Introduction
New state-based long-term care (LTC) has been created by welfare states throughout the 20th century, particularly in Europe, to address the increasing number of older adults living with disability under informal care – especially that provided by family members (Mair et al., Reference Mair, Quinones and Pasha2016). However, informal care remains an important part of LTC even in welfare states (Anderson and Hussey, Reference Anderson and Hussey2000). As in other welfare states, a variety of LTC services are available to older adults in Japan, which expanded state-based LTC by implementing the ‘Gold Plan’ in 1990 and introducing LTC insurance in 2000 (Campbell and Ikegami, Reference Campbell and Ikegami2000). In Japan, systematic changes following the launch of LTC insurance have possibly contributed to the promotion of LTC service use. Before LTC insurance was available, LTC services were provided by the social welfare sector. Care from the social welfare sector required that individuals met strict eligibility criteria that were means-tested to target low-income older adults and those living alone.
Further, this care limited LTC services and attached some stigma to using welfare, essentially excluding many older adults who needed LTC services (Yong and Saito, Reference Yong and Saito2012). Reduction of the stigma attached to using LTC services, the introduction of eligibility criteria based on physical and mental status, and the expansion of LTC services, especially community LTC services, began under the provision of universal LTC insurance (Ikegami et al., Reference Ikegami, Yamauch and Yamada2003). As a result, the use of LTC services among older adults has increased. Indeed, the number of older people (per 1,000 insured individuals) aged 65 or older using LTC services provided by LTC insurance doubled between 2000 and 2016: from 73 in 2000 to 138 in 2016 (Ministry of Health, Labour and Welfare, nd-a). Even after the reinforcement of LTC insurance, however, informal care remains the most common source of LTC for older adults living with disability in Japan (Hanaoka and Norton, Reference Hanaoka and Norton2008). According to a nationwide survey conducted in 2001, 79 per cent of LTC was provided by informal care-givers, while community ITC services provided 7 per cent. National surveys in Japan conducted in 2004, 2010, 2013 and 2016 reported similar patterns of preference for LTC (Ministry of Health, Labour and Welfare, nd-b).
While there are data regarding the types of LTC used by older people, differences in their preferences by period remains unclear. It has become increasingly important to explore the differences in LTC preference by period because the need for LTC by older adults can be projected based on their type of LTC preferred by older adults as well as the prevalence of disability (Kane and Kane, Reference Kane and Kane2001; Eckert et al., Reference Eckert, Morgan and Swamy2004). In addition, if gaps between the preference for LTC services and the actual LTC services use in Japanese older adults appear, these findings suggest that the actual LTC service use does not reflect LTC preference among older adults.
What effects does period seem to have on LTC preference? Burstein (Reference Burstein2003) notes that public opinion towards family-based versus state-based care is an important topic to explore among individuals of all ages, due to its potential influence on public policy. According to Burstein, there may have been a recent increase in the preference for formal LTC services that may have encouraged the reinforcement of LTC insurance in Japan. This view is also elicited from trends of recent increases in the actual use of LTC services. However, others have argued that there is a strongly ingrained cultural basis of family responsibility – including support and care for older adults – in East Asia (Chattopadhyay and Marsh, Reference Chattopadhyay and Marsh1999), and thus we can also hypothesise that LTC preferences have not changed easily over time in Japan. One of the few surveys regarding these matters was conducted by the Japanese government (Cabinet Office, Government of Japan, 2002, 2003, 2010) using surveys of the general population at three time-points, 1995, 2003 and 2010, that asked about their preferred place of living if they became bedridden.
However, we cannot evaluate which of the aforementioned hypotheses is valid because the government did not use identical questionnaires across the period. In our survey of existing research on the period effect in the perception of support for older adults, we found one study conducted in the United States of America (USA) and four on East Asian countries. In the USA, Gans and Silverstein (Reference Gans and Silverstein2006) showed that filial norms weakened among people aged 16–91 from the 1980s to the 1990s. In East Asia, Matsunari (Reference Matsunari1991), as well as Ogawa and Retherford (Reference Ogawa and Retherford1993), analysed the same survey data on married Japanese females below the age of 50, and demonstrated that the expectations of old-age support – including financial, physical and emotional care – from children had declined steadily between 1963 and 1986. Similarly, Tsutsui and Muramatsu (Reference Tsutsui and Muramatsu2014) argued that perceived filial obligation had decreased among Japanese family care-givers from 1999 to 2001. In a sample from Taiwan, Hsu et al. (Reference Hsu, Lew-Ting and Wu2001) indicated that agreement on living with married children and their parents among a representative sample of the population has slowly decreased. Unfortunately, there are few studies on the period effect on LTC preferences among older adults in East Asia and Western countries alike.
Even if we could discern the significance of period effects on LTC preference for LTC after controlling the age effect, it is possible that the cohort effect complicates this relationship. Ito (Reference Ito2003) has pointed out that the establishment of LTC insurance reflected a reconfiguration of the welfare state in response to post-industrial changes in Japan, including changing attitudes towards family, work and gender relations – particularly among younger cohorts. Although Hsu et al. (Reference Hsu, Lew-Ting and Wu2001) did not detect a cohort effect in the agreement on living with married children and their parents in Taiwan, younger cohorts of the older adults demographic may express different LTC preferences due to differences in education and labour participation compared to older generations in Japan. In terms of educational attainment, when those aged 65 in 2000 were 15–18 years old, the entrance rate of high school was 40 per cent, and university under 10 per cent. However, when those aged 65 in 2016 were 15–18 years old, the high school entrance rate was about 70 per cent and that of university 20 per cent (Statistics Bureau, Ministry of Internal Affairs and Communications, 2012). While the rate of co-residence with three generations was about 30 per cent among persons aged 65 or above in 2000, this rate had reduced to about 10 per cent by 2016 (Ministry of Health, Labour and Welfare, nd-c). Moreover, the rate of labour participation rate among women aged 30–34 years increased by 10 per cent (from 60%) between 2000 and 2016 (Statistical Bureau, Ministry of Internal Affairs and Communications, nd). Certainly, some empirical studies have indicated that the younger the age, the stronger the preference for institutional LTC among the older demographic (Kim and Kim, Reference Kim and Kim2004; Fernández-Carro, Reference Fernández-Carro2016), suggesting the possibility of a cohort effect. However, these studies have not provided concrete evidence of the cohort effect because it is impossible to separate the effects of age from those of cohort based on cross-sectional data only conducted once. Thus, we need to use repeated cross-sectional data to elucidate the separate age–period–cohort (A-P-C) effects on the LTC preference.
