Introduction
Population ageing has created an unprecedented global challenge to the social welfare arrangement in many countries as the number of older people is expected to grow from an estimated 524 million in 2010 to nearly 1.5 billion by 2050 globally, compounded by a growing dependency ratio due to declining fertility rates and increased longevity of the older populations (World Health Organization, 2018). The fast ageing population is associated with a sharp rise in the prevalence of old-age conditions requiring both health and long-term care (LTC) services. Despite more LTC services being provided formally in many countries these days, informal care, often provided by family members and unpaid care-givers, remains an important source of LTC for older people. In Europe, it is estimated that between 20 and 44 per cent of the LTC is provided by informal carers (Jegermalm and Grassman, Reference Jegermalm and Grassman2011; Jang et al., Reference Jang, Avendano and Kawachi2012; Sole-Auro and Crimmins, Reference Sole-Auro and Crimmins2014; Verbakel, Reference Verbakel2017). The same phenomenon is observed in other ageing societies, such as Japan, South Korea and Singapore (Jang et al., Reference Jang, Avendano and Kawachi2012; Hayashi, Reference Hayashi2016). In Japan, informal care accounts for approximately 24–41 per cent of the care, where traditional social norms tend to put the primary responsibility for care on children (Hanaoka and Norton, Reference Hanaoka and Norton2008).
Despite the fact that informal care plays an essential role in the LTC system in developed countries, the majority of these countries have policies in place for formal LTC provision. The development of LTC is different in developing countries, including emerging economies in the world, whereby the formal LTC system is often fragmented, less established or non-existent, and the demographic shift towards an ageing population is rapid. It is projected that, by 2050, nearly eight in ten of the world's older people will live in less-developed regions (World Health Organization, 2018). This is especially pertinent for a region such as Asia, which comprises some of the largest developing countries in the world and LTC provision is predominately reliant on informal care-givers.
China, for example, is experiencing population ageing at an unprecedented pace. Although nearly 180 million people or 13.3 per cent of the population (National Bureau of Statistics of China, 2011) are above 60 years old, China's formal LTC system is still in its infancy. Informal care, long enshrined by the Confucian ethics of filial piety, is still the mainstay of old age support in China (Fu et al., Reference Fu, Guo, Bai and Chui2017). It is predicted that a quarter of older people aged 60 and above in China were receiving informal care from a family member, and the number of informal carers was estimated to be 53 million people in 2014 (Hu and Ma, Reference Hu and Ma2018). However, rapid demographic shifts and socio-economic changes have fuelled considerable concerns over the LTC system in China. The one-child policy introduced since 1979 has direct implications for LTC arrangements as the Chinese society has experienced a significant increase in dependency ratios resulting from the enforcement of this policy (Lou and Ci, Reference Lou and Ci2014). With the mass flow of labour from countryside to city, older people in rural areas are now geographically distant from their children and grandchildren, and this family-centred approach has become untenable.
Population ageing is also fuelling concerns about an inadequate supply of informal care for older people (Feng et al., Reference Feng, Liu, Guan and Mor2012). Chen (Reference Chen2015) conducted a series of studies on factors influencing older people's choices of LTC services. She found that many older people worried about the issue of discordance and may feel distrust towards their children whose practices may not conform to their perception of filial piety. Some of them were also worried that the disruption from care-giving arrangements could affect the dynamics of co-residence with their children (Chen, Reference Chen2015). The child care-givers, on the other hand, also complained that they were unable to balance work and care responsibilities, and they responded by seeking paid help or by placing their parents in a nursing home for professional care (Chen and Ye, Reference Chen and Ye2013). These circumstances have shifted informal care-giving norms, and affected both care recipients’ willingness and family members’ commitment towards informal care provision.
As instrumental support from family care-givers is declining, unmet needs, which have been widely documented as leading to numerous adverse effects on health, are on the rise (Zhen et al., Reference Zhen, Feng and Gu2013). Gu and Vlosky (Reference Gu, Vlosky, Garner and Christiansen2008) found that nearly 60 per cent of older Chinese people reported having unmet needs in 2005. Predisposition and enabling factors, such as socio-economic status, place of residence and access to health services, are strongly associated with unmet needs. Zhu (Reference Zhu2015) found that older people living in rural areas and having an activities of daily living (ADL) limitation are more likely to have unmet needs. Another study, by Zhu and Österle (Reference Zhu and Österle2017), showed that rural residents and those with limited education have a significantly higher risk of unmet needs. These findings are bolstered by a more recent study in China which reported that older people living in rural areas have higher levels of unmet needs compared to those living in urban areas, and higher levels of unmet needs is associated with more severe depressive symptoms (Hu and Wang, Reference Hu and Wang2019). Despite using different data sources, these studies, nevertheless, reached similar conclusions, that is, a significant mismatch exists in terms of LTC needs and the availability of care among older people in China.
