Introduction
The concept of readiness for change has been known as part of assessing suitability for therapy and adapting therapy for years (Geller et al., Reference Geller, Zaitsoff and Srikameswaran2005; Geller and Drab, Reference Geller and Drab1999; McConnaughy et al., Reference McConnaughy, Prochaska and Velicer1983; Truant, Reference Truant1999). Despite an anecdotal understanding of ‘whether a patient is ready to engage in therapy’, few measures exist (Haggerty et al., Reference Haggerty, Siefert, Stoycheva, Sinclair, Baity, Zodan, Mehra, Chand and Blais2014; Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009) and there is little research into associations between readiness and therapy outcomes. No specific measures are routinely used to measure this construct in psychological therapy services in the United Kingdom such as Improving Access to Psychological Therapies (IAPT) services which have been established across England, to provide NICE-recommended psychological therapies for depression and anxiety disorders (Clark, Reference Clark2011).
The transtheoretical model (TTM) of change is a prominent theory that describes motivation for behaviour change. It has been applied to addiction literature (Prochaska et al., Reference Prochaska, DiClemente and Norcross1992), smoking cessation (DiClemente et al., Reference DiClemente, Prochaska, Fairhurst, Velicer, Velasquez and Rossi1991), exercise uptake (Marcus et al., Reference Marcus, Rakowski and Rossi1992) and other problem behaviours (Prochaska et al., Reference Prochaska, Velicer, Rossi, Goldstein, Marcus, Rakowski, Fiore, Harlow, Redding and Rosenbloom1994).
Literature regarding the application of TTM to readiness for therapy typically focuses on more severe and enduring mental health problems such as eating disorders or addiction. Meta-analyses have yielded inconsistent results when generalising the TTM to readiness for therapy (Rosen, Reference Rosen2000). The use of the TTM to conceptualise readiness for therapy has also been criticised, highlighting that readiness for behaviour change and readiness for therapy are not synonymous constructs. Readiness for therapy is a more complex construct to measure than specific behaviour change (Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009). A review of meta-analyses found some clinically significant associations between stages of change and therapy outcomes (Norcross et al., Reference Norcross, Krebs and Prochaska2011), again mostly focusing on populations with severe and enduring mental health difficulties. Indeed, a measure has been developed specifically to measure the stages of change for those with a diagnosis of anorexia nervosa (Rieger et al., Reference Rieger, Touyz and Beumont2002) and for engagement in psychodynamic psychotherapy for severe depression or anxiety (Laaksonen et al., Reference Laaksonen, Lindfors, Knekt and Aalberg2012).
The literature may focus more upon severe and enduring mental health difficulties with regard to readiness due to motivational interviewing techniques finding their roots within addiction treatments (Rollnick and Miller, Reference Rollnick and Miller1995), thus perpetuating a gap in the literature with regard to common mental health problems. Some trials have considered use of motivational interviewing techniques as a pre-cursor to CBT, finding reduced rates of drop-out in cases of severe anxiety disorders (Westra et al., Reference Westra, Constantino and Antony2016; Westra and Norouzian, Reference Westra and Norouzian2018).
A possible utility of readiness measures include the predictive ability of engagement, or non-engagement with treatment. Current measures of readiness for therapy (Haggerty et al., Reference Haggerty, Siefert, Stoycheva, Sinclair, Baity, Zodan, Mehra, Chand and Blais2014; Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009) do not predict clinical outcomes or engagement with therapy. A semi-structured clinical interview designed to measure ‘suitability’ for short-term cognitive therapies (Safran et al., Reference Safran, Vallis, Segal and Shaw1986) has predicted therapy outcomes but not attrition from therapy (Renaud et al., Reference Renaud, Russell and Myhr2014). In the addiction literature, treatment readiness has been shown to be predictive of engagement, retention and attrition (Brogan et al., Reference Brogan, Prochaska and Prochaska1999; Joe et al., Reference Joe, Simpson and Broome1998). Reliability of current measurement scales has also been reviewed for use for those with dual diagnosis of mental health and addiction (DiClemente et al., Reference DiClemente, Nidecker and Bellack2008; Nidecker et al., Reference Nidecker, DiClemente, Bennett and Bellack2008). Similarly, attrition was modestly predicted by pre-contemplation and contemplation stages in those with severe mental health difficulties (Rogers et al., Reference Rogers, Martin, Anthony, Massaro, Danley, Crean and Penk2001). However, these were for vocational and educational courses, not therapy.
