Introduction
A long-term health condition (LTC) defines any health condition that can be managed, but not cured (IAPT, 2014a). Examples include diabetes, chronic heart disease, asthma and chronic obstructive pulmonary disease. Medically unexplained symptoms (MUS) is an umbrella term used to describe sets of physical symptoms that cannot be explained by disease specific and observable biomedical pathology (IAPT, 2014a). Examples include irritable bowel syndrome, fibromyalgia and chronic fatigue. There are many issues, tensions and debate surrounding the sensitivity and complexity of language in MUS. LTC patients are the most frequent users of health care services, as 30% of the general population suffer from one or more LTC (Department of Health, 2011a). More than a quarter of Primary Care patients present with unexplained pain, IBS or chronic fatigue (Aggarwal, McBeth, Zakrzewskai, Lunt and McFarlane, Reference Aggarwal, McBeth, Zakrzewskai, Lunt and McFarlane2006), with associated excess costs comparable to that of depression or anxiety disorders (Konnopka et al., Reference Konnopka, Schaefert, Heinrich, Kaufmann, Luppa and Herzog2012). Mood disturbance in the context of LTC/MUS can impact on self-care and self-management regimes/capabilities, which reciprocally increase healthcare use, cost and distress (Edege and Ellis, Reference Egede and Ellis2010).
In terms of trying to help LTC/MUS patients, when GP-patient interactions have been targeted for change, consultation communication patterns do change, but do not then subsequently alter patient outcomes (Morris et al., Reference Morris, Dowrick, Salmon, Peters, Dunn and Rogers2007). Specific cognitive-behavioural interventions have therefore been developed and tested that target reducing LTC/MUS symptoms. There is an increasing body of evidence that supports the use of adapted CBT across a range of LTCs (Sage, Sowden, Chorlton and Edeleanu, Reference Sage, Sowden, Chorlton and Edeleanu2008) and MUS (Deary, Chalder and Sharpe, Reference Deary, Chalder and Sharpe2007). Specific examples in LTC include CBT for type-2 diabetes (Ismail, Winkley and Rabe-Hesketh, Reference Ismail, Winkley and Rabe-Hesketh2004; Wroe, Rennie, Gibbons, Hassy and Chapman, Reference Wroe, Rennie, Gibbons, Hassy and Chapman2015), oncology (Hopko and Coleman, Reference Hopko and Colman2010) and multiple sclerosis (Moss-Morris and Wearden, Reference Moss-Morris and Wearden2013). In MUS, randomized control trials (RCT) in irritable bowel syndrome (Moss-Morris, McAlpine, Didsbury and Spence, Reference Moss-Morris, McAlpine, Didsbury and Spence2010) and chronic fatigue (Chalder, Wallace and Wessley, Reference Chalder, Wallace and Wessley1997) demonstrate efficacy and particularly the use of pacing as a helpful technique. However, in the White et al. (Reference White, Goldsmith, Johnson, Potts, Walwyn and Decesare2011) RCT the adaptive pacing arm did not perform as well in terms of fatigue and functioning outcomes compared to graded exercise or CBT. The recent Marquis, de Gucht, Gouveia, Leal and Maes (Reference Marquis, de Gucht, Gouveia, Leal and Maes2015) meta-analysis of 16 pacing RCTs in chronic fatigue found significant small to medium effect sizes across all outcomes at end of treatment and follow-up, with the largest effect sizes for reduced severity of fatigue. Research demonstrates significant physical improvements following CBT for individuals with chronic pain (Gatchel, Peng, Peters, Fuchs and Turk, Reference Gatchel, Peng, Peters, Fuchs and Turk2007) and chronic fatigue (Flo and Chalder, Reference Flo and Chalder2014). In terms of 3rd wave approaches, use of acceptance and commitment therapy (ACT) has been demonstrated to be effective (albeit typically in uncontrolled studies) in terms of enhancing adjustment across a wide range of LTCs such as chronic pain, cancer, epilepsy, diabetes, obesity, tinnitus and multiple sclerosis (Dewhurst, Novakova and Reuber, Reference Dewhurst, Novakova and Reuber2015; McCracken and Vowles, Reference McCracken and Vowles2014).