Previous studies have contributed to a preliminary understanding of unmet needs and overall LTC provision in China, but the relationship between informal care provision, the most important and frequently used care for older people in China, and unmet needs, is under-examined. In particular, questions such as how much informal care an older person receives on average and whether the intensity of informal care-giving has any effects on unmet needs, remains unanswered. Answers to these questions are particularly important for Chinese policy makers as we often assume that informal care is still preferred by Chinese families without having a clear picture of whether and how much informal care is being utilised by older people nowadays. Furthermore, even among those who receive informal care, a significant discrepancy exists in terms of intensity of care. Whether and to what extent this discrepancy may associate with different care outcomes remains an empirical puzzle. Drawing data from the 2015 wave of the China Health and Retirement Longitudinal Survey (CHARLS), this study seeks to explore the relationship between informal care provision and unmet needs. We ask the following research questions:
(1) On average, how much informal care does a disabled older person receive per month?
(2) Does receiving informal care lower unmet needs as opposed to not receiving informal care?
(3) Among those who receive informal care, does a higher intensity of informal care associate with lower unmet needs?
We define disabled people as having one or more ADL or instrumental ADL (IADL) limitations, and we pay special attention to older people with physical limitations, which is one of the key factors that drives unmet needs (Liu et al., Reference Liu, Chang and Huang2012; Herr et al., Reference Herr, Arvieu, Aegerter, Robine and Ankri2014).
The rest of the paper is organised as follows. The next section illustrates the data, sample and methods applied in the analysis. The third section describes the empirical results. The final section concludes and discusses policy implications and suggests future directions in building a sustainable LTC provision system in China.
Data and methods
Data and sample
This study draws data from the 2015 wave of the CHARLS (Zhao et al., Reference Zhao, Hu, Smith, Strauss and Yang2014), which employs multi-stage sampling to collect a nationally representative sample of Chinese residents aged 45 and above in 28 provinces/autonomous regions. The survey asks questions relating to respondents’ demographic and socio-economic statuses, health and health services utilisation, and LTC needs and utilisation. In our analysis, we also merged data from the CHARLS with regional economic data (provincial Gross Domestic Product (GDP) per capita) from the Global Economic Data, Indicators, Charts & Forecasts (CEIC) China Premium Database 2015.
Our study sample encompasses older people who reported difficulties in managing either ADLs or IADLs (disabled older people hereafter) and received informal care. The reason for using this sample is because the information used for constructing the dependent variable in our analysis (i.e. unmet needs) is only reported by older people who are disabled (i.e. those who reported having difficulty in at least one of the ADLs or IADLs) instead of the whole sample in the survey. We excluded a small number of observations (N = 26) of those who reported receiving formal care from a nurse or paid care worker from our final sample (N = 2,263) to reduce the potential bias to our findings. Table 1 shows the descriptive statistics of the study sample.