Japan is one of the very few developed countries to have maintained a relatively high rate of co-residence between older parents and their adult children (Takagi et al., Reference Takagi, Silverstein and Crimmins2007). While the rate of co-residence between older adults and their children has decreased from 69 to 39 per cent between 1980 and 2015, it remains higher than rates of such co-residence in Western countries. The traditional form of intergenerational co-residence in Japan can be viewed as a demonstration of filial piety – an ideology requiring children to care for ageing parents (Takagi et al., Reference Takagi, Silverstein and Crimmins2007). As Japan is a country in which filial piety co-exists with a European-style LTC system, analytical results from Japan may prove particularly beneficial regarding the prospective LTC preferences in other welfare states with relatively strong filial piety.
The present study examines the differences in LTC preferences in Japanese older adults according to A-P-C, using six cross-sectional surveys conducted between 1998 – just before the establishment of LTC insurance – and 2016. These surveys were limited to people living in a suburban city of metropolitan Tokyo. This study offers a unique opportunity to assess differences in LTC preferences by A-P-C, resolving the problem of discerning between the effects of these factors by using multiple, identical cross-sectional surveys for representative samples at an 18-year interval in the same geographic location. We hypothesise that the effects of A-P-C on LTC preference differ by gender, family structure and activities of daily living (ADL). According to previous research, the tendency to prefer community LTC services or nursing homes was high in older women as well as in older adults who lived alone (McAuley and Blieszner, Reference McAuley and Blieszner1985; Peek et al., Reference Peek, Coward, Lee and Zsembik1997; Roberto et al., Reference Roberto, Allen and Blieszner2001; McCormick et al., Reference McCormick, Ohata, Uomoto, Young, Graves, Kukull, Teri, Vitaliano, Mortimer, McCurry, Bowen and Larson2002; Eckert et al., Reference Eckert, Morgan and Swamy2004). As these findings suggest that being female and living alone due to a lack of informal support or cultural background is related to greater difficulty in obtaining informal care, it is hypothesised that these characteristics widen the A-P-C effects. Moreover, given that the preference for institutionalisation is higher among older adults with worse health or greater need for care (Min, Reference Min2005; Fernández-Carro, Reference Fernández-Carro2016; Hajek et al., Reference Hajek, Lehnert, Wegener, Riedel-Heller and König2017), it is hypothesised that the A-P-C effects will appear more markedly among this portion of older adults. In addition, in terms of any period effect on preferences for LTC, this study compares and analyses the results between the preferences and actual use of services in the city.
Methods
Sample
The sample used in this study was from a cross-sectional survey repeated six times, 1998–2016, among people aged 65 or older living in a suburban city of metropolitan Tokyo, Japan. The sample size in each survey was: 7,800 (total population of 23,597) in 1998; 10,000 (of 26,905) in 2002; 10,000 in 2004 (of 28,583); 8,000 (of 33,755) in 2010; 3,648 (of 36,821) in 2013; and 3,956 (of 39,707) in 2016. As the surveys between 1998 and 2010 were conducted to collect opinions regarding LTC as well as to screen for older adults living with disability, the initial sample sizes were larger than in surveys after 2010. The sample was selected by a random sampling method using a resident register, and surveys were conducted by mail, with a response rate of 74 per cent in 1998, 77 per cent in 2002, 75 per cent in 2004, 75 per cent in 2010, 67 per cent in 2013 and 68 per cent in 2016. The total number of respondents was 32,140.
The population size of the surveyed city gradually increased from 172,000 in 2000 to 187,000 in 2015. This population shift slightly differed from the demographic trend for the country, which was almost equal in size from 126,900,000 in 2000 to 127,100,000 in 2015. The rate of ageing in the surveyed city increased from 16 per cent in 2000 (national rate of 17 per cent) to 21 per cent (27 per cent) in 2015, suggesting that the speed of population ageing was slower in the surveyed city than that of the country as a whole. In the sample area, taxable annual income was 4.5 million JPY (US$ 41,000) per taxpayer in 2000 and 4.2 million JPY (US$ 38,000) in 2013; this was higher than the national average total of 3.6 million JPY in 2000 and 3.2 million JPY in 2000. Finally, the proportion of adults aged 65 and older living alone was 23 per cent in 2000 and 25 per cent in 2015; these figures were higher than the national averages of 14 and 18 per cent, respectively.
Measurements
LTC preference
The measurement of the preference used in this study was based on a hypothetical condition that required an LTC decision, using the following question: ‘From who or where do you mainly prefer to receive care when you were bedridden?’ This method has been previously used in the studies of Peek et al. (Reference Peek, Coward, Lee and Zsembik1997) and McCormick et al. (Reference McCormick, Ohata, Uomoto, Young, Graves, Kukull, Teri, Vitaliano, Mortimer, McCurry, Bowen and Larson2002). In addition, we constrained the preference to reflect the choice an older adult would need to make if faced with being bedridden. As a result, the measure of LTC preference included seven choices relating to care location (home/community versus institution) and provider (kin versus professional/paraprofessional), specifically ‘spouse’, ‘children including stepchild living with you’, ‘grown children who had lived elsewhere and then moved into your home to provide care’, ‘moving you to your child's’ home’, ‘community LTC services’, ‘nursing homes for older adults’ and ‘hospitals’. We then integrated these choices into the following three categories for an effective analysis: informal care (reference group) including ‘spouse’, ‘children including stepchild living with you’, ‘grown children lived elsewhere and moved into your home to provide care’ and ‘moving you to your child's home’; community LTC services (CLTCS); and institutional LTC services (ILTCS), which included ‘nursing homes for older adults’ and ‘hospitals’. Finally, we created a fourth category to which we added the answers ‘I don't know’ and ‘others’.
Age–period–cohort
The age range of the respondents in this study was 65–107 years. The top-coded age was aggregated as 94, while the bottom-coded age was 65. Age was treated as a continuous variable. Period was determined by the survey years, 1998–2016. Birth cohort was determined by five-year birth cohorts ranging from 1897 to 1951; although the earliest cohort included nine years (1897–1909), while the last included two years (1950–1951).
Gender
Respondent gender was used as a control variable. Male (=1) was treated as the reference group.