In February 2011, the UK Government published No Health Without Mental Health, setting out the service development priority of the expansion of the IAPT programme to include people with LTC/MUS (Department of Health, 2011b). Wroe et al. (Reference Wroe, Rennie, Gibbons, Hassy and Chapman2015) highlighted that as IAPT services were being expected to offer interventions for LTC/MUS, this signalled a degree of patient complexity. A key challenge for IAPT services is therefore to test the evidence as to whether interventions delivered at step 2 (PWP) and step 3 (High Intensity Therapies) are clinically effective for anxiety and depression in an LTC/MUS context. This current research therefore details the developments, processes and outputs from the Sheffield LTC/MUS Pathfinder Site concerning depression and anxiety outcomes for LTC/MUS patients seen within a standard IAPT service. The research aims were as follows: (1) to describe and examine the organizational impact of a new stepped-care model of service delivery; (2) to evaluate whether interventions were effective in improving anxiety and depression; and (3) to benchmark outcomes for LTC/MUS patients against routine IAPT patients.
Method
Study samples
This study was based on the retrospective analysis of routinely collected outcomes for patients with LTC/MUS accessing the IAPT service during the Pathfinder initiative. Outcomes were analysed for LTC/MUS patients who were referred to and treated within the IAPT service between September 2012 and April 2013. All referrals were made by GPs who recognized the need for psychological intervention due to mental health issues (i.e. anxiety and depression) being implicated in poor LTC/MUS self-management. Psychological treatment was defined by attending at least one treatment session, following an initial suitability screening appointment. Suitability was ascertained via a 45-minute face-to-face assessment with a Psychological Well-Being Practitioner (PWP). Screenings were structured using an adapted version of the Reachout clinical assessment guidelines (Richards and Whyte, Reference Richards and Whyte2009). Adaptations included expanded assessment of somatic symptoms and problem statements reflecting the poor coping with (and associated impact of) the LTC/MUS. Conditions meeting the criteria for LTC or MUS were determined by using the National LTC/MUS Pathfinder categorization. Feedback from IAPT practitioners stated that the typical MUS presentations referred were chronic fatigue syndrome, fibromyalgia and irritable bowel syndrome. No formal record was made of the specific LTC or MUS.
Stepped care service design
The stepped-care model developed is detailed in Figure 1. At step one, appropriate LTC/MUS patients were either referred or GPs employed watchful waiting. Patients were seen initially in step 2 (PWP) and then stepped up to step 3 (CBT, ACT and counselling) should the assessment of the PWP identify sufficient need, or when patients had been unresponsive to guided self-help. At step 2, PWPs treated those LTC/MUS patients that screened positive for the presence of depression or an anxiety disorder and whose symptoms were in the mild to moderate range. Step 2 interventions were also offered to LTC/MUS patients with recent onset severe depression and anxiety – but in the absence of significant risks regarding self-neglect or suicide. Treatments offered at step 2 were the extant guided self-help protocols (Richards and Whyte, Reference Richards and Whyte2009), motivational interviewing (MI) or pacing (via a manual written for the purposes of the project). The decision to offer pacing across LTC/MUS presentations was based on pacing being a behaviourally based intervention, that could fit well with the guided self-help PWP clinical method. The decision to offer MI was based on the evidence from four meta-analyses (Lundahl and Burke, Reference Lundahl and Burke2009), which show MI as effective in increasing client engagement in treatment and this was considered particularly important in an LTC/MUS context. Pacing could therefore be considered as a suitable intervention across the range of MUS presentations seen at step 2. PWPs (N = 36) received two days MI and pacing training. The pacing manual supported PWPs in their psychoeducational “coaching” role and was not a departure from the low intensity approach. PWP interventions were brief and lasted between 1–6 (30-35 minute) 1-2-1 sessions (IAPT, 2011).