Variable specifications
Dependent variable: unmet need
An unmet need is related to the support received by a person given his or her needs, as well as the extent to which such support is satisfactory from the respondent's perspective. In the literature, scholars have defined two types of unmet need: (a) a subjective unmet need based on the person's own assessment of need (Allin et al., Reference Allin, Grignon and Le Grand2010; Kemper et al., Reference Kemper, Weaver, Short, Shea and Kang2007) and (b) an objective unmet need defined as whether the person receives any help with an activity in which he or she is limited due to disability (Tennstedt et al., Reference Tennstedt, McKinlay and Kasten1994; Shea et al., Reference Shea, Davey, Femia, Zarit, Sundström, Berg and Smyer2003; García-Gómez et al., Reference García-Gómez, Hernández-Quevedo, Jiménez-Rubio and Oliva-Moreno2015). In the analysis, we have chosen to focus on objective unmet need as the CHARLS lacks information on the subjective self-assessed unmet need. Furthermore, the subjective unmet need, e.g. a self-reported unmet need, has been widely used in a number of studies, and a recent study has found that the objective measure of an unmet need has a larger level of pro-poor inequity compared with the subjective measure of unmet need, suggesting some level of self-reporting bias on the basis of socio-economic position (García-Gómez et al., Reference García-Gómez, Hernández-Quevedo, Jiménez-Rubio and Oliva-Moreno2015). Hence, this paper considers the objective indicator of unmet need, which captures whether a disabled person (who has at least one limitation in ADLs or IADL) receives any care (Shea et al., Reference Shea, Davey, Femia, Zarit, Sundström, Berg and Smyer2003; Kemper et al., Reference Kemper, Weaver, Short, Shea and Kang2007; García-Gómez et al., Reference García-Gómez, Hernández-Quevedo, Jiménez-Rubio and Oliva-Moreno2015). In particular, the variable was constructed based on a two-level question in the survey uniquely structured to identify unmet needs among older adults in China. The first question asked if a person had difficulty in performing any ADLs or IADLs. If they reported having difficulty, the second question asked if they had received help with any of the ADLs or IADLs. Unmet need is thus a binary variable defined as whether one receives help with one or more ADLs or IADLs or not (García-Gómez et al., Reference García-Gómez, Hernández-Quevedo, Jiménez-Rubio and Oliva-Moreno2015). Following this definition, we constructed a dichotomous dependent variable for unmet need to measure the probability of having one or more ADL or IADL unmet needs, with 1 indicating having unmet needs and 0 indicating not having any unmet needs. ADL needs entail limitations in eating, bathing, dressing, toileting and transferring/walking and continence, while IADL needs entail limitations in doing household chores, preparing meals, shopping, managing money and taking medications. ADL is a set of validated indicators to measure functional disability among older people. It has been frequently used among institutionalised older people and older people with chronic illness (Katz et al., Reference Katz, Downs, Cash and Grotz1970). Since the CHARLS only surveys non-institutionalised older people, IADL is also included in the analysis to measure limitations of higher-order tasks necessary for independent living in the community or at home, such as doing housework, preparing meals and managing medications (Lawton and Brody, Reference Lawton and Brody1969; Ng et al., Reference Ng, Niti, Chiam and Kua2006).
Independent variables of interest: various levels of informal care intensity
We constructed two independent variables of interest in our analyses. The first independent variable of interest is a binary variable which indicates whether or not a disabled older person is receiving informal care. The second independent variable of interest in this study is the intensity of informal care received. We first calculated the total number of hours of informal care received per month from different types of informal carers. We subsequently categorised them into three groups: those who received a high intensity of care, a medium intensity of care and a low intensity of care. A high intensity of care is defined as receiving more than 200 hours of care per month, a medium intensity of care is defined as receiving between 81 and 200 hours of care per month, while a low intensity of care is defined as receiving 80 hours or less of care per month. The construction of these care-intensity proxies is based on a number of published peer-reviewed studies examining informal care intensity provided by different informal carers (Robards et al., Reference Robards, Vlachantoni, Evandrou and Falkingham2015; Kumagai, Reference Kumagai2017). This study calculated the number of hours of informal care provided by different informal carers and categorised this information into a high, medium or low level of care intensity. The assumption that we made in the analysis is that while the presence of informal care could help to ease the care burden, the discrepancies in care needs among the disabled older adults, if observed, would be attributed to the intensity of the informal care that they received.
Other independent variables
Based on the recent works that examined unmet needs among older people in China (Zhu, Reference Zhu2015; Zhu and Österle, Reference Zhu and Österle2017), we controlled for a set of health needs and non-needs variables in the regression model that are likely to affect unmet needs. Health needs variables include age, gender, number of ADL and IADL difficulties, and cognitive measurement. Age is a categorical variable that groups older adults into three groups: 45–59, 60–79, and 80 and above. Age 45–59 is used as the reference category. Gender is a binary variable with the female set as the reference category. Number of ADL and IADL limitations are count variables representing the number of ADL and IADL limitations as reported by the respondents. The cognitive measurement variable is a count variable that measures the number of correct answers that a respondent is able to provide from a total of 21 questions designed to assess their cognitive functioning. These 21 questions are categorised into three components: (a) Telephone Interview Cognitive Status which is based on the ability of an older person to state the date (day, month, year), day of the week, season of the year and serial subtractions from 100 (up to five times) correctly, and constitute a total of ten questions; (b) episodic memory score which assesses the immediate recall of the number of words after the interviewers read a list of Chinese nouns, and delayed recall after four to ten minutes, and constitute a total of ten questions; and (c) visuo-spatial ability in which respondents are shown a picture and are asked to draw a similar figure. A respondent's total score ranges from 0 to 21 (Li et al., Reference Li, Cacchione, Hodgson, Riegel, Keenan, Scharf, Richards and Gooneratne2017; Fu et al., Reference Fu, Li and Mao2018).
