Introduction
On a global scale, the proportion of older adults in the population is growing at an unprecedented rate. Importantly, with our population's increasing age comes an increase in the prevalence of dementia (Prince et al., Reference Prince, Bryce, Albanese, Wimo, Ribeiro and Ferri2013, Reference Prince, Ali, Guerchet, Prina, Albanese and Yu2016; Duong et al., Reference Duong, Patel and Chang2017; World Health Organization, 2017; Wu et al., Reference Wu, Beiser, Breteler, Fratiglioni, Helmer, Hendrie, Honda, Ikram, Langa, Lobo, Matthews, Ohara, Pérès, Qiu, Seshadri, Sjölund, Skoog and Brayne2017). As dementia affects an increasing number of people, associated direct and indirect costs are also increasing (Wimo et al., Reference Wimo, Winblad and Jönsson2010, Reference Wimo, Guerchet, Ali, Yu, Prina, Winblad, Jönsson, Liu and Prince2017; Wong et al., Reference Wong, Gilmour and Ramage-Morin2016; Cloutier et al., Reference Cloutier, Penning, Nuernberger, Taylor and MacDonald2017).
Dementia literacy, defined as beliefs and knowledge about dementia that promote recognition, management or prevention of the condition (Low and Anstey, Reference Low and Anstey2009), is, therefore, of importance to our society (Annear et al., Reference Annear, Toye, McInerney, Eccleston, Tranter, Elliott and Robinson2015). Care-givers of individuals with dementia as well as laypersons tend to have insufficient knowledge about dementia (Low and Anstey, Reference Low and Anstey2009; McParland et al., Reference McParland, Devine, Innes and Gayle2012; Cahill et al., Reference Cahill, Pierce, Werner, Darley and Bobersky2015; Glynn et al., Reference Glynn, Shelley and Lawlor2017; Cations et al., Reference Cations, Radisic, Crotty and Laver2018). For example, laypersons often believe the myth that dementia is a normal part of ageing (Cahill et al., Reference Cahill, Pierce, Werner, Darley and Bobersky2015; Cations et al., Reference Cations, Radisic, Crotty and Laver2018).
Of note, demographic characteristics may also be related to one's general dementia knowledge. Dementia knowledge, for instance, is greater among younger adults and those with relatively higher levels of education (Sahin et al., Reference Sahin, Gurvit, Emre, Hanagasi, Bilgic and Harmanci2006; Li et al., Reference Li, Fang, Su, Liu, Xiao and Xiao2011). While general dementia knowledge does not differ by gender, women tend to have greater awareness of specific dementia symptoms compared to men (Sahin et al., Reference Sahin, Gurvit, Emre, Hanagasi, Bilgic and Harmanci2006).
Given that dementia primarily affects older adults, it is important to consider negative attitudes and stereotypes towards ageing. According to the Social Identity Theory (Tajfel and Turner, Reference Tajfel, Turner, Austin and Worchel1979), people seek to define the group to which they belong in positive terms and the opposing group, to which they do not belong, in negative terms. When applied to ageing, we can see how younger adults may project negative attitudes on to older adults to promote a more positive image of their own group of younger adults (Harwood, Reference Harwood2007). Terror Management Theory (Greenberg et al., Reference Greenberg, Pyszczynski, Solomon and Baumeister1986) offers another explanation for negative attitudes towards ageing. According to this theory, we avoid situations that remind us that death is inescapable. In terms of ageing, this theory suggests that younger adults avoid situations involving older adults, including older adults with dementia (O'Connor and McFadden, Reference O'Connor and McFadden2012), as a way of preserving the belief that death is only a distant possibility. It has been suggested that, by psychologically distancing themselves from older adults, younger adults may be able to have more positive attitudes about ageing (Calasanti, Reference Calasanti2005).
Attitudes towards ageing can be influenced by a myriad of factors. For example, increased knowledge about ageing leads to reduced anxiety about ageing and, subsequently, to fewer negative attitudes towards older adults (Allan and Johnson, Reference Allan and Johnson2008). Similarly, increased contact with older adults reduces these negative attitudes (Schuldberg, Reference Schuldberg2005). However, the type of contact is of relevance: persons residing with older adults have more anxiety about ageing compared to persons who have regular contact with older persons in their work environment (Allan and Johnson, Reference Allan and Johnson2008). Age also plays a role in attitudes towards ageing. That is, negative attitudes towards ageing are prevalent in younger and middle-aged adults but not in older adults (Kite et al., Reference Kite, Stockdale, Whitley and Johnson2005).
Attitudes towards ageing also tend to influence attitudes about dementia because people believe that dementia is a normal part of ageing (Corner and Bond, Reference Corner and Bond2004). Thus, people with negative attitudes about ageing may also have more negative dementia attitudes. Moving beyond attitudes towards ageing, dementia generally has been associated with negative attitudes (Jolley and Benbow, Reference Jolley and Benbow2000; Sahin et al., Reference Sahin, Gurvit, Emre, Hanagasi, Bilgic and Harmanci