Figure 1. Stepped care psychological service model for LTMCs/MUS IAPT Pathfinder Pilot
Treatments delivered at step 3 were CBT, ACT or counselling. CBT treatments were typically up to 20 sessions and the CBT delivered followed IAPT approved treatment protocols for depression and anxiety (Roth and Pilling, Reference Roth and Pilling2007). CBT staff (N = 30) also received 2-days of experientially-based training on ACT for LTC/MUS, delivered by experienced ACT trainers/practitioners. ACT treatment duration contracts were up to 20 sessions. N = 28 counsellors received two days training on revisiting and enhancing the Rogerian core conditions of effective counselling during the treatment of LTC/MUS patients. Counselling at Step 3 was also delivered in an up to 20-session format. Counselling training focused on the manner in which counsellors could acknowledge the physical factors in the LTC/MUS patient's presentations, whilst retaining the core Rogerian conditions. Training across each of the steps had a consistent element of education about LTC/MUS (e.g. common elements of LTC/MUS impact, epidemiology, co-morbidity and phenomenology). Training emphasized that existing PWP, counselling and CBT interventions could be delivered with LTC/MUS patients if the assessment indicated that this could be effective. Satisfaction data were generally high across the three types of training and these data are available from the first author. Step 4 entailed clinical health psychologists providing a complex case consultation service (GPs could access this service), providing clinical supervision and also treatment of complex cases. A pilot group of GPs also attended workshops on Primary Care recognition and management of LTC/MUS patients. All IAPT practitioners (PWPs, counsellors and CBT staff) had access to regular LTC/MUS group supervision to reinforce the lessons learnt from the training, reflect on their practice, provide support and reduce therapeutic drift.
Outcome measures
This study was based on two self-report outcome measures that form a part of the IAPT minimum dataset (IAPT, 2011). The Patient Health Questionnaire-9 (PHQ-9) is a case-finding and outcome measure for depression (Kroenke, Spitzer and Williams, Reference Kroenke, Spitzer and Williams2001). The PHQ-9 provides banded severity ratings (full range 0–27) with a cut-off score for the detection of depression being a score ≥10 (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). The PHQ-9 has been well validated demonstrating adequate sensitivity and specificity (Kroenke, Spitzer, Williams and Lowe, Reference Kroenke, Spitzer, Williams and Lowe2010; Kroenke et al., Reference Kroenke, Spitzer and Williams2001). The GAD-7 is a case-finding and outcome measure for generalized anxiety, social phobia, PTSD and panic disorder (Spitzer, Kroenke, Williams and Lowe, Reference Spitzer, Kroenke, Williams and Lowe2006; Kroenke, Spitzer, Williams, Monahan and Lowe, Reference Kroenke, Spitzer, Williams, Monahan and Löwe2007). The GAD-7 provides banded severity ratings (full range 0–21) and a cut-off score ≥ 8 detects an anxiety disorder with adequate sensitivity and specificity.
Analysis strategy
The first phase involved the description of LTC/MUS patient traffic through the stepped-care model of service delivery. The second stage involved investigation of patient outcomes according to LTC or MUS presentation and step of service. Demographic and outcome data included all LTC/MUS patients seen in the IAPT service (e.g. completed treatment, dropped-out, sign-posted to other services) during the evaluation period and for whom assessment and final outcome scores were available. Patients seen at step 3 had their outcomes removed from the step 2 cohort analyses. Dropout was defined as any unscheduled termination of treatment by the patient, recorded by practitioners. Reasons for dropout were not recorded.