Family structure
We measured family structure by living alone (reference group) and living with others.
Activities of daily living
We measured ADL according to whether the respondents went out by themselves; not going out by themselves (=1) was treated as the reference group.
Analysis
First, we examined each A-P-C effect before controlling for the remaining two A-P-C effects other than the focused A-P-C effect and the effects of gender, family structure and ADL. As a result, odds ratios of each rate of CLTCS preference and the ILCTS preference for the rate of informal care preference were calculated by the simple division of each rate of CLTCS preference and ILCTS preference by the rate of informal care preference based upon the LTC preference distributions for each age, period and cohort category.
Second, we examined each A-P-C effect after controlling for the remaining two A-P-C effects other than the focused A-P-C effect and the effects of gender, family structure and ADL. However, A-P-C models suffer from an identifiability problem regarding the relationship between the variables (cohort = period − age). To disentangle the effects of A-P-C, Yang and Land (Reference Yang and Land2013) proposed a hierarchical A-P-C (HAPC) modelling approach utilising individual-level data and a multi-level modelling framework. The period effect is associated with temporal or sequential changes in the conditions and circumstances of life that have an equal impact on all cohorts, while the cohort effect results from differences in living conditions and experiences over time. Thus, it is reasonable to assume that each person in the same period or cohort is embedded in the same socio-historical context as their peers. As a result, in the HAPC, respondents are simultaneously influenced by two higher-level socio-historical contexts defined by the period and cohort, which are randomly modelled (Yang and Land, Reference Yang and Land2013). We adopted an HAPC model and, more specifically, a cross-classified random-effects two-level model (CCREM), which estimated fixed effects for age and age square as level-1 factors, and estimated random effects for period and birth cohorts by treating these variables as level-2 factors. The slope of the regression line with age might result in an ambiguous combination of the age and cohort effects because the scores obtained by centring the grand mean contain both within- and between-cohort variations (Enders and Tofighi, Reference Enders and Tofighi2007). Even when the grand mean is centred, we can still obtain an unbiased regression slope by entering cohort means as a predictor in the level-2 intercept equation (Enders and Tofighi, Reference Enders and Tofighi2007). In terms of the differences in the period and cohort effects according to gender, family structure and ADL, we examined cross-level interactions between gender, family structure and ADL as level 1 and each period and cohort as level 2. Regarding the differences in the age effect by gender, family structure and ADL, we examined interactions between age and gender, family structure and ADL as level 1.
Ethical considerations
This study was conducted according to the guidelines set by the Helsinki Declaration, and the Research Ethics Board of Tokyo Metropolitan University approved all procedures (authorisation number H28-66). Both a letter of invitation explaining the content of the study and the questionnaire were sent to each potential participant in the surveys. Data collection procedures assured confidentiality by the use of self-administered and anonymous questionnaires. Identification numbers were given to questionnaires used in the surveys between 1998 and 2010 because these surveys were conducted to screen older adults living with disability. The questionnaires for opinion surveys conducted between 1998 and 2010 were separated from those used for screening to further assure anonymity in the former. As a result, the questionnaires used in the opinion surveys were anonymous. Participation in this study was completely voluntary and confidentiality was fully guaranteed. Only respondents who wished to participate in this survey returned their questionnaires.
Results
Actual use of LTC services in the surveyed city
Figure 1 shows the actual use of each CLTCS, ILTCS and community support projects service (CSPS; starting from 2006) in the surveyed city and the entire country of Japan. The benefits for the long-term care services in Japan are classified using seven-grade nursing care levels including the two that are least severe (support levels 1 or 2) and the five that are more severe (care levels 1–5) according to the individual's degree of needed help. CSPS are provided to meet the goal of ‘maintaining or enhancing the ability to perform daily activities and preventing people from becoming dependent’, and eligible people for these services are the individuals with support levels 1 or 2 (Tsutsui and Muramatsu, Reference Tsutsui and Muramatsu2007). The data in Figure 1 were obtained from the Report on Long-term Care Insurance Service (Ministry of Health, Labour and Welfare, nd-a). The rate of CLTCS users among the insured in the city showed a rapid increase from 2001 to 2004. Although this indicated a slight reduction in use in 2006 and 2007 just after the launch of CSPS, CLTCS showed a gradual increase in use after 2008. The number of ILTCS users among the insured in the city appeared to be nearly stable over the period. These trends were quite similar to the rates in Japan as a whole. Although the rates of LTC service differed by age and gender, our figure does not show results that controlled for the influences of age and gender differences over time because the available data did not include numbers that were broken down by age and gender categories.