Non-health variables used in the analysis are: socio-economic variables, marital status, education, living arrangements, job status, per capita household equivalent income and provincial GDP per capita. Marital status comprises two sets of binary variables: married/co-habiting and not married, with married/co-habiting used as the reference category. Education is also constructed as a set of binary variables categorised as no education, elementary school education, middle school education, and high school education and above. No education is used as the reference category. Job status is also a binary variable which records a value of 1 if the person is currently working and 0 otherwise. Following earlier studies examining the extent of unmet needs among older people in China, we used household per capita equivalent income as the measurement of living standards (Zhu, Reference Zhu2015; Zhu and Österle, Reference Zhu and Österle2017). We constructed this variable by measuring the total household income and adjusted it by household size and the demographic composition of the household (i.e. number of adults and children) using the equivalence scale (Citro and Michael, Reference Citro and Michael1995). Three binary variables based on the level of household per capita equivalent income are constructed (less than 1,000 yuan per month, 1,001–4,500 yuan per month and more than 4,500 yuan per month), with less than 1,000 yuan per month used as the reference category. Region of residence is also a binary variable with 1 being an urban region and 0 being a rural region based on the respondents’ registration status as on his or her identification booklet (Hukou Footnote 1). We also included a regional economic variable as a proxy for regional care resources – GDP per capita of each province – and categorised them into provinces with low GDP per capita (less than 35,001 yuan per capita), provinces with lower,middle GDP per capita (35,001–45,000 yuan per capita), provinces with upper-middle GDP per capita (45,001–80,000 yuan per capita) and provinces with high GDP per capita (more than 80,000 yuan per capita) (Zhu and Österle, Reference Zhu and Österle2017). We use low GDP per capita as the reference category. Table 1 shows a summary of the variables used in the analysis.
Table 1. Descriptive statistics

Notes: SD: standard deviation. ADL: activity of daily living. IADL: instrumental activity of daily living. GDP: Gross Domestic Product. 1. ADL independent denotes that the older people have difficulties with IADL only. 2. ADL dependent denotes that the older people have difficulties in either ADL only or both ADL and IADL. 3. For the different informal care intensity categories, the number of observations are 2,116 (total), 1,333 (ADL independent) and 783 (ADL dependent). 4. Household per capita income is adjusted using the equivalence scale.
Empirical strategies
We conduct both descriptive and inferential analysis in this study. Our descriptive analysis maps out the average hours of informal care received by ADL statuses and the proportion of unmet needs among disabled older people by the informal care intensity that they received. We also plot two kernel density curves to ascertain if any systematic difference exists in the distribution of the total number of hours of informal care received each month between the same older adults who reported having unmet needs and those who reported no unmet needs.
Our inferential analysis employs Probit regression models to examine the association between informal care intensity and unmet needs among disabled older people in China, controlling for a set of co-variates (health needs and non-health needs variables) that are likely to influence their unmet needs. Following Wooldridge (Reference Wooldridge2013), we estimate the following regression:
where Y denotes the predicted probability of unmet needs (1 = having unmet needs, 0 otherwise), Φ denotes the cumulative normal distribution function, IC denotes informal care and X is the vector that captures all other independent variables for Y.
We analysed the marginal effects at means of unmet needs to show how the predicted probabilities of different levels of informal care change from 0 to 1 by holding all other explanatory variables at their means.
We first analyse the predicted probabilities of the entire pool of disabled older people who received informal care, before disaggregating them into two sub-groups: ADL dependent and ADL independent. The ADL dependent group includes the disabled older people who have difficulties in ADLs only or both ADLs and IADLs. The ADL independent group includes those who have difficulties in IADLs only. Differentiating those who are ADL independent from ADL dependent allows us to determine the extent to which care intensity has the propensity to lower the unmet needs of the older people based on their functional status when holding all other variables constant.