A key clinical consideration for a readiness for therapy measure is the length of the measure (Haggerty et al., Reference Haggerty, Siefert, Stoycheva, Sinclair, Baity, Zodan, Mehra, Chand and Blais2014). In busy clinical environments, the need for shorter measures is an important consideration, with existing measures of readiness for therapy being 20 items long (Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009) or Safran et al.’s (Reference Safran, Vallis, Segal and Shaw1986) 1 hour long semi-structured interview. Additionally, previous literature indicates the usefulness of developing instruments designed more specifically for the population of its intended use (Rieger et al., Reference Rieger, Touyz, Schotte, Beumont, Russell, Clarke, Kohn and Griffiths2000) as opposed to more generalised measures of change such as the University of Rhode Island Change Assessment (URICA) scale (Dozois et al., Reference Dozois, Westra, Collins, Fung and Garry2004).
Converging evidence suggests that an instrument that can help assess readiness for therapy for common mental health difficulties would be of benefit: the relationship between stages of change and clinical outcomes (Norcross et al., Reference Norcross, Krebs and Prochaska2011) in some clinical populations (i.e. Hudson and Mac Neil, Reference Hudson and Mac Neil2018; McHugh, Reference McHugh2007) and reviews of drop-out in CBT therapy indicate considering careful patient selection (Fernandez et al., Reference Fernandez, Salem, Swift and Ramtahal2015). The benefits of a measure that predicts engagement and attrition (Joe et al., Reference Joe, Simpson and Broome1998; Westra et al., Reference Westra, Constantino and Antony2016; Westra and Norouzian, Reference Westra and Norouzian2018) include adapting limited therapeutic resources to those most likely (‘ready’) to benefit, increasing overall efficiency of services, and focusing attention on additional support and interventions needed for those not yet at that stage of change.
Two previous measures of readiness for therapy exist for short-term evidence-based psychotherapies in mainstream mental health services. However, the measures are time consuming to administer and no research currently has looked at whether or not Ogrodniczuk et al.’s (Reference Ogrodniczuk, Joyce and Piper2009) Readiness for Psychotherapy Index predicts therapy outcomes and Safran et al.’s (Reference Safran, Vallis, Segal and Shaw1986) Readiness for Therapy Questionnaire did not predict attrition rate from therapy (Renaud et al., Reference Renaud, Russell and Myhr2014). This paper describes the development and initial psychometric properties of the Readiness for Therapy Questionnaire (RTQ) in a primary care psychological therapies service. Directions for future research and clinical implications are also considered.
Method
Design
The RTQ was produced by psychological therapists and researchers in collaboration with patients from Talking Change (Solent NHS Trust). Talking Change is the primary care psychological therapy service in Portsmouth, UK. The service is a local IAPT provider. Talking Change offers a range of evidence-based therapies to adults experiencing mood and anxiety disorders (see Table 1 for a list of therapies offered and diagnoses treated).
Table 1. Therapy type and diagnosis of sample

The RTQ was developed and validated in five phases across two Quality Improvement Service Evaluations. The evaluations were approved by the Academy of Research & Improvement (Solent NHS Trust) because they were a formal review of the standard clinical practices (e.g. assessing patient readiness for therapy) and usual service procedures (e.g. eliciting patient feedback, analysis of patient data) at Talking Change. All patients in the service are provided with information about the use of their data, including national reporting, and all patients are given the opportunity to opt out and remove their data from such analyses.
Identifying factors of readiness for therapy
In phase 1, the research team sought to understand factors associated with readiness for therapy from the patient perspective. Patients who completed therapy or dropped out before the end of therapy were telephoned as routine service procedure within a month of their discharge and invited to give feedback about the therapy they had received. In line with national IAPT guidance, therapy drop-out was classified as a patient who attended two or more therapy sessions and discontinued therapy without providing a reason. Patients who attended two or more sessions and finished therapy on the agreed date were defined as completed (The National Collaborating Centre for Mental Health, 2020). A semi-structured interview was used to elicit patient experience of therapy, their reasons for dropping out (if applicable), and their recommendations for service improvement. Patient feedback was transcribed at the point of collection. The transcriptions obtained from January 2016 to January 2017 were collated, and a thematic analysis was conducted (see Ghaemian et al., Reference Ghaemian, Ghomi, Wrightman and Ellis-Nee2020).
In phase 2, the research team reviewed the following databases for published articles between 1988 and January 2017 that validated a measure of readiness for psychological therapy with a clinical population in a mental health setting: Embase, Your Journals@Ovid, and Journals@Ovid Full Text. The search yielded one study by Ogrodniczuk et al. (Reference Ogrodniczuk, Joyce and Piper2009). Ogrodniczuk and colleagues developed a 20-item measure, and proposed four factors associated with readiness for therapy: interest, perseverance, openness and distress.