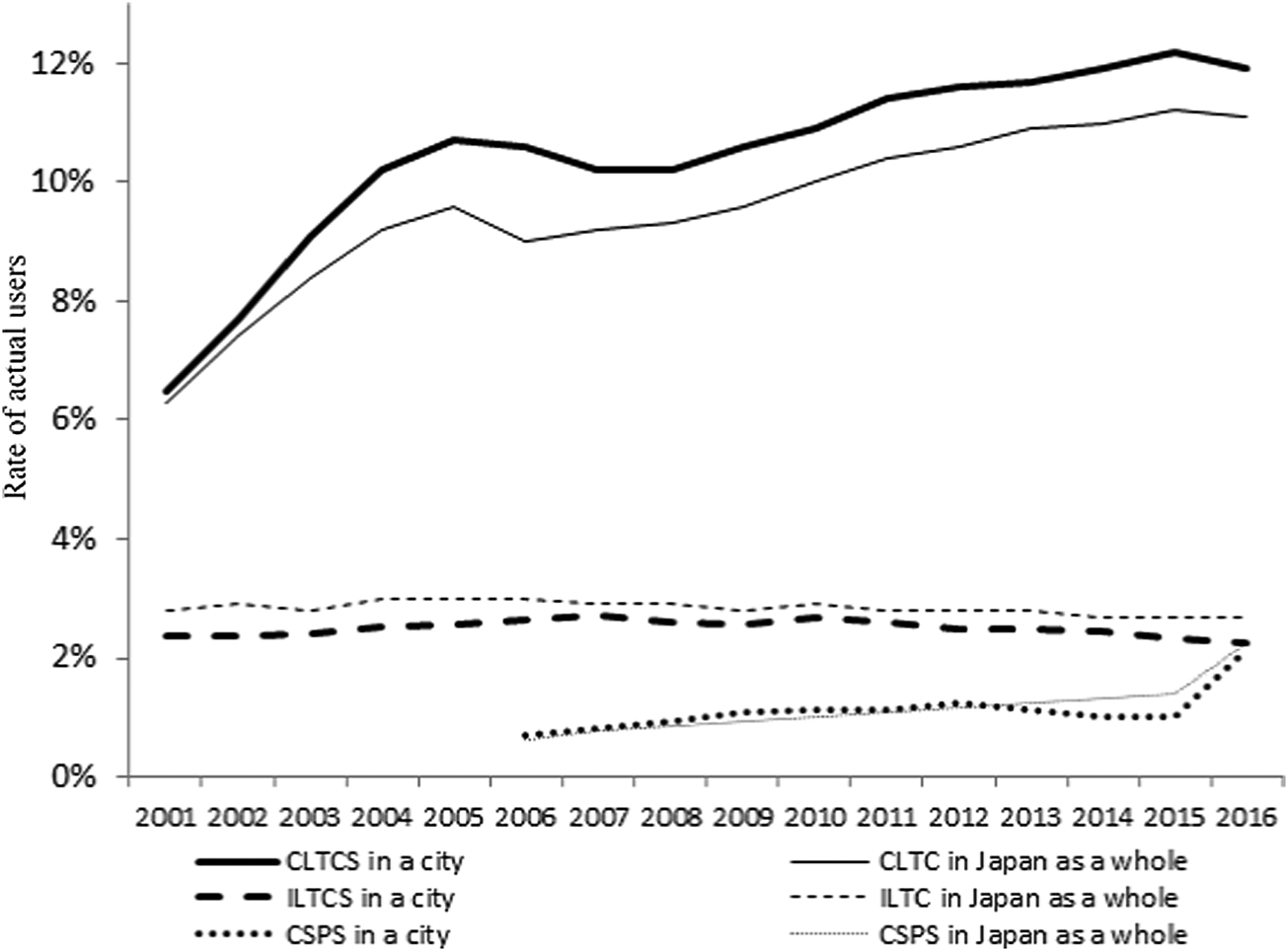
Figure 1. Rate of the actual use of community long-term care services (CLTCS), institutional long-term care services (ILTCS) and community support projects services (CSPS) in insured individuals aged 65 and over in a city in metropolitan Tokyo and Japan as a whole.
With regards to the rates of all types of LTC service users in Japan, there were data which presented the number of users that were broken down by age and gender categories in the Survey on Long-term Care Insurance Payments (Ministry of Health, Labour and Welfare, nd-d). As shown in Figure 2, we calculated the age- and gender-adjusted rates of LTC service users in older adults from 2001 to 2016 using the 2000 census data as the reference population. As the calculation method for the rate of users in Figure 2 differed from that used in Figure 1, the rates of LTC service users differ from total ratios of CLTCS, ILTCS and CSPS users. Even after controlling for the age and gender differences over time, the rate of LTC service users showed a gradual increase over time. If the number of ILTCS users remains stable over time, there is a high probability that the incremental gains in the number of LTC service users reflect increasing trends towards CLTCS use. This increase in use is not only observed in the surveyed city but also in Japan, suggesting that the gradual increase could not be explained by age and gender differences in population over time.

Figure 2. Rate of the actual long-term care (LTC) users among Japan's total population aged 65 and over. Note: LTC users included CLTCS, ILTCS, and CSPS users.
Characteristics of respondents
Table 1 provides a summary of statistics for LTC preference, age, period, cohort, gender, family structure and ADL based on the surveys conducted between 1998 and 2016. A total of 605 respondents were third persons other than the target persons who were eligible to answer the questionnaires, while 963 respondents had at least one missing value without an LTC service preference. These respondents were excluded from the analysis. Consequently, the final sample size was 30,882. The respondents excluded from the analyses were less likely to prefer informal care and were more likely to be female. The number of respondents who preferred informal care (35%) and ILTCS (33%) was almost the same. The number of respondents who preferred CLTCS was 23 per cent.
Table 1. Characteristics of respondents for analyses
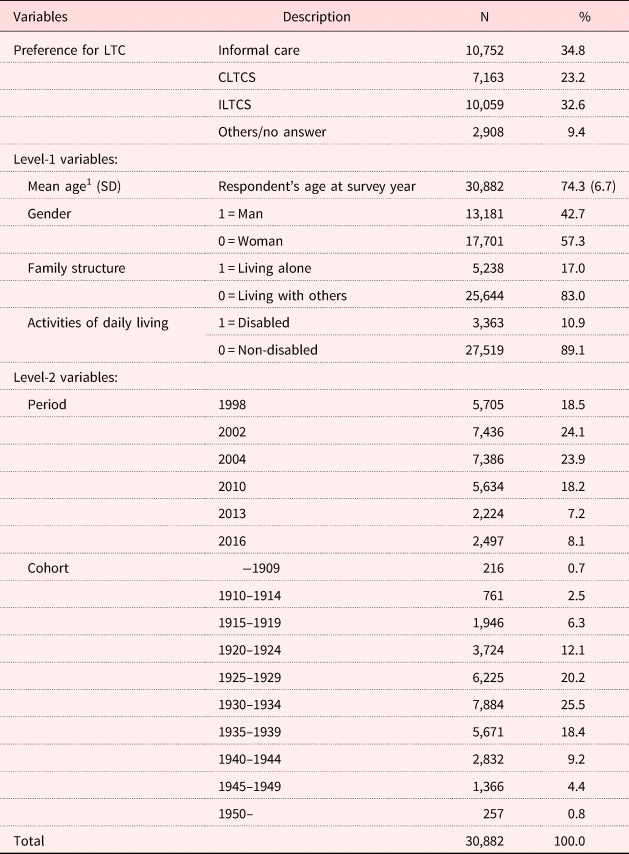
Notes: LTC: long-term care. CLTCS: community long-term care services. ILTCS: institutional long-term care services. SD: standard deviation. 1. Mean values before centring.
