that found EA to be related to depression severity in samples with other primary diagnoses such as PTSD and bipolar disorder (Berking et al., Reference Berking, Neacsiu, Comtois and Linehan2009; Wenze et al., Reference Wenze, Kats and Gaudiano2018), to an OCD sample. Significant relationships between greater experiential avoidance and depression severity were observed in the regression model. More specifically, EA was significantly associated with reduction in depression symptoms, beyond that accounted for by OCD symptom reduction and changes in distress tolerance ability. These findings suggest that EA is a potential contributing factor to depressive symptoms in those with a primary diagnosis of OCD. This result builds on Rueda and Valls’ (Reference Rueda and Valls2016) hypothesis that EA is possibly an important target for addressing depressive symptoms in the context of psychiatric disorders, extending EA’s influence on depression symptoms into patients with OCD.
EA was a unique contributor to these constructs when added to a model using change in depression and DT to predict change in OCD symptoms. Given the potential overlap of the distress element in measures of all four constructs, with EA uniquely adding to a model above and beyond OCD change to predict depression change, and adding to a model above and beyond depression change to predict OCD change, results suggest that EA plays a unique role in understanding co-morbid depression in the context of OCD. Additionally, change in DT fell out of significance with the addition of EA in the model to predict depression, further showing that EA plays a unique role independent of general distress.
Overall, results add support to the idea that EA may be an important construct to consider when examining the relationship between OCD and co-morbid depression symptoms, and it suggests that EA may be an important variable in treatment response. We must also consider all the analyses in this study in the context of the treatments the patients were getting, which involved CBT and ERP along with ACT and other emotion regulation-based intervention strategies.
While this study provides support for the existence of these relationships, further work with more in-depth longitudinal models is needed to truly examine the role of EA as a mechanism of change and understand its differential effect on OCD and depression symptoms throughout treatment. More specifically, future models should better account for the nuances of change throughout psychotherapy, given conflicting consensus on the most appropriate way to analyse change in various situations. This study utilized residualized change scores to account for baseline severity of symptoms without inflating results, but latent change scores could better account for change and measurement error; they were beyond the scope of this current initial study (Saito, Reference Saito2020).
Exploration of underlying mechanisms of this relationship between OCD, EA and depression is important. Rumination may be an important mechanism to consider underlying the relationship between OCD and depression and potentially also non-suicidal self-injury, a behaviour considered to be experientially avoidant (McKay and Andover, Reference McKay and Andover2012). It has been linked to urges to compulse and associated distress, and to mediate the link between OCD symptoms and depression after treatment for OCD (Motivala et al., Reference Motivala, Arellano, Greco, Aitken, Hutcheson, Tadayonnejad, O’Neill and Feusner2018; Wahl et al., Reference Wahl, Hout and Lieb2019). In a study of rumination and EA, high ruminators experienced more EA according to the AAQ and fear of emotions according to the Affect Control Scale, demonstrating the convergent validity of the AAQ and the relevance of rumination in these relationships (Giorgio et al., Reference Giorgio, Sanflippo, Kleiman, Reilly, Bender, Wagner, Liu and Alloy2010). While evaluating rumination and specific avoidant behaviours like NSSI is out of the scope of this study, future work could explore the links between EA, depression and OCD, and the role of rumination.
Additionally, work should continue to explore existing hypotheses for the relationship between change in OCD and change in depression that was discussed in the Introduction and is summarized in Toledano et al. (Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020). It may be that specifically addressing EA in treatment facilitates opportunities to face fears, or address avoidance in the case of targeting EA, that helps build global self-esteem and decrease depression, as hypothesized by Toledano et al. (Reference Toledano, Guzick, McCarty, Browning, Downing, Geffken and McNamara2020).
This study illustrates that EA, an important target of ACT, is associated with co-occurring depressive symptoms along with its previously established relationship to OCD symptoms. Together, these provide further support for the utility of interventions targeting EA as a part of OCD treatment (Bluett et al., Reference Bluett, Homan, Morrison, Levin and Twohig2014; Twohig, Reference Twohig2009), especially when co-morbid depression may be present. For example, ACT seeks to increase psychological flexibility and to increase values-motivated activities by targeting six processes of change, one of which is acceptance, the opposite of EA (Twohig et al., Reference Twohig, Abramowitz, Bluett, Fabricant, Jacoby, Morrison, Reuman and Smith2015). Previous research has provided support for the inclusion of acceptance and values-based interventions in targeting avoidance involved in OCD and anxiety. For example, past studies have demonstrated that ACT can enhance exposure-based treatment for anxiety disorders and OCD, and recent studies have shown that ACT-based exposure treatments for OCD and anxiety lead to lower scores on the AAQ-16 (Arch et al., Reference Arch, Eifert, Davies, Vilardaga, Rose and Craske2012) and AAQ-II (Twohig et al., Reference Twohig, Abramowitz, Smith, Fabricant, Jacoby, Morrison, Bluett, Reuman, Blakey and Ledermann2018). The current study extends support for the utility of acceptance/value-based interventions when co-morbid depression-related symptoms are present.