The research team synthesised their themes with the study by Ogrodniczuk et al. (Reference Ogrodniczuk, Joyce and Piper2009). Twelve themes associated with readiness for therapy were identified: (1) willingness – an intention to try things even when it feels uncomfortable; (2) urgency – therapy is needed as soon as possible to reduce suffering; (3) change – an intention to make positive adjustments; (4) acceptance – an intention to tolerate difficult thoughts and feelings; (5) openness – an intention to try things despite initial scepticism; (6) perseverance – an intention to work through difficulty and continue therapy until the end; (7) locus of control – responsibility for the outcome of therapy is assumed; (8) commitment – an intention to practise or complete things in between sessions; (9) importance – therapy is prioritised and session time is protected; (10) cognitive flexibility – an intention to cultivate new perspectives; (11) expectations – the realistic assumption that the benefits of therapy tend to come over time; and (12) motivation – the decision to attend therapy has been made independently.
The Readiness for Therapy Questionnaire (RTQ)
In phase 4, the RTQ was developed by the research team in consultation with the therapists from the clinical teams. As the RTQ was planned to be completed alongside other routine clinical measures, we sought to reduce overall questionnaire burden by developing a measure that would contain fewer items than the measure by Ogrodniczuk and colleagues (Reference Ogrodniczuk, Joyce and Piper2009).
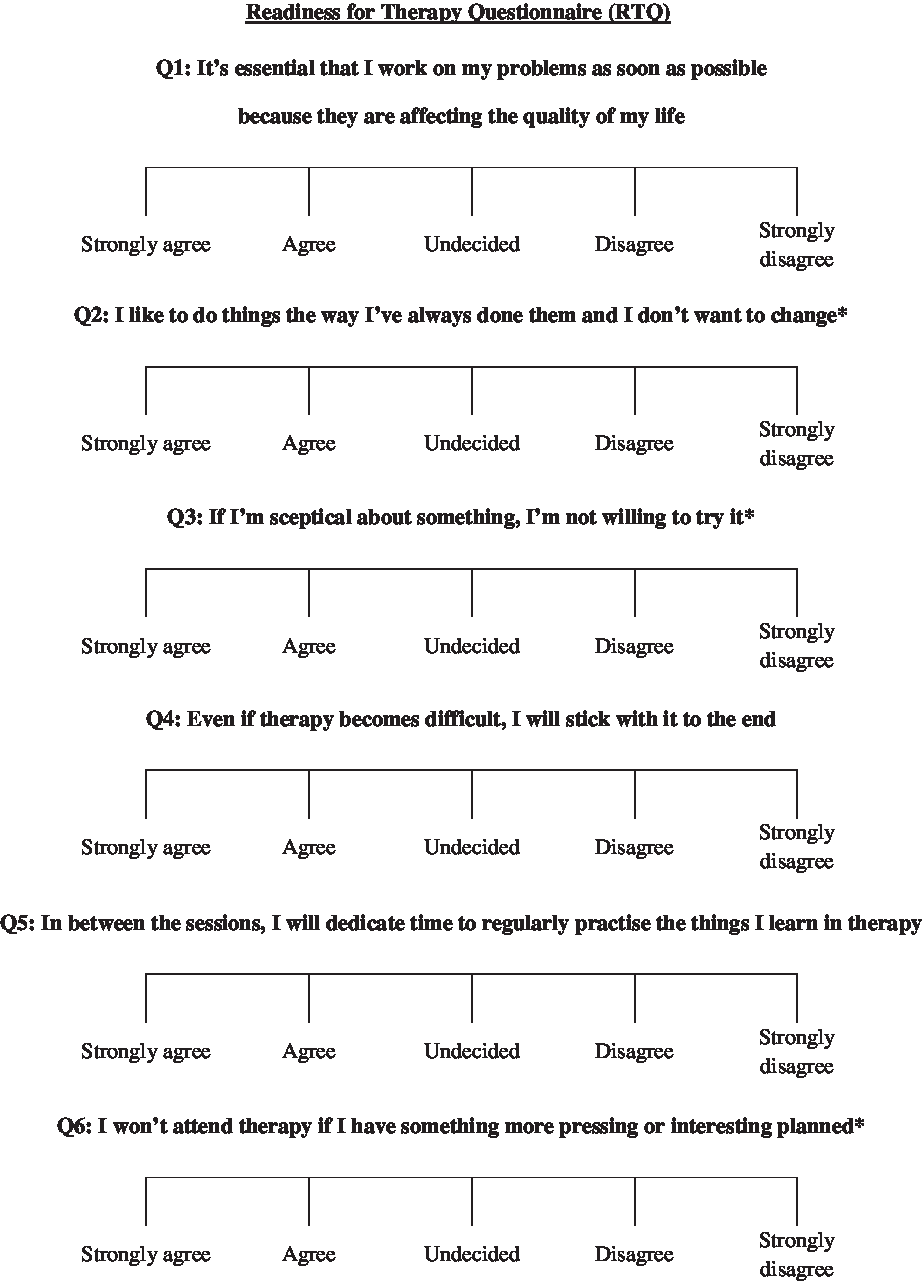
The RTQ consisted of 12 items, an item per theme, a 5-point Likert scale ranging from strongly disagree (0) to strongly agree (4), and an equal number of alternating forward and reverse scored items. A higher score indicated greater readiness for therapy. We planned to assess if the number of items could be reduced by examining which items were most strongly associated with clinical outcomes. The final 6-item RTQ is shown in Fig. 1.