Age, period and cohort effects on LTC preference
Table 2 shows the A-P-C effects on LTC preference before controlling other factors. The accumulated distribution of each preference of informal care, CLTCS, ILTSC and others/no answers from 1998 to 2016 surveys was 34.8, 23.2, 32.6 and 9.4 per cent, respectively. In terms of the period effect, although the odds ratios of CLTCS preference and ILTCS preference compared to informal care preference were almost the same between 1998 and 2004, they increased in 2010. The effect of period on each odds ratio was significant with the odds ratio of CLTCS preference to informal care preference: p < 0.001; and the odds ratio of ILTCS preference to informal care preference: p < 0.001. As for the age effect, each odds ratio for the preference CLTCS and ILTCS to that for informal care decreased according to the increase in age. The effect of age on each odds ratio was also significant with the odds ratio for CLTCS preference to informal care preference being p < 0.001, and the odds ratio for ILTCS preference to informal care preference being p < 0.001.
Table 2. Differences in preference of long-term care by age, period and cohort, and odds ratio (OR) of each preference rate of community long-term care services (CLTCS) and institutional long-term care services (ILTCS) to that of informal care
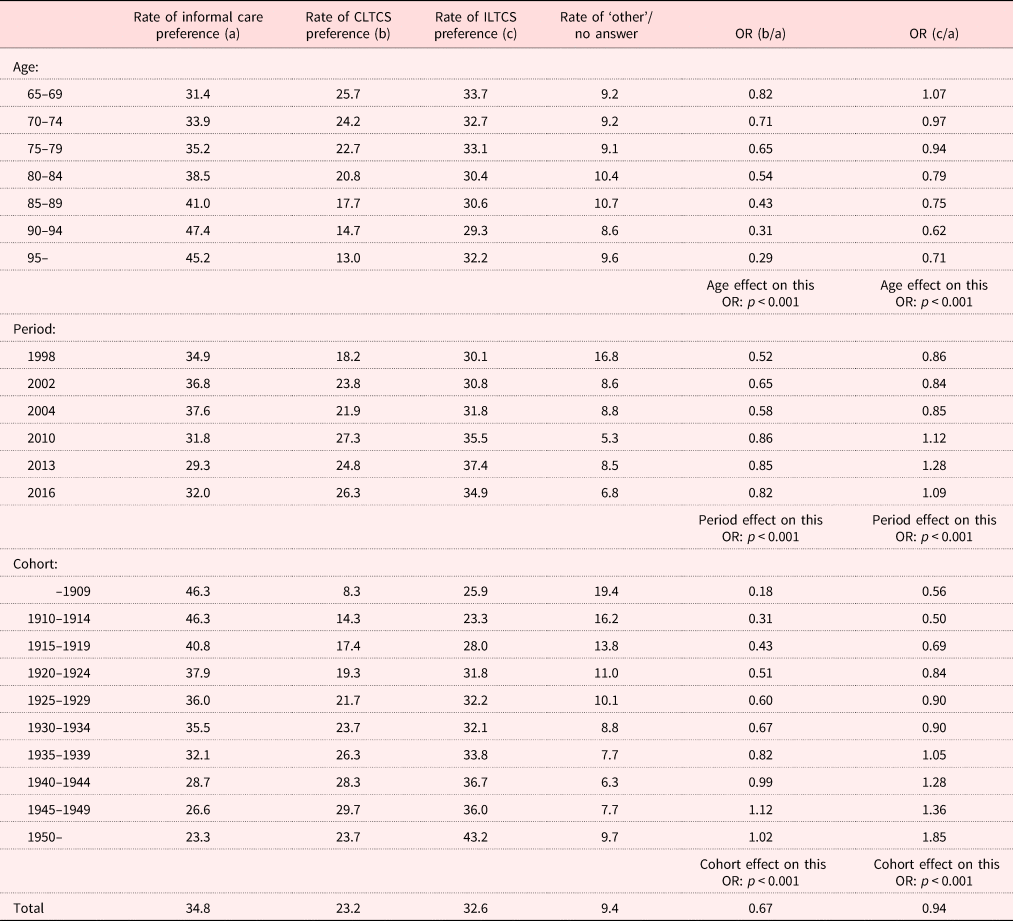
Notes: ORs for each preference of CLTCS and ILCTS compared to the preference for informal care were calculated by simple division of each rate of CLTCS preference (b) and ILTCS preference (c) by rate of informal care preference (a). As a result, each OR did not control for the remaining two effects other than the focused age, period and cohort effect, and the effects of gender, family structure and activities of daily living.
With regard to the cohort effect, each odds ratio for the preference CLTCS and ILTCS to that for informal care increased the younger the cohort was. That is, the younger the cohort, the more likely the preference for CLTCS and ILTCS. Effect of cohort on each odds ratio was significant with the odds ratio for CLTCS preference to informal care preference being p < 0.001, and the odds ratio of ILTCS preference to informal care preference being p < 0.001.
Table 3 provides the results by CCREM to examine each A-P-C effect on LTC preference separately. Each A-P-C effect was examined after controlling for the remaining two effects other than the focused A-P-C effect and effects of gender, family structure and ADL. The odds ratio for the preference of CLTCS to that for informal care largely differed by period (p < 0.10). To interpret this result, we calculated predictive values using the regression equation, as illustrated in Figure 3. The preference for CLTCS increased after 1998, in contrast with the preference for informal care, and the level of this preference was almost the same after 2010, although the actual number of CLTCS users showed a gradual increase during the same period, as indicated in Figure 2.

Figure 3. Period effects on preference for community long-term care services (CLTCS).
Table 3. Estimated hierarchical age–period–cohort models of preference for long-term care, 1998–20161

Notes: CLTCS: community long-term care services. ILTCS: institutional long-term care services. 1. The cross-classified random-effects model was conducted using all variables in the model shown in Table 1. However, this table shows only related results. 2. The results for the cross-classified random-effect model indicated that the G-matrix was not positive. As a result, we excluded these variables from the random-effect model.
In terms of age effects, older respondents had a significantly lower preference for both CLTCS and ILTCS compared to informal care (CLTCS: p < 0.001; ILTCS: p = 0.002). Moreover, the interactions between age, gender and family structure were significant, with the interaction between age and gender on CLTCS being highly significant (p < 0.001), as well as the interaction between age and gender on ILTCS (p < 0.001), and the interaction between age and family structure on ILTCS (p = 0.005). To interpret these results, we calculated predictive values using the regression equation, the results of which are illustrated in Figures 4 and 5. Each difference in the odds ratio of the preferences for both CLTCS and ILTCS by gender reduced according to the increase in age (Figure 4). Furthermore, the difference in the odds ratio of the preference for ILTCS by family structure decreased relative to the increase in age (Figure 5). Although we observed the cohort effect of the preference before controlling age, period and other independent factors, we did not observe a significant cohort effect after controlling these factors.