We also perform two sets of robustness checks for each Probit regression model. The first robustness check replaces the independent variable of interest, which is categorical variables of informal care intensity (low, medium, high), with a logarithmic form of the continuous variable of ‘total number of informal care hours received per month plus one’. The second robustness check replaces the ‘cognitive assessment’ variable with the ‘number of total words recalled’ variable, which is one out of the three components in the cognitive assessment and has a score range from 0 to 10 (episodic memory) (see the online supplementary material).
Results
Our descriptive analysis in Table 2 shows the average total number of informal care hours received by a disabled older person each month based on different levels of care intensity. Our results show that approximately 6.5 per cent of the disabled people report having received no informal care at all. Most people receive less than 80 hours of informal care irrespective of whether they are ADL dependent or not. Specifically, 39.44 per cent of the people who are ADL dependent and 52.15 per cent of the people who are ADL independent receive a low intensity of care – an average of 38.46 hours per month. For the whole sample, less than a quarter of the disabled older people receive a high intensity of care. For those who are ADL dependent, only 32.23 per cent of them received a high intensity of care (see Table 2). In terms of unmet needs, 30.61 per cent of disabled older persons who do not receive any informal care report having unmet needs. This appears to be slightly higher than those who report receiving low-intensity care (22.12%), medium-intensity care (22.73%) and high-intensity care (20.14%) (see Figure 1).

Figure 1. Percentage of unmet needs for disabled older adults by level of care intensity.
Note: N = 2,263.
Table 2. Total number of informal care hours received each month by care intensity

Notes: ADL: activity of daily living. IADL: instrumental activity of daily living. 1. ADL independent denotes that the older people have difficulties with IADL only. 2. ADL dependent denotes that the older people have difficulties in either ADL only or both ADL and IADL. 3. The average number of informal care hours received per month is disaggregated by different levels of informal care intensity (low, medium, high).
We plotted kernel density estimations of the total number of informal care hours received per month by older adults and compared those with and without unmet needs in Figure 2. The probability density function shows clearly that there is no systematic difference in terms of the total number of care hours received per month between those with and without unmet needs, meaning that no matter how many hours of care a disabled older person receives, the probability of them reporting having unmet needs does not differ significantly.
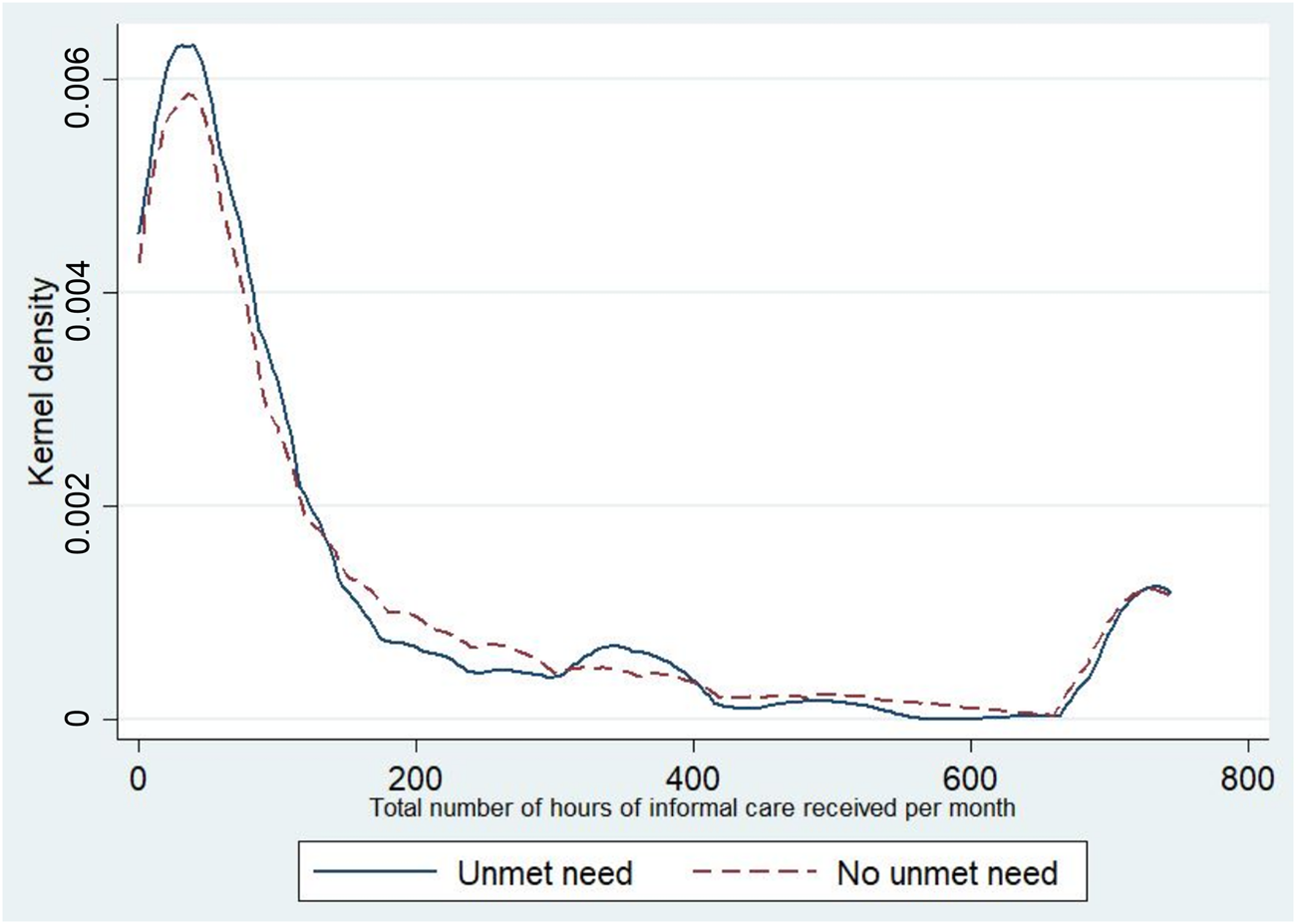