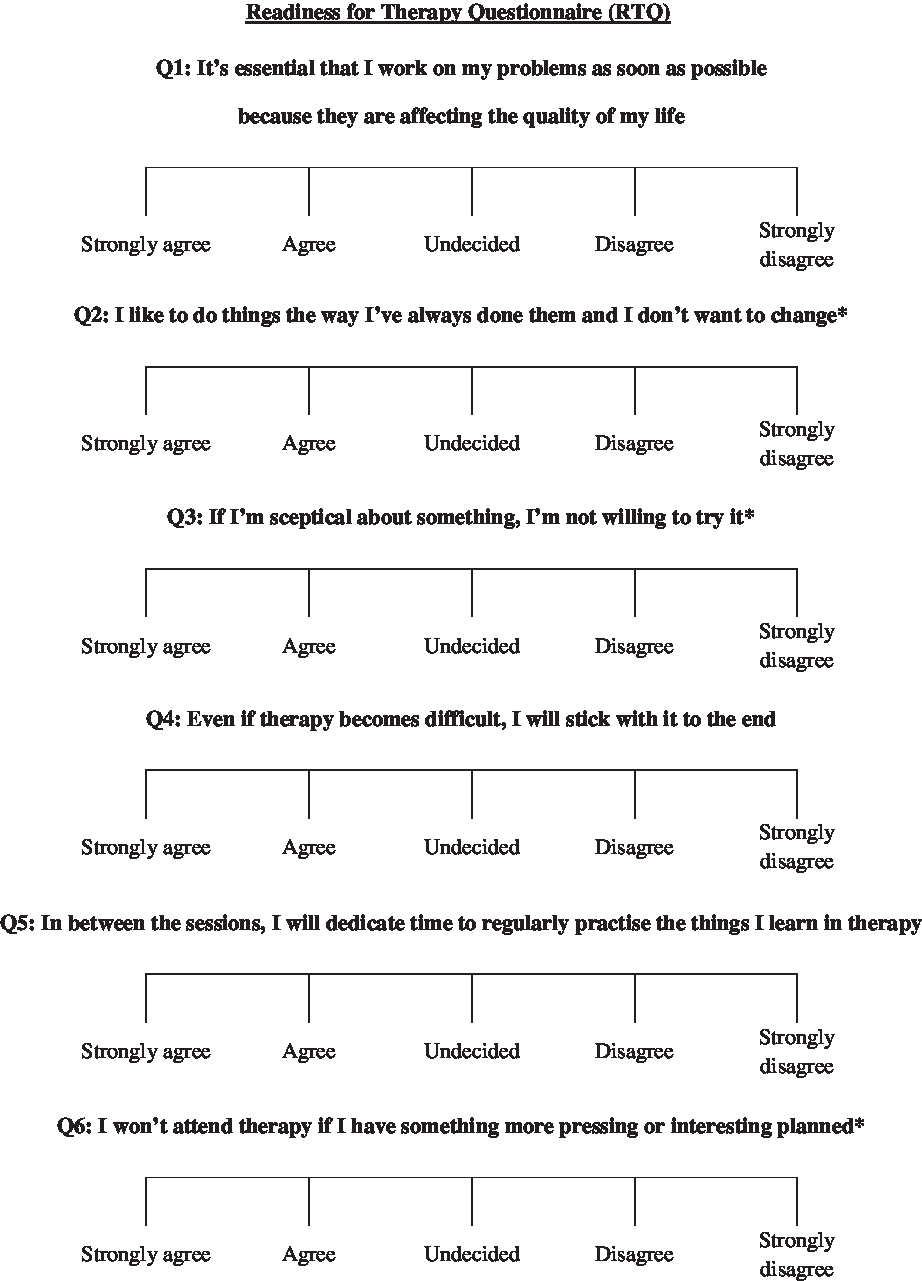
Figure 1. The 6-item Readiness for Therapy Questionnaire (RTQ). An asterisk indicates items reverse scored.