Figure 4. Gender differences in age effect on preference for both community long-term care services (CLTCS) and institutional long-term care services (ILTCS): (a) CLTCS versus informal care; (b) ILTCS versus informal care.

Figure 5. Family structure differences in age effect on preference for institutional long-term care services (ILTCS).
Discussion
The results of the present study provide new evidence about the A-P-C for LTC use among older Japanese adults. Aggregate data obtained from 1999 to 2016 showed that each preference for informal care, CLTCS, ILTCS and other/no answer occupied 35, 23, 33 and 9 per cent, respectively. A significant period effect was observed, with the preference for CLTCS as compared to informal care increasing between 1998 and 2010, and remaining nearly stable after 2010. A significant age effect was also observed. Both preferences for CLTCS and ILTCS over informal care were higher among younger participants. Moreover, the age influence was stronger in women and respondents who lived alone. We did not observe a significant cohort effect for preference.
As the area in which respondents in this study lived was limited, we need to be careful in generalising from these results. We can compare these data to the surveys on LTC preference in a national representative sample conducted in 2003 and 2010 by the Japanese government (Cabinet Office, Government of Japan, 2003, 2010); however, when doing so, we must pay attention to the differences between the surveys regarding the preference categories used. The surveys conducted by the Japanese Cabinet Office used an integrated category of ‘at home’ to represent the categories of informal care and CLTCS that were used in this study, and the additional choice of ‘fee-based nursing homes’ was added to the Japanese Cabinet Office survey. According to the Cabinet Office surveys: 45 per cent of respondents aged 65 or over selected ‘at home’ in 2003, while 42 per cent chose this option in 2010; 33 per cent selected ‘nursing homes’ or ‘hospitals in 2003 and 39 per cent in 2010; while 9 per cent chose ‘fee-based nursing homes’ in 2003 and 12 per cent in 2010. In this study, the rate of respondents who selected ‘at home’ – which included both informal care and CLTCS – was 58 per cent, while 33 per cent preferred ILTCS, which included nursing homes and hospitals. The higher preference for ‘at home’ in this study may be due to not including the choice of ‘fee-based nursing homes’. Nonetheless, as the distributions of the preference for community and institutions are similar in both surveys, we can generalise the results of the present study to a certain degree.
It is difficult to explore how the preferences among Japanese older adults differ from those in the same demographic in other countries, as there are no studies which have used the same measurements. While comparability is somewhat problematic, we can examine the characteristics the preferences of our study's respondents in comparison ones of people from other counties. According to Esping-Andersen (Reference Esping-Andersen1990), there are three ideal regime types in the welfare states, liberal, conservative and social-democratic, and these provide important insights when comparing such data. In the liberal regime, the state provision of welfare is minimal, benefits are modest and often attract strict entitlement criteria, and recipients are usually means-tested and stigmatised. The conservative welfare state regime is distinguished by its ‘status-differentiating’ welfare programmes in which benefits are often earnings-related, administered through the employer and geared towards maintaining existing social patterns. The social-democratic regime is the smallest regime cluster; welfare provision is characterised by universal and comparatively generous benefits, a commitment to full employment and income protection, and a strongly interventionist state is used to promote equality through a redistributive social security system. Norway (Daatland, Reference Daatland1990) and the Netherlands (Wielink et al., Reference Wielink, Huijsman and McDonnell1997; Wielink and Huijsman, Reference Wielink and Huijsman1999) are typed as the social-democratic regime (Esping-Andersen, Reference Esping-Andersen1990), and the rate of the preference for informal care was much lower than for CLTCS. Germany (Pinquart and Sörensen, Reference Pinquart and Sörensen2002) is typed as a conservative regime (Esping-Andersen, Reference Esping-Andersen1990), and the preference for informal care was almost equal to that for CLTCS. Esping-Andersen (Reference Esping-Andersen1997) labelled Japan as a hybrid of a liberal regime and a conservative one. According to a review article of quantitative studies on welfare typologies in developed countries based on the framework by Esping-Andersen, Japan does not seem to fit clearly any of the identified typologies (Ferragina and Seeleib-Kaiser, Reference Ferragina and Seeleib-Kaiser2011). As a result, we followed a label by Esping-Andersen, identifying Japan as a hybrid of a liberal regime and a conservative one.
The preference for informal care and CLTCS in this study was 35 and 23 per cent, respectively. These results are more similar to those of Germany, a conservative regime, than those of countries included in the social-democratic regime. As for the distribution of the preference for institution as place of receiving care, Spain (Costa-Font et al., Reference Costa-Font, Elvira and Miró2009; Fernández-Carro, Reference Fernández-Carro2016), Taiwan (Wang et al., Reference Wang, Chung, Lai, Chou and Kao2004; Chung et al., Reference Chung, Hsu, Wang, Lin, Huang, Amidon and Kao2008) and Korea (Kim and Kim, Reference Kim and Kim2004) are typed as conservative regimes (Daatland and Lowenstein, Reference Daatland and Lowenstein2005; Lee and Ku, Reference Lee and Ku2007), and approximately 20 per cent or less of respondents preferred nursing homes in these countries. The USA (McAuley and Blieszner, Reference McAuley and Blieszner1985; Peek et al., Reference Peek, Coward, Lee and Zsembik1997; McCormick et al., Reference McCormick, Ohata, Uomoto, Young, Graves, Kukull, Teri, Vitaliano, Mortimer, McCurry, Bowen and Larson2002) is categorised as a liberal regime (Esping-Andersen, Reference Esping-Andersen1990), and 25–40 per cent of respondents preferred nursing homes. In this study, 33 per cent of respondents preferred ILTCS. It is possible that the preference for ILTCS in Japan is relatively similar to that in the USA, more so than in Spain and other countries in East Asia.
With regard to the period effect, there have been few studies on the preference LTC of older age in Western countries. In East Asia, as noted earlier, only two studies have indicated that the expectations and norms of old-age support from children have declined steadily over time (Matsunari, Reference Matsunari1991; Ogawa and Retherford, Reference Ogawa and Retherford1993). However, both the studies by Matsunari (Reference Matsunari1991) and Ogawa and Retherford (Reference Ogawa and Retherford1993) were published more than 20 years ago and are limited in that they did not control the cohort effects. This study observed the approximate increase in the preference for CLTCS between 1998 and 2010. However, it remains unclear whether this period effect resulted from the reinforcement of LTC insurance or a historical trend in the decreasing preference for informal ITC care because the preference for LTC was measured only once before the fortification of LTC insurance.