This study utilized a large, naturalistic, treatment-seeking sample to examine the role of EA within co-morbid depressive symptoms in the context of severe OCD. The wide range of presenting symptoms and co-morbidity further support the importance of addressing EA in real-world clinical settings, allowing for examination of these relationships in complex symptom presentations. This study was one of the first to explore the role of EA in depressive symptoms within an OCD sample – however, it is important to note that the intensive/residential setting may represent a unique proportion of individuals with OCD symptoms and limited variability of social demographics may limit generalizability. Thus, future studies would benefit from examining multiple levels of care. Furthermore, future studies would benefit from accounting for temporal precedence in their analysis to better evaluate the order of variable change across treatment.
Lastly, this study utilized the AAQ-II, a widely used but sometimes questioned measure of experiential avoidance that has recently been found to lack optimal construct, discriminant and convergent validity with other newer measures of experiential avoidance and related measures of distress (Ong et al., Reference Ong, Pierce, Petersen, Barney, Fruge, Levin and Twohig2020; Rochefort et al., Reference Rochefort, Baldwin and Chmielewski2018). Initially, in terms of discriminant validity, Bond et al. (Reference Bond, Hayes, Baer, Carpenter, Guenole, Orcutt, Waltz and Zettle2011) found discriminant validity between the AAQ-II and the BDI-II measure of depression, whereas the current study used a brief depression measure. Research into experiential avoidance, depression and other diagnoses could be improved by more extensive depression measures.
As Ong et al. (Reference Ong, Pierce, Petersen, Barney, Fruge, Levin and Twohig2020) and Rochefort et al. (Reference Rochefort, Baldwin and Chmielewski2018) state, more research and use of the newer measures of psychological flexibility should continue. Furthermore, work should continue to develop measures that capture the nuanced process-based and hierarchical nature of psychological flexibility, measuring each sub-construct and the broader factors instead of attempting to measure psychological flexibility as a unidimensional construct like the AAQ-II. Future work should explore some of the measures that capture the more nuanced aspects of psychological flexibility, like the MPFI and UFM scales (Rogge and Daks, Reference Rogge and Daks2021; Rolffs et al., 2016). Additionally, development/utilization of a more tailored measure of EA designed for OCD samples may help increase sensitivity to EA’s role in this population. A full discussion into the nuances and current literature on measurement of psychological flexibility is beyond the scope of this paper, and the AAQ-II was a widespread and prominent measure of experiential avoidance at the time of data collection. In future studies we plan to utilize more recent measures, and it is our hope that this brief discussion provides a platform for others to do the same.
Conclusions
This study examined the role of EA in the context of depressive symptoms in patients with OCD through the course of IRT for OCD. Changes in EA were found to significantly add to the model explaining change in depression symptoms across treatment, even after accounting for the role of distress tolerance and change in OCD symptoms. These results build on previous findings within the broader literature suggesting that EA is an important target in treating depressive symptoms in the context of co-morbid psychiatric disorders. Given the established connection between depression symptoms and quality of life in those with OCD (Eisen et al., Reference Eisen, Mancebo, Pinto, Coles, Pagano, Stouf and Rasmussen2006; Fontenelle et al., Reference Fontenelle, Fontenelle, Borges, Prazeres, Range, Mendlowicz and Versiani2010; Jacoby et al., Reference Jacoby, Leonard, Riemann and Abramowitz2014; Velloso et al., Reference Velloso, Piccinato, Ferrão, Perin, Cesar, Fontenelle, Hounie and Rosário2018; Vorstenbosch et al., Reference Vorstenbosch, Hood, Rogojanski, Antony, Summerfeldt and McCabe2012), this relationship between EA and depression symptoms reinforces the importance of directly addressing EA in the context of OCD treatment to help individuals with co-morbid depression symptom to lead fulfilling lives according to their values.
Acknowledgements
We would like to thank the patients for their participation in this clinical research and the Office of Clinical Assessment and Research (OCAR) staff for their support of this project.
Financial support
Anonymous philanthropy provided support for the broader research activities that led to the collection of the data analysed in this paper.
Conflicts of interest
The authors declare none.
Ethics statements
The authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the APA (http://www.apa.org/ethics/code/) which align with the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. This study was approved by the hospital’s Institutional Review Board (approval number 2014P000509).
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author.
Author contributions
Morgan E. Browning: Conceptualization (lead), Formal analysis (lead), Methodology (lead), Writing-original draft (lead), Writing-review & editing (equal); Nathaniel P. Van Kirk: Conceptualization (supporting), Data curation (equal), Formal analysis (supporting), Methodology (supporting), Supervision (lead), Writing-original draft (supporting), Writing-review & editing (equal); Jason W. Krompinger: Data curation (supporting), Formal analysis (supporting), Project administration (supporting), Writing-review & editing (equal).








Comments
No Comments have been published for this article.