Figure 2. Kernel density estimation of total number of informal care hours received per month between older adults with or without unmet needs and who experienced difficulties in managing their daily living.
Table 3 reports the marginal effects at means of unmet needs among disabled older adults who received informal care. For the whole sample and those who are ADL independent (no functional limitations), receiving some form of informal care had lower predicted probabilities of unmet needs when comparing with disabled older adults who received no informal care. Interestingly, this relationship does not hold for those who are ADL dependent (with functional limitations). In other words, receiving informal care does not lead to lower unmet needs for older people with functional limitations.
Table 3. Marginal effects at means of unmet needs among older adults who experienced difficulties in managing their daily living in China

Notes: ADL: activity of daily living. IADL: instrumental activity of daily living. SE: standard errors. Ref.: reference category. GDP: Gross Domestic Product. 1. ADL independent denotes that the older people have difficulties with IADL only. 2. ADL dependent denotes that the older people have difficulties in either ADL only or both ADL and IADL. 3. Household per capita income is adjusted using the equivalence scale.
Significance levels: * p < 0.1, ** p < 0.05, *** p < 0.01.
There appear to be distinct differences in several control variables that influence unmet needs. For those who are ADL independent, in other words have no functional limitations, being in an older age group (age 60–79) increased the predicted probabilities of reporting unmet needs as opposed to the reference group (age 45–59). Living in an urban area is closely associated with lower predicted probabilities of unmet needs as compared to living in rural areas. Other factors, such as the number of IADL limitations and being unmarried, increase the predicted probabilities of reporting unmet needs. For the ADL dependent group, being in rural area, living alone and with low cognitive scores increased the predicted probabilities of reporting unmet needs.
We further test the effects of intensity of care on unmet needs, as shown in Table 4. Here, we are interested in knowing whether intensity of care has any effects on unmet needs. Our results show that among those who are ADL independent, receiving higher intensities of informal care lowers the predicted probabilities of unmet needs significantly. Specifically, receiving a medium intensity of care lowers the predicted probability of unmet needs by 5.2 per cent (p < 0.05), whereas receiving a high intensity of care lowers the predicted probability of unmet needs by 7.1 per cent (p < 0.01) compared with those who received a low intensity of care. These effects, nevertheless, are not significant among those who are ADL dependent. In other words, for those who have functional limitations, receiving a higher intensity of care has no significant effect on reducing unmet needs.