Procedure: examining predictive utility
The GAD-7 (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006) and PHQ-9 (Kroenke et al., Reference Kroenke, Spitzer and Williams2001) were administered at each therapy session as per routine clinical practice. Therapy engagement (completed or dropped out) was reviewed in addition to clinical outcomes on GAD-7 and PHQ-9 scores from pre-therapy to post-therapy. These clinical outcomes were used to assess whether RTQ scores at pre-therapy treatment predicted therapy drop-out and recovery. In line with other IAPT services, recovery or ‘below caseness’ was defined as scoring ≤9 on the PHQ-9 and ≤7 on the GAD-7 at post-therapy treatment after scoring above these scores on either measure at pre-therapy (The National Collaborating Centre for Mental Health, 2020). Footnote 1
Participant characteristics
All participants received an assessment and a ‘provisional diagnosis’ by therapists from the clinical teams, using the overview and screener modules of the Structured Clinical Interview for the DSM-IV (American Psychiatric Association, 1994) for Axis I disorders (SCID-I; First et al., Reference First, Gibbon, Spitzer and Williams1996) and Axis II disorders (SCID-II; First et al., Reference First, Gibbon, Spitzer, Williams and Benjamin1997).
Participants who were provisionally diagnosed with a mood or anxiety disorder and therefore met the referral criteria for treatment within a primary care psychological therapy service were offered treatment in the service. Participants whose main presenting problem was an Axis 2 disorder (e.g. psychotic disorders, personality disorders) were not included in the study, and instead were signposted to the local secondary care mental health team.
Data were collected from 349 participants. Participants were 69.6% (n = 243) female and 30.4% (n = 106) male. Ages ranged from 18 to 77 years, with a mean of 37.1 years. Participants reported their ethnicity as follows: 90.5% (n = 314) White; 5.7% (n = 20), another ethnicity; and 4.3% (n = 15) did not report their ethnicity. All participants scored ‘above caseness’ at pre-therapy treatment. Table 1 displays the therapy type participants received and their provisional diagnosis.
Data analysis
Participants who had missing data for half or more of the items on the RTQ were excluded (n = 15). The sample mode response replaced items of missing data. There were no missing data on the PHQ-9 and GAD-7. Kolmogorov–Smirnov tests were significant for PHQ-9 and GAD-7 total scores, and RTQ total and subscale scores. Kurtosis and skewness were within the normal range on the RTQ, PHQ-9 and GAD-7 (–2 to +2), and the histograms for each measure appeared normal. Thus, the data were declared as normally distributed.
Results
56.2% (n = 196) of the sample completed therapy and 43.8% (n = 153) dropped out. 50.1% (n = 175) of the sample were recovered on both the PHQ-9 and GAD-7 post-therapy. There was a reliable improvement in both the PHQ-9 (reduction of 6 or more points) and GAD-7 (reduction of 4 or more points) for 58.5% (n = 204) of participants. There was a reliable reduction in both the PHQ-9 (increase of 6 or more points) and GAD-7 (increase of 4 or more points) for only 1.1% (n = 4) of participants.
Reliability and scale reduction
Total scores on the 12-item RTQ ranged from 20 to 48 out of 48 with a mean of 35.5 (SD = 4.8), a median of 35 and a mode of 33. Internal consistency for the total score was acceptable: α = .73.
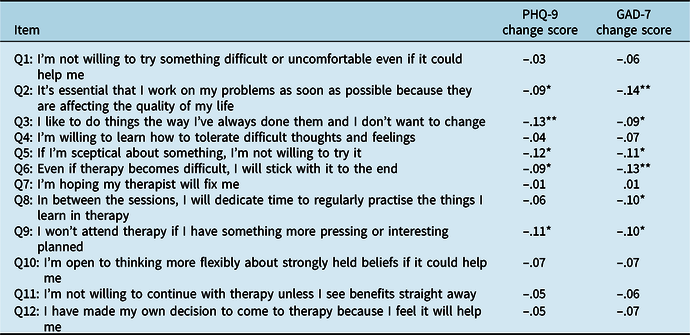
In order to reduce the number of items for the measure, responses to the individual questions were correlated with changes in PHQ-9 and GAD-7 scores across therapy (see Table 2). The PHQ-9 change score significantly correlated with question 2: r = –.09, p < .05; question 3: r = –.13, p < .01; question 5: r = –.12, p < .05; question 6: r = –.09, p < .05; and question 9: r = –.11, p < .05. The GAD-7 change score significantly correlated with question 2: r = –.14, p < .01; question 3: r = –.09, p < .05; question 5: r = –.11, p < .05; question 6: r = –.13, p < .01; question 8: r = –.10, p < .05; and question 9: r = –.10, p < .05. These questions which correlated with both or either change scores where then used to develop a 6-item measure. This is shown in Fig. 1.