Categorical outcomes were calculated for the PHQ-9 and the GAD-7 using the national IAPT metrics for calculating change (IAPT, 2014b). The following categories were used: (a) moving to recovery counted patients above the clinical cut-off before intervention and below following intervention. A patient was a “case” when they scored above the clinical threshold on depression and/or anxiety before intervention (i.e. PHQ-9 score ≥10 at assessment and/or GAD-7 ≥8 at assessment). Moving to recovery occurred when the final outcome score was below the clinical threshold on depression and anxiety (i.e. PHQ-9 score <10 at termination and GAD-7 <8 at termination); (b) reliable improvement required that any improvement in outcome scores pre and post intervention exceeded measurement error of the PHQ-9 and GAD-7 using reliable change criteria (RCI; Jacobson and Truax, Reference Jacobson and Truax1991). Reliable improvement was a reduction of ≥6 points on the PHQ-9 or ≥4 points on the GAD-7 (IAPT, 2014b). Conversely, reliable deterioration occurred when any deterioration in outcome scores pre and post intervention exceeded measurement error on the PHQ-9 and GAD-7, again using reliable change criteria (RCI; Jacobson and Truax, Reference Jacobson and Truax1991). Reliable deterioration was an increase of ≥6 points on the PHQ-9 or ≥4 points on the GAD-7 (IAPT, 2014b). (c) A stasis outcome was recorded when there was no movement to recovery and neither reliable improvement or deterioration. (d) reliable recovery required reliable improvement, but the case had to additionally move below the caseness threshold on both outcome measures at the end of treatment. (e) limited recovery requires reliable improvement, but the case only had to additionally move below caseness threshold on a single outcome measure at the end of treatment. (f) a harm outcome was recorded when a patient had a pre–post reliable deterioration on either the PHQ-9 or GAD-7and also moved from non-case to case following intervention. The outcome categories of moving to recovery, reliable improvement, reliable deterioration and reliable recovery are standard IAPT terms (IAPT, 2014b) and are marked with an asterisk in Table 3. Stasis, limited recovery and harm outcome categories were created as additional outcome categories by the research team. In order to contextualize outcomes for LTC/MUS patients, category outcome rates were additionally benchmarked against routine IAPT patients (patients with common mental health problems). Effect sizes on pre–post comparisons were also calculated with partial eta squared.
Results
The flow chart of patients through the stepped care model is presented in Figure 2 which includes the step-up and drop-out rates. A total of N = 844 LTC and N = 172 MUS patients were treated, with LTC referrals out-numbering MUS referrals at a ratio of 4:1. At assessment, N = 99 LTC/MUS patients were deemed not suitable for an IAPT intervention (reasons for unsuitability were not recorded) and were signposted to other services or discharged. In terms of volume of clinical work, 81.81% of patients were treated at step 2 (PWP), 17.03 at step 3 (comprising 8.86% receiving CBT/ACT and 8.17% receiving counselling) and 2.17% of patients at step 4. Overall, 14.46% (N = 147) of patients entering the IAPT service were stepped-up; 19.18% of MUS (N = 33) and 13.50% of LTC (N = 114). N = 125 patients were stepped up from step 2 to step 3 and N = 22 were stepped up from step 3 to step 4. In terms of treatment acceptability, N = 130 (12.8%) of LTC/MUS patients dropped-out of treatment, with the remaining 87.2% completing treatment. There was no significant difference between dropout rates for LTC and MUS (χ² (1) = 2.252, p = .132). The dropout rate during treatment at step 2 for LTC was 9.72% and 2.37% at step 3. The dropout rate during treatment for MUS was 12.79% at step 2 and 3.46% at step 3. There was no significant relationship between health condition and step of service that patients dropped out from (χ² (1) = 0.046, p = .831).

Figure 2. Patient flow through the LTC/MUS stepped-care model
In terms of the uptake of the consultation service, N = 66 consultation requests were made. Table 1 reports the breakdown of consultation requests by step of service and associated outcomes. PWPs were most likely to request consultation, with the most frequent request regarding advice on clinical management issues. Response time was between 1–3 days for 94% of the requests, with consultation provided within 7 days of initial request in 80% of cases.
Table 1. Request source for consultation and subsequent outcome at step 4

No differences were found between health condition (χ² (5, N = 1016) = 10.29, p = .068), gender (χ² (1, n = 1016) = 1.59, p = .207) or ethnicity (χ² (1, n = 909) = 2.11, p = .146) and step of service patients were treated in. The mean age of LTC/MUS patients seen in at step 2 was 48.2 years (SD = 15.57, range 16–89) and 46.5 years (SD = 12.83, range 19–76) at step 3. LTC and MUS patients did not differ in terms of their age (t (309.13) =1.48, p = .139). Mean age for generic IAPT patients at step 2 was 38.9 years (SD = 14.46, range 16–87) and 39.5 years (SD = 14.09, range 17–88) years at step 3. LTC/MUS patients were therefore significantly older than patients seen within generic IAPT services at both step 2 (t (4362) =16.25, p < .001) and step 3 (t (857) = 6.082, p < .001). Fewer males (36%) and more female patients (64%) attended generic IAPT services compared to the LTC/MUS patients at step 2 (χ² (1) = 6.302,p = .12).