Interestingly, the preference for CLTCS occurred around the same time, after 2010, although the actual use of CLTCS increased during this period, as noted earlier. Why did the preference for CLTCS not strengthen after 2010? There are two possible reasons. One reason for this relates to the resilience of filial piety. Croll (Reference Croll2006) has suggested that filial piety has been resilient against modernisation in Asia because intergenerational exchanges of monetary and other forms of aid have adapted to become a component of filial piety. Hirosima (Reference Hirosima1987), as well as Elliott and Campbell (Reference Elliott and Campbell1993), noted that co-residence in Japan was moving away from an obligatory behaviour urged by ideology and becoming a strategic behaviour based upon choice and a give-and-take relationship. Tsuya and Martin (Reference Tsuya and Martin1992) have also pointed out that attitudes towards inheritance are more pragmatic or compensatory because it would be preferable to leave property to the children who took care of the older adults. Another may be related to the recognition of the availability of CLTCS among older adults. Although LTC insurance was ideally established to realise socialisation of LTC, the effects of CLTCS insurance on the overall wellbeing of older people living with disability and their informal carers remain unclear (Tamiya et al., Reference Tamiya, Noguchi, Nishi, Reich, Ikegami, Hashimoto, Shibuya, Kawachi and Campbell2011). As a result, the lack of effectiveness of CLTCS may also be an explanatory factor in the levelling-off of CLTCS preference after 2010.
In terms of older adult preferences for ILTCS, this study did not provide evidence of a significant decrease in preference after the reinforcement of LTC insurance. In addition, although the preference rate for CLTCS increased, it remains lower than the preference rate for ILTCS. In fact, the preference rate for CLTCS and ILTCS was 26.3 and 34.9 per cent, respectively, in 2016. Why is the preference for ILTCS higher than that of CLTCS in older adults? Putting older adults in ILTCS would alleviate most of the care-giving burden of family care-givers since that is seen as transferring total responsibility (Tamiya et al., Reference Tamiya, Noguchi, Nishi, Reich, Ikegami, Hashimoto, Shibuya, Kawachi and Campbell2011). The usage of ILTCS among older adults could largely reduce the concern and challenges for their family members compared to the use of CLTCS, which may be related to the continued preference of ILTCS to CLTCS among older adults, even after the launch of LTC insurance.
Regarding the actual service use in the surveyed city, the user rate of ILTCS was 11.9 per cent, and it was five times the rate of CLTCS (2.3%; Ministry of Health, Labour and Welfare, nd-c). It seems that the preference of ILTCS to CLTCS in older adults might not be a reflection of the actual use of both ILTCS and CLTCS. Gaps between preference and actual use of ILTCS may appear through policies to restrict ILTCS use which pre-date the launch of LTC insurance. Before LTC insurance, LTC services including CLTCS and ILTCS were provided by local government or by special welfare organisations. As access to both CLTCS and ILTCS remain limited by the budget while the health-care costs were not subject to budgetary restraints, the demand for ILTCS came to be met by hospitals (Ikegami et al., Reference Ikegami, Yamauch and Yamada2003). As a result, medically inappropriate and expensive ‘social admissions’ to hospitals were seen as a serious problem. To resolve these problems, an inclusive per diem payment was introduced to hospitals that focused on LTC in 1990 (Ikegami et al., Reference Ikegami, Yamauch and Yamada2003).
Also, the reform of the medical insurance system in 2006 led to the discontinuance of LTC hospitals. After the establishment of LTC insurance, the goal was to reduce the economic incentive for institutionalisation by requiring ILTCS users to pay room and board expenses. The co-payment for food, living quarters, around-the-clock care and safety was lower than the rent and utilities for most apartments in Japan (Tsutsui and Muramatsu, Reference Tsutsui and Muramatsu2007). In addition, the Japanese government intended that improving CLTCS through LTC insurance would reduce the dependence and expenditure on ILTCS (Campbell et al., Reference Campbell, Ikegami and Gibson2010). Even after the launch of LTC insurance, informal care-givers including family members comprised approximately 70 per cent of the primary care-givers of older adults living with disability, suggesting that CLTCS seems to serve only a subsidiary role (Ministry of Health, Labour and Welfare, 2017b). In fact, government policy aims to supplement informal care and relieve some of the burdens on family members (Campbell et al., Reference Campbell, Ikegami and Gibson2010).
On the other hand, after the launch of LTC insurance, the number of applicants for nursing homes increased. This demand may be the result of the reduction of stigmatisation in nursing homes and the relaxing of the qualifications to apply for residence in a nursing home. According to a survey conducted in 2009 and again in 2014, by the Ministry of Health, Labour and Welfare, the number of applicants for nursing homes increased (Division of the Support for the Elderly, General Affairs Division, Ministry of Health, Labour and Welfare, 2014). It is possible that a gradual increase in the actual use of CLTCS may be better for those older adults who are not able to use ILTCS.
In terms of the age effect on LTC preference, we observed that the younger the respondent, the more likely the preference for CLTCS and ILTCS during the observational periods – even after controlling the influence of other variables. In addition, age effects were stronger in women than in men, as well as for respondents who lived alone than those who lived with others. Some empirical studies have indicated that younger respondents had a stronger preference for ILTCS; findings based on cross-sectional data, with uncontrolled cohort effects (Kim and Kim, Reference Kim and Kim2004; Fernández-Carro, Reference Fernández-Carro2016). Moreover, according to a survey conducted by the Ministry of Health, Labour and Welfare (nd-a), 64 per cent of adults aged 50–59, and 49 per cent of adults aged over 70 reported preferring to receive care outside their own homes. This study found that ageing influenced a lower preference for ILTCS similar to the results of previous studies (Kim and Kim, Reference Kim and Kim2004; Cabinet Office, Government of Japan, 2010; Fernández-Carro, Reference Fernández-Carro2016). Based on the Survey of Institutions and Establishments for Long-term Care (Social Statistics Office, Director-General for Statistics and Information Policy, Ministry of Health, Labour and Welfare, 2016), the Survey of Long-term Care Benefit Expenditures (Social Statistics Office, Director-General for Statistics and Information Policy, Ministry of Health, Labour and Welfare, nd) and the Comprehensive Survey of Living Conditions (Ministry of Health, Labour and Welfare, 2017a), rates of actual LTC services use increased according to being in the older age category. That is, this study suggests that gaps between the preference for LTC and actual use of LTC services widen as persons become older.