Table 4. Marginal effects at means of unmet needs among older adults who received informal care and experienced difficulties in managing their daily living in China

Notes: ADL: activity of daily living. IADL: instrumental activity of daily living. SE: standard errors. Ref.: reference category. GDP: Gross Domestic Product. 1. ADL independent denotes that the older people have difficulties with IADL only. 2. ADL dependent denotes that the older people have difficulties in either ADL only or both ADL and IADL. 3. Household per capita income is adjusted using the equivalence scale.
Significance levels: * p < 0.1, ** p < 0.05, *** p < 0.01.
We performed two robustness checks for our analysis. The first robustness check replaces the informal care variable with a logarithmic form of the total number of informal care hours received by an older adult per month (continuous variable) plus 1. The second robustness check uses theh ‘total number of words recalled’ variable as the cognitive measurement. We observe similar trends for both robustness checks as with our main results (see the online supplementary material).
Discussion and conclusion
This study is among the first to investigate the relationship between informal care and unmet needs among disabled older people in China. We found that the majority of disabled older people receive a low intensity of informal care, and for those with IADL limitations, receiving informal care tends to lower the probabilities of reporting unmet needs when compared to not receiving informal care. We do not observe the same effects of informal care on unmet needs for older people with functional limitations (ADL limitations). Similarly, higher intensities of informal care do not translate into lower predicted probabilities of unmet needs for those with functional limitations.
The findings from this study give rise to a number of important policy implications with regard to LTC in China. First, even though a previous study showed that having informal care support is able to lower the odds of unmet needs among disabled older adults (Zhu and Österle, Reference Zhu and Österle2017), we have found mixed results. In particular, we do not observe any significant associations between a high intensity of care and low unmet needs for those with functional limitations. This suggests that disabled older people who experienced difficulties managing basic dimensions of their daily living have more care needs and may require care provision that is much more intense and onerous from the care-givers. At the same time, this could also indicate that most informal carers may not be equipped to provide adequate care to their disabled family members despite devoting up to six or seven hours of their time on care provision every day. In view of this, there is a pressing need for the government to buttress the formal care institutions and delivery systems to support the 33 million incapacitated older people who need advanced care (Liu and Sun, Reference Liu and Sun2015), as well as to help the informal carers overcome care-giver fatigue. Internationally, scholars have called for a recalibration of the interface between the formal and informal LTC systems. For instance, the deployment of professional care-givers from the formal health system, such as home care nurses, rehabilitation therapists and social workers, to the community is seen as a necessary move to support and supervise untrained informal carers in fast ageing societies (Tao and McRoy, Reference Tao and McRoy2015). In European countries, many governments are looking into changing their policy priorities to cut back on formal care provision and to promote ‘age at home’ or ‘age in place’ for those who need intensive care. This change has also given rise to the importance of care-giving, especially in Southern European countries such as Portugal and Spain which still uphold strong traditions of family care-giving (Broese van Groenou and De Boer, Reference Broese van Groenou and De Boer2016; La Porte and McMahon, Reference La Porte, McMahon and Scheffler2016). To this end, some European countries are fast adopting a mixed provision of the formal and informal care model, in which collaboration between professional health actors and informal carers is established to complement one another in order to strengthen the entire long-term care delivery systems for older people (Litwin and Attias-Donfut, Reference Litwin and Attias-Donfut2009; Geerts and Van den Bosch, Reference Geerts and Van den Bosch2012; Verbeek-Oudijk et al., Reference Verbeek-Oudijk, Woittiez, Eggink and Putman2014; Hengelaar et al., Reference Hengelaar, Hartingsveldt, Wittenberg, Etten-Jamaludin, Kwekkeboom and Satink2017; Wimo et al., Reference Wimo, Elmståhl, Fratiglioni, Sjölund, Sköldunger, Fagerström, Berglund and Lagergren2017). Similar measures should be adopted by the Chinese government so that the burden of care will not be predominantly shouldered by informal carers.
Second, the lack of significant associations between care and unmet needs for those who are ADL dependent suggests that an average of six to seven hours of care on a daily basis by an informal carer has not been able to address significantly the needs of the majority of older adults with functional disabilities. This implies that there is a need for policy makers and practitioners to rethink new strategies that could bridge the capacity deficit gaps among informal carers, especially those in home-based settings. While our analysis is unable to ascertain if any skills deficits or personal care issues among the carers exist, a recent study on care-givers for older people with Alzheimer's disease in China indicated high levels of care burden lead to the presence of mental health issues among carers (Liu et al., Reference Liu, Li, Shi, Wang, Zhou, Liu, Liu, Yu and Ji2016). Another study found that training informal care-givers of patients who had had a stroke improved the patients’ quality of life and reduced costs (Stevenson, Reference Stevenson2004). In light of high care-giving burdens, interventions to provide training and support to informal carers, especially those who provide intensive care, need to be implemented in the future.