Table 2. Correlations between the 12-item RTQ with PHQ-9 and GAD-7 change scores
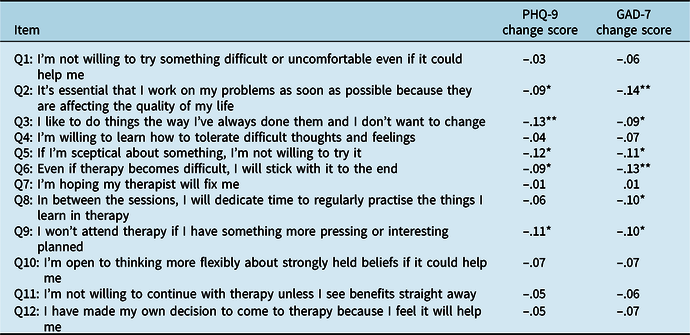
Change scores from post-therapy to pre-therapy; *p < .05, **p < .001.
Total scores on the 6-item RTQ ranged from 10 to 24 out of 25 with a mean of 18.4 (SD = 2.8), a median of 18 and a mode of 17. The Cronbach’s alpha for the 6-item measure was α = .63. Above .6 has been suggested as acceptable for short measures, and mean inter-item correlation was .24. The correlation with the 12-item measure was high: r = .90.
Correlations
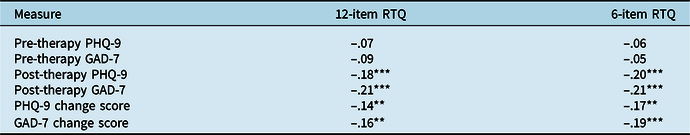
Table 3 presents the correlations between the 12-item and 6-item RTQ with PHQ-9 and GAD-7 scores pre-therapy, post-therapy and change scores (post-therapy to pre-therapy). Please note that the correlations are for all participants whether they were deemed completed or dropped out of therapy, as measures were completed at every session.
Table 3. Correlations between the 12-item and 6-item RTQ with PHQ-9 and GAD-7 scores pre-therapy, post-therapy and change scores
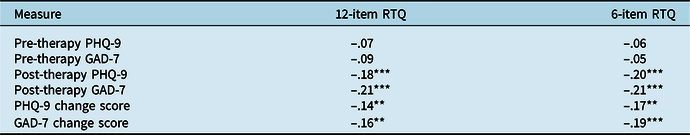
One-tailed Pearson’s correlations. Change scores from post-therapy to pre-therapy; **p < .01, ***p < .001.
The 6-item measure was therefore used for the rest of the analyses. Both the 6- and 12-item version did not correlate with pre-scores but significantly correlated with pre- and change scores for both the PHQ-9 and GAD-7. The correlations for the 6-item measure were slightly higher than for the 12-item version, so the 6-item measure was therefore used for the remaining analyses.
Logistic regression: predictors of outcomes
A hierarchical linear regression was conducted to see whether the RTQ and subscale predicted clinical outcome after controlling for demographic variables (gender, age, ethnicity) and baseline PHQ-9 and GAD-7 scores. There were three clinical outcomes analysed separately:
-
Therapy completion (completed vs dropped out);
-
Recovered on both the PHQ-9 and GAD-7 post-therapy;
-
Having a reliable improvement in scores on both the PHQ-9 and the GAD-7 post-therapy.
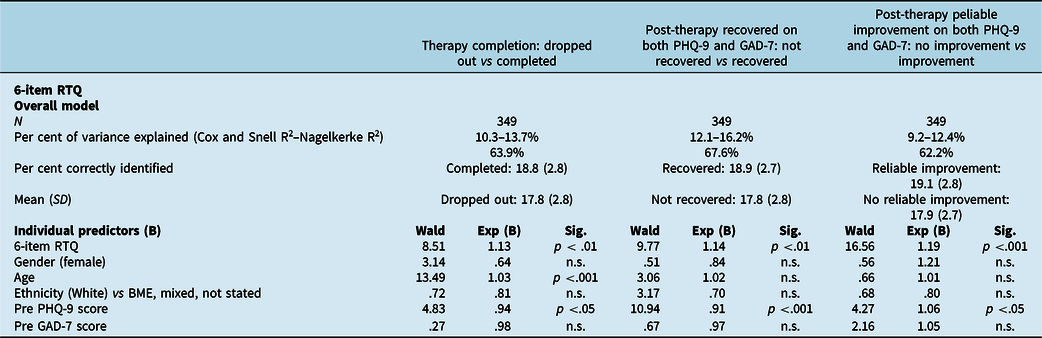
There were not enough participants who had a reliable deterioration to see whether the RTQ predicted this. The results are shown in Table 4. All outcomes of therapy completion, being recovered post-therapy on both PHQ-9 and GAD-7 and having a reliable improvement in scores on both PHQ-9 and GAD-7 post-therapy were significantly predicted by the 6-item RTQ, after controlling for demographics and baseline PHQ-9 and GAD-7 scores.