With regard to the reasons why younger people have a stronger inclination to use ILTCS, Kim and Kim (Reference Kim and Kim2004) explained that younger generations are better informed about ILTCS and thus have a more positive attitude towards such care. Fernández-Carro (Reference Fernández-Carro2016) noted that the willingness to choose ILTCS as an ideal setting increased with the level of education among the younger cohorts of older people. While their rationalisation is related to cohort differences in LTC preference, our study did not observe significant cohort effect on the preference; we also observed an age effect on the preference even after controlling the cohort effects. The theory of socio-emotional selectivity elucidates our finding. As is typical with age, people become increasingly selective and invest greater resources in emotionally meaningful goals and activities than in knowledge-related goals (Carstensen et al., Reference Carstensen, Isaacowitz and Charles1999). This selective narrowing of social interaction maximises positive emotional experiences and minimises emotional risks as individuals become older. Based on this theory, we suggest that those of an older age would like to receive care from informal care-givers in order to maximise positive emotional experiences. In addition, in this study, older age was related to narrowing the difference between the preference for CLTCS and ILTCS among both family structure and gender. A stronger motivation to seek positive emotions linked to ageing may contribute to an increased preference for informal care in females as well as among older adults who live alone.
Concerning the cohort effect, respondents from earlier cohorts grew up in a period characterised by strong national goals and values. The strong social values and system of this period were influenced by Confucian norms and traditional family ideology (Izuhara, Reference Izuhara2000). In contrast, respondents in later cohorts were raised in a rapidly democratising society during the post-Second World War period, in which a new family ideology emerged (Izuhara, Reference Izuhara2000). Accordingly, we hypothesised that respondents in earlier cohorts had a stronger preference for informal care than those of later cohorts due to the significant discrepancy in life experiences between the cohorts. After controlling the age effect, we did not obtain results supporting this hypothesis. As noted when considering the period effects on the preference for CLTCS, if economic incentives exist as a background of filial piety, it is possible that the cohort effect of the preference for CLTCS and ILTCS weakened.
This study not only identified gaps by period and age between the preference for LTC and tendencies in the actual use of LTC services, but also the explanatory factors of these gaps. Is it possible that other factors contribute to these gaps? One study reported that the choice of services for older adults was not only influenced by the wishes of their family members, but at times, the decision was made by the families (Asahara et al., Reference Asahara, Momose and Murashima2003). Accordingly, it is possible that trends of the actual use LTC services mainly reflect decreases in intentions or norms of providing informal care to older parents among the general population, especially middle-aged people who do not wish to act as informal care-givers. Certainly, Tsutsui and Muramatsu (Reference Tsutsui and Muramatsu2014) presented the findings which supported this view: perceived filial obligation had decreased among Japanese family care-givers, especially among daughters-in-law from 1999 to 2001, although the study by Tsutsui and Muramatsu (Reference Tsutsui and Muramatsu2014) was limited by the low frequency of surveys and the short time period. While one of the characteristics of ITC insurance in Japan is its user-oriented system, where users can choose their care services directly from many providers (Tsutsui, Reference Tsutsui2010), this study indicates that this idea has not come fully to fruition. To verify if the actual LTC service use parallels the intentions and norms of providing informal care to their older parents among middle-aged people, we need to examine the A-P-C effects on their intentions and norms as a future study.
This study has some limitations, the first of which is related to choices provided on the questionnaire to measure LTC preference. The preference for LTC options – such as fee-based nursing homes for older adults – has been diversified with new LTC trends (Cabinet Office, Government of Japan, 2010). While this study did not add such choices due to securing the comparability across surveys, these choices indicating new trends need to be included in future research. The second limitation is that the periods for the cross-sectional survey were relatively short. By using analytical data covering longer periods of time than in this study, we can examine the cohort effect on LTC preference in detail. The third limitation is related to our study population, although the rate for each actual use of CLTCS and ILTCS and these time trends were very similar both in the surveyed city and in Japan as a whole. The surveys used in this study were conducted in a geographically restricted area, and results may not be generalisable to other areas because local conditions may influence LTC preferences. Peek et al. (Reference Peek, Coward, Lee and Zsembik1997) have shown that rural older adults were nearly twice as likely as urban older adults to report that they would turn to family members rather than nursing homes if their failing health resulted in them no longer being able to live independently. Similarly, Coward et al. (Reference Coward, Cutler and Mullens1990) reported that severely impaired older adults residing in non-metropolitan communities were significantly more likely to be receiving assistance exclusively from informal helpers than older residents living in more urban and suburban community settings.
Conclusions
This study has overcome some of the shortcomings of prior studies that have investigated the influences of each A-P-C on the preference for LTC. Previous studies that have been conducted only focused on periodic trends or age effects in the preference for LTC, and therefore ignored cohort effects. In addition, this study examined the differences in the influences of each A-P-C on the preference for LTC by gender, family structure and ADL. Regarding the period effect, while there was an increase in levels of preference for CLTC, as compared with those of informal care from 1998 to 2010, levels of these preferences were almost stable after 2010. In terms of the age effect, the younger the respondent, the more likely the preference for CLTCS and ILTCS as compared with informal care. Moreover, the age influence was stronger in women and among respondents who lived alone. This study suggests that there are gaps by period and age between the preference for LTC and the actual LTC services use. Also, it is suggested that possible related factors or backgrounds for these gaps, including pragmatic filial piety, socio-emotional selectivity, and norms and intention of providing care in middle-aged adult children, should be included in future research.
Author ORCIDs
Hidehiro Sugisawa http://orcid.org/0000-0003-1646-1824.
Author contributions
HS formulated the research questions, designed the study, analysed the data and wrote the article. YS and YN designed a portion of the study and conducted data analysis on the preference for long-term care. All authors contributed to drafting the manuscript, and read and approved the final version of the manuscript.
Financial support
This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (grant number 25285175).
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The study complied with the guidelines of the Helsinki Declaration. All procedures were approved by the Research Ethics Board at the Tokyo Metropolitan University (authorisation number H28-66).