Third, the under-provision of informal care for disabled older adults in China is likely to be a result of the rapid urbanisation in China which results in occupational migration to metropolitan areas for many prospective adult carers, leaving family members who need care with limited social support at home (Lin et al., Reference Lin, Yin and Loubere2014). In addition, the implications of the one-child policy for informal care-giving in China should also be considered. Even though this policy was reversed in 2013, the socio-economic impacts of this policy are far-reaching. Rapid urbanisation and the one-child policy in China directly or indirectly affect the kinship-based familial structure and informal care-giving patterns in China, and suggest the decline of a support structure for the current older generation. This situation is all the more prevalent in rural areas compared to urban areas. Therefore, there is a need for the government to find a way to compensate informal carers or help older people to ‘age in place’. Experiences from established LTC systems in Europe suggest that cash benefits for recipients and informal carers for disabled older people who need care at home was more popular than direct service reimbursement (Campbell et al., Reference Campbell, Ikegami and Gibson2010; Da Roit and Le Bihan, Reference Da Roit and Le Bihan2010; Rhee et al., Reference Rhee, Done and Anderson2015). Nonetheless, closer to China, Japan and Korea have decided to reimburse eligible recipients for direct services such as home care, community-based care and institutional care only, without handing out cash for various social cultural reasons (Tamiya et al., Reference Tamiya, Noguchi, Nishi, Reich, Ikegami, Hashimoto, Shibuya, Kawachi and Campbell2011; Rhee et al., Reference Rhee, Done and Anderson2015).
Last but not least, our findings echo previous studies, showing that older people living in rural areas or from poorer regions are more likely to report having higher unmet needs or having lesser access to care services (Li et al., Reference Li, Zhang, Zhang, Zhang, Zhou and Chen2013; Hu and Wang, Reference Hu and Wang2019). This is not surprising given the fact that the number of potential care-givers in rural areas is shrinking, and many older people from rural areas are geographically distant from their children and grandchildren who may have migrated to urban cities. As many LTC sources are mostly concentrated in affluent urban areas (Feng et al., Reference Feng, Liu, Guan and Mor2012), it is important for the government to address the issue of the shortage of formal LTC services in rural and under-developed areas. Attention should also be paid to promote home- and community-based care in rural areas, and the government should direct more funding towards the development of LTC in poor rural areas.
The findings should be interpreted bearing in mind several limitations. First, this study relies on self-reported measures, which may be subjected to recall bias or inaccuracy in reporting during the interview process. However, this should not pose a major concern as previous studies have demonstrated no association between under-reporting and demographic characteristics other than age (Tsui et al., Reference Tsui, Leung, Woo, Choi and Lo2005; Bhandari and Wagner, Reference Bhandari and Wagner2006). Second, the data used are not sufficiently detailed to measure all aspects of home- and community-based LTC use. It is possible that a small proportion of older people may experience concurrent use of these LTC services that are not captured by the survey. This makes it difficult for us to gauge whether the analysis is able to capture the real effects of informal care on unmet needs. An inquiry would be necessary to decipher the nuances of long-term formal and informal care received by older adults in China and how these different types of care affect their care needs. Third, future research is needed to examine the causal relationship between informal care intensity and unmet needs among disabled older people as we are unable to establish a causality due to the cross-sectional nature of the data and the empirical strategies we used.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X1900148X.
Acknowledgements
The authors are grateful for the support provided by the UK Economic and Social Research Council through a research grant titled ‘Who will care for you when you get old? A study of inequities in health and long-term care among the elderly in rural China’. The authors would like to thank the editor and two anonymous reviewers for their constructive comments which helped to improve this paper.
Financial support
This work was supported by the UK Economic and Social Research Council (grant number ES/N002717/2).
Conflict of interest
The authors declare no conflicts of interest that are relevant to the content of this paper.
Ethical standards
Ethical approval is not required for this research as the analysis is based on publicly available data.