Table 4. Regression results: pre-therapy 6-item RTQ predicting therapy completion, and post-therapy reliable improvement and recovery on PHQ-9 and GAD-7
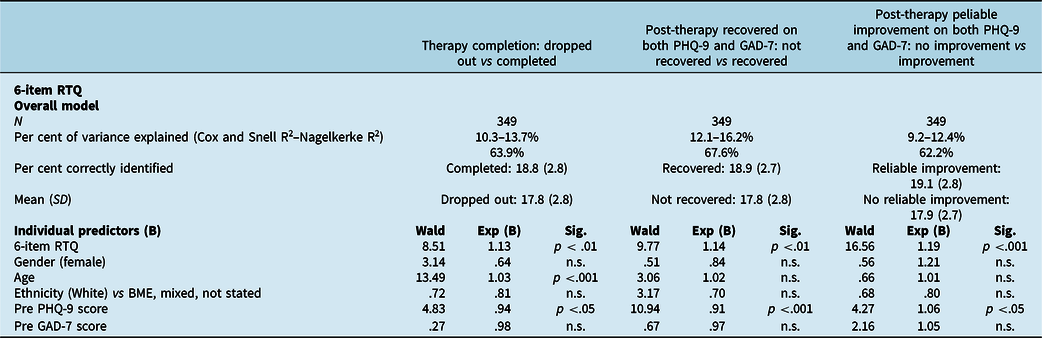
Dummy variables are shown in parentheses. n.s., non-significant.
Cut-off point: ROC curve analysis
A receiver operating characteristic (ROC) curve was used to see if there was a cut-off to predict the clinical outcome variables by scores on the 6-item RTQ. An equal weight was placed on specificity and sensitivity.
For drop-out vs completion of therapy, the 6-item RTQ had 59.8% within the ROC curve. The best balance between specificity and sensitivity was achieved by a score of 19 or more which identified those who completed therapy with a sensitivity of .53 and a specificity of .63. For recovery on both PHQ-9 and GAD-7 post-therapy, the 6-item RTQ had 60.6% within the ROC curve. The best balance between specificity and sensitivity was achieved by a score of 19 or more which identified those who recovered with sensitivity of .53 and a specificity of .61. For reliable change on both the PHQ-9 and GAD-7 post-therapy, the 6-item RTQ had 62.9% within the ROC curve. The best balance between specificity and sensitivity was achieved by a score of 19 or more, which identified those who recovered with sensitivity of .57 and a specificity of .62.
Discussion
This study aimed to develop a measure to assess readiness to change prior to psychological therapy and assess its potential utility in predicting clinical outcomes. The development phase suggests acceptability with patients and face validity with clinicians. The results suggest RTQ scores could potentially predict whether or not patients are likely to drop out of therapy. Furthermore, high RTQ score significantly predicted recovery, i.e. completing therapy with GAD-7 and PHQ-9 scores within the recovered range, and reliable improvement, a reduction of 6 points on PHQ-9 and 4 points on GAD-7. This result held even after controlling for demographics and baseline symptom severity.
The development of the RTQ was influenced by the Readiness for Psychotherapy Index (Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009) a measure designed for assessing readiness for therapy. To the best of the authors’ knowledge, the Readiness for Psychotherapy Index has not yet been shown to be a predictor of attrition in therapy or clinical outcome. At 20 items, the Readiness for Psychotherapy Index was considered to be too long to use in busy clinical settings, such as the IAPT service, where a number of other measures are required to be administered. Thus, a shorter measure which can be shown to predict clinical outcome and drop-out was considered as having better clinical utility. A 12-item RTQ was initially designed and was further shortened to a 6-item measure. The shorter version of RTQ showed acceptable reliability and had a slightly stronger correlation with recovery on PHQ-9 and GAD7 in comparison with the 12-item RTQ. The overall RTQ score did not correlate with depression and anxiety symptoms pre-therapy. This suggests a limited impact of symptom severity on motivation to change: a previous study in a primary care psychological therapies service did not show an impact of distress level on initial appointment attendance (Murphy et al., Reference Murphy, Mansell, Craven, Menary and McEvoy2013). However, RTQ total scores correlate with lower depression and anxiety scores, and total scores correlated with greater reductions in symptomatology across the course of therapy.
The Cronbach’s alpha of the 6-item RTQ (α = .63) was below the .7 generally suggested as acceptable. However, a low alpha can result from a low number of items such as in this case (Tavakol and Dennick, Reference Tavakol and Dennick2011); the inter-item mean correlation of .24 is within the range of .15 to .50 suggested as acceptable by Clark and Watson (Reference Clark and Watson1995).