Table 2 reports the LTC/MUS case rates at initial assessment according to step of service, with the vast majority of patients reaching caseness on the PHQ-9 and GAD-7. Caseness proportions were significantly higher at step 3 than step 2 for both depression (χ² (1, n = 979) = 6.997, p = .008) and anxiety (χ² (1, n = 935) = 6.416, p = .011). Table 3 also displays assessment benchmarks with generic IAPT patients, indicating that severe depression and anxiety were the most frequent categories.
Table 2. LTC, MUS and generic IAPT caseness rates at assessment analysed by step of service
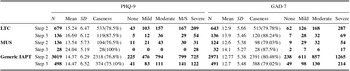
Table 3. Outcome rates for LTC, MUS and generic IAPT patients
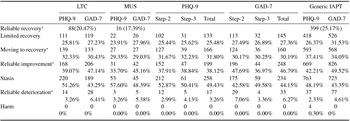
Note: Percentages do not total to 100 % due to some patients being in two outcome categories (i.e. for the recovery plus patients, they are automatically in the recovery group) and that patients needed to be a case at intake to a meet recovery or recovery plus outcome at termination.
Table 3 reports the outcomes for LTC and MUS, with generic IAPT benchmark outcomes. Reliable improvement rates were similar across LTC (39.07%) and MUS (33.70%) for depression, with reliable improvement in anxiety rates higher across LTC (47.14 %) and MUS (45.16%). No difference in reliable improvement rates was found between LTC and MUS for depression (χ² (1) = 0.928, p = .335) or anxiety (χ² (1) = 0.121, p = .728). Moving to recovery rates for depression were 32.33% for LTC and 29.35% for MUS patients. Moving to recovery rates for anxiety were 30.43% for LTC and 29.03% for MUS. No significant differences were found for the moving to recovery rates between MUS and LTC patients for either depression (χ² (1) =0.310, p = .578) or anxiety (χ² (1) = 0.072, p = .789). The limited recovery rate for depression was 25.81% for LTC patients and 23.91% for MUS. There were no significant differences in depression (χ² (1) = 0.144, p = .704) or anxiety (χ² (1) = 0.02, p = .887) limited recovery rates between LTC and MUS patients. The reliable recovery rate for LTC patients was 20.47% and 17.39% for MUS. There was no significant difference in reliable recovery rates (χ² (1) = 0.693, p = .782) between LTC and MUS patients. LTC and MUS deterioration rates were generally low (4.83% for LTC and 4.32% for MUS), with the harm rate being zero.
Moving to recovery rates for depression at step 2 was 31.67% and 32.23% at step 3; there was no significant difference in the moving to recovery rates between the steps (χ² (1) =0.013, p = .908). The anxiety moving to recovery rate was 30.17% for step 2 and 30.25% for step 3 LTC/MUS patients. There was no significant difference between the service steps in terms of these moving to recovery rates (χ² (1) = 0.001, p = .986). There was no significant difference in reliable improvement rates for LTC/MUS depression (χ² (1) = 0.35, p = .852) or anxiety (χ² (1) = 0.590, p = .442) between step 2 and 3.
Reliable improvement rates were higher for generic IAPT patients for both depression (42.21%) and anxiety (49.52%). There was a significant difference in reliable improvement rates between LTC/MUS and generic IAPT patients for depression (χ² (1) = 4.507, p = .034), but not for anxiety (χ² (1) = 3.308, p = .069). There were no significant differences in terms of moving to recovery rates between LTC/MUS and generic cohorts on both depression (χ² (1) = 2.709, p = .1) and anxiety outcomes (χ² (1) = 1.198, p = .274). There was a significant difference in limited recovery rates between LTC/MUS and generic IAPT patients on the PHQ-9 (χ² (1) = 5.367, p = .021), but not for the GAD-7 (χ² (1) = 2.711, p = .1). The reliable recovery rate was correspondingly higher in the generic IAPT service (25.17%) compared to LTC (20.47%) and MUS (17.39%).
Finally, Table 4 documents pre–post mean differences and associated depression and anxiety effect sizes for LTC and MUS patients who completed pre and post measures. Both the LTC and MUS patients improved on the PHQ-9 by a mean of 4.53 and 3.60, creating a large effect size (= 0.35; 0.25). LTC and MUS patients improved on the GAD-7 by a mean of 3.77 and 3.39; this had large effect size (es = 0.32 and 0.31 respectively). For MUS patients there was a significant reduction in depression (t (91) = 5.482, p < .001) and anxiety (t (92) = 6.542, p < .001). For all LTC patients, there was a larger significant reduction in depression (t (429) = 15.33, p < .001) and anxiety (t(436) = 14.064, p < .001). A direct comparison of change for LTC and MUS patients was non-significant for both the PHQ-9 (F(1,528) = 0.328, p = .567) and GAD-7 (F(1,520) = 1.738, p = .188).
Table 4. Pre-post group level change in LTC/MUS patients

Discussion
This study aimed to evaluate the development of a stepped care service delivery model for LTC/MUS patients seen within an IAPT service and to benchmark associated depression and anxiety outcomes. LTC/MUS patients presented with higher PHQ-9 and GAD-7 intake scores and were also less likely to meet IAPT-defined recovery outcomes at discharge than generic IAPT patients. Nevertheless, over a third of LTC/MUS patients showed reliable improvement in either their anxiety and/or depression, and in most instances this was following a low intensity intervention. LTC/MUS dropout rates were low at both step 2 and at step 3. Results provide some initial support for IAPT services being capable of adapting service design and delivery to support the needs of LTC/MUS patients and that the extant IAPT interventions focal to depression and anxiety retain some utility for people living with LTC/MUS.
Staff valued the training, supervision and consultation provided to help them adapt their clinical work. The training at step 3 was not on the specific forms of CBT that exist for MUS, but was rather on ACT and how this could be used to frame and intervene with MUS presentations. There is still a need for IAPT services to develop and evaluate methods to address the physical symptoms of individuals with LTC/MUS and to integrate associated outcome monitoring into performance reporting (Wroe et al., Reference Wroe, Rennie, Gibbons, Hassy and Chapman2015). It has previously been illustrated that a referral to IAPT for LTC patients is associated with a reduction in health care utilization (e.g. fewer sick certificates, fewer admissions to hospital, bed-days and attendance at A&E; de Lusignan et al., Reference de Lusignan, Chan, Tejerina-Arreal, Parry, Dent-Brown and Kendrick2013).
Clinical implications
A far greater proportion of LTC patients were referred in comparison to patients with MUS. Wileman, May and Chew-Graham (Reference Wileman, May and Chew-Graham2001) found that GPs often felt ill-equipped and frustrated when dealing with MUS presentations. Therefore, GPs may have referred less MUS patients due to issues in alliance formation preventing discussion of a potential referral to the IAPT service. Unigwe, Rowett and Udo (Reference Unigwe, Rowett and Udo2014) noted that MUS patients experience a mismatch between their physical problems and being offered a psychological intervention. As “body-based problems” are paired with “body-based solutions”, this may contribute to reluctance (or distrust of) consideration of psychological therapies. The difference in referral rate prompts the consideration of development of dedicated services in IAPT to meet the needs of MUS and LTC as separate patient groups.
The demographic profile of LTC/MUS patients was different to that of traditional IAPT patients, whilst LTC and MUS patients shared many demographic similarities. Significantly more males with LTC/MUS were seen at step 2, and across steps 2 and 3 LTC/MUS patients were significantly older. This finding appears to fit with extant evidence that LTCs increase with age (Naylor et al., 2012). The fact that the LTC/MUS patients tended to be older and male may reflect a context effect, particularly in terms of LTC. South Yorkshire has been identified as an area of disproportionately high incapacity benefit claim rates that reflects the shadow cast by the previous dominance of heavy industry/mining and the physical toll/damage such work creates (Lindsay, Greve, Cabras, Ellison and Kellett, Reference Lindsay, Greve, Cabras, Ellison and Kellett2015). Caseness rates for anxiety and depression for LTC/MUS patients were high and again show the on-going emotional suffering created by living with LTC/MUS (Goodwin, Davidson and Keyes, Reference Goodwin, Davidson and Keyes2009). The mean anxiety and depression scores were higher for MUS patients being seen at step 3 than for patients with LTC. The reasons why this was the case appears unclear and may be related to factors not addressed or measured in the current study.