The RTQ total pre-therapy score was significantly higher for those with a positive clinical outcome, which is in line with previous studies showing a correlation between readiness and outcome in treatment for anorexia nervosa (i.e. Hudson and Mac Neil, Reference Hudson and Mac Neil2018; McHugh, Reference McHugh2007) and readiness and engagement/retention for addiction treatment (Joe et al., Reference Joe, Simpson and Broome1998). Previous studies have found predictors of poor clinical outcome such as personality disorder symptoms scores (Goddard et al., Reference Goddard, Wingrove and Moran2015) and attention control (Buckman et al., Reference Buckman, Saunders, Fearon, Leibowitz and Pilling2019); however, this is the first time a measure specially about readiness for change has been shown to predict clinical outcomes.
However, despite the statistically significant differences in scores on the RTQ based on clinical outcomes, there was poor sensitivity and specificity for the measure in predicting these same outcomes. This was probably due to the small difference between the mean scores of positive and negative clinical outcomes. Thus, it is not possible at this point to develop a cut-off point for the RTQ which could be used to predict positive or negative clinical outcome at the point of assessment. It may therefore be more helpful to use this measure as a continuous measure of readiness with associated score ranges (for example low, average, high), rather than a single cut-off classifying into two binary positive and negative outcomes. Such a use of the RTQ could mean reductions in scores signifies clinical change more than just above or below a cut-off point. The strong correlations between the RTQ and change scores in this study would indicate this as a potential use.
A possible clinical implication of the RTQ measure is to use it in conjunction with a broader clinical assessment of motivation and suitability, and the answers from the questions being used to generate a clinical discussion about potential barriers to therapy and possible ways to overcome these. Alternatively, the RTQ can be used to assess the benefit of offering motivational interviewing (MI) as a precursor, or an adjunct, to treatment as usual. MI principles can often be offered as part of treatment as usual; however, our results indicate that greater attention to readiness for change and addressing motivational factors can potentially make a significant difference to patients’ outcomes. This is consistent with previous research that showed combining MI with evidence-based psychological therapies can help reduce drop-out and in turn potentially enhance clinical outcomes given the overlap between engaging with, and completing treatment, and clinical recovery (Westra et al., Reference Westra, Constantino and Antony2016; Westra and Norouzian, Reference Westra and Norouzian2018). Engaging patients with therapy when they present with complex mental health difficulties can sometimes be extremely challenging for patients and therapists alike. Thus, having the ability to assess capacity and readiness for therapy from the outset could prevent rushing through the process of change, which in turn could affect the alliance, and help with collaboratively agreeing realistic goals from the outset. This is particularly relevant when working with chronic, long-standing and hard-to-treat clinical presentations such as severe anxiety or depression, or anxiety and depression in the context of other difficulties such as autism and spectrum disorder, long-term health conditions and Axis II disorders. Further research is needed to look at potential clinical application of RTQ for these presentations.
There are several limitations that need to be considered. This study analysed outcomes from only one service. There was limited ethnic diversity. Future research is needed to determine if the predictive utility of the RTQ varies based on variables such as gender, age and ethnicity. Similarly, it will also be helpful to measure the mean and range of number of sessions attended in future research to see if the application of RTQ is enhanced, in part, as a function of the duration of treatment. The convergent validity of the RTQ compared with the Readiness for Psychotherapy Index (Ogrodniczuk et al., Reference Ogrodniczuk, Joyce and Piper2009) was not established in this study. Future research should include both measures in order to determine correlations between the two and compare their predictive efficiency. It is unknown if the results would hold for other intervention types, such as computer-based CBT. It might be that the RTQ has different outcomes for different therapies and problems but there was an insufficient sample size in the current study to examine such potential differences. It also remains to be seen whether the RTQ predicts clinical outcomes in secondary care or more specialised psychological therapies services. More research is needed in other settings with different clinical populations to see if our result can be replicated. Future research could assess if addressing motivational factors can change the RTQ score and if this leads to enhanced clinical outcomes. Furthermore, it will be helpful to compare the impact of adding MI as a pre-cursor to psychological treatment versus addressing RTQ as ongoing part of therapy on clinical outcomes.
Despite these limitations this study has developed a Readiness for Therapy Questionnaire that predicts clinical outcomes in a primary care psychological therapy service. Future research with a larger sample in a range of services would help further demonstrate utility and develop the measure, including trying to increase the sensitivity and specificity to establish a cut-off score.
Acknowledgements
None.
Financial support
None.
Conflicts of interest
None.
Ethics statement
The authors of this paper have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS throughout this study.
Data transparency
Three of the current authors of this manuscript have published a qualitative paper (Ghaemian et al., Reference Ghaemian, Ghomi, Wrightman and Ellis-Nee2020), where the data have been extracted from the same sample as this manuscript, albeit with a different focus. The current manuscript is looking at the validity of RTQ and whether or not RTQ can predict outcome and drop-out, whereas the qualitative paper is focusing on patients’ subjective experience of therapy and reasons for discontinuation from therapy.




Comments
No Comments have been published for this article.