Moving to recovery and reliable recovery rates were found to be similar across LTC and MUS patient groups and no systematic differences were found in outcomes according to step of service. The notion of “recovery” sits slightly uncomfortably with LTCs, with staff training and supervision championing better condition management and enhanced self-care, rather than recovery. There is a research need across IAPT services to identify predictors of a “stasis” outcome particular to specific interventions and also evaluate interventions specifically aimed at reducing stasis rates. Whilst deterioration rates were low, exploring why some patients experience deterioration whilst receiving interventions demands attention.
Limitations
As this evaluation was based on generating practice-based evidence, many methodological compromises were created. The prime methodological weakness was that LTC/MUS patients were not randomly allocated to interventions and therefore efficacy of interventions was not tested. There was also no formal system for checking the competency of the interventions provided. However, supervision groups did allow practitioners to reflect on their LTC/MUS practice and regular taping of sessions for “live” supervision is a cultural norm within the service. IAPT services do not tend to routinely follow up patients and therefore durability of change was not captured. In terms of the decision to deliver ACT at step 3, the Ost (Reference Ost2008) meta-analysis noted that there was much controlled clinical trial work to be done to ensure that ACT became an empirically validated treatment. Indeed, the choice to deliver MI and pacing at step 2 and ACT at step 3 was somewhat a compromise, as the evidence for these interventions with LTC/MUS populations is still building. Whilst well-evidenced specialist adaptations of high intensity CBT exist for differing forms of LTC and MUS, these are yet to be tested in IAPT services.
A further limitation is that patients were seen because of the depression/anxiety associated with the LTC/MUS, issues related to the management/adjustment to LTC/MUS or a combination of both. Despite these sub-groups naturally existing in the referrals, practitioners did not record the exact reason for referral and therefore appropriate analyses could not be performed. Future IAPT research also needs to explore the reasons why LTC/MUS patients dropout of low and high intensity therapies. Chan and Adams (Reference Chan and Adams2014) have shown for generic IAPT work that there are no differences in terms of the dropout and appointment cancellation rates between step 2 and 3. A major study weakness was that typical self-management treatment targets of LTC/MUS (such as self-care, medication adherence, quality of life and pain management) were not measured. It is acknowledged that indexing depression and anxiety outcomes provided only a partial picture of outcome (Rimes, Wingrove, Moss-Morris and Chalder, Reference Rimes, Wingrove, Moss-Morris and Chalder2014). Future research concerning evaluating system change in IAPT in the care of LTC/MUS needs therefore to consider a wider selection of outcomes and also define a primary outcome measure suitable for use with LTC/MUS (i.e. indexing the physical outcomes of people with LTC/MUS following psychological intervention).
Conclusions
This report has summarized the clinical and organizational outcomes from Pathfinder investment and evidences that stepped-care IAPT services (with appropriate investment and support) can adapt to working with LTC/MUS patients. Extra investment and input via teaching, training and supervision is required to enable IAPT services to offer therapy that is bespoke for people with LTC/MUS. The input into the project of the clinical health psychologists was vital in terms of clinical supervision, teaching/training and sharing specialist experience of LTC/MUS. The input of the IAPT service was vital in terms of ensuring interventions remained within the boundaries of an IAPT service specification. Future and further service investment, research and evaluation are indicated for the LTC/MUS patient group in IAPT services.
Acknowledgements
This work was supported by the DoH LTC/MUS Pathfinder Initiative. With thanks also to Simon Bennett, Rebecca Haines, Deborah Gamsu, Gwyneth De Lacey and Penny Harvey for their work on early drafts and the Pathfinder initiative itself.
Conflict of interest: The authors have no conflicts of interest with respect to this publication, but it is noted that Nic Wilkinson, Paul Bliss and Tom Ayers were all employed by Sheffield Health and Social Care NHS Foundation Trust at the time of the evaluation.









Comments
No Comments have been published for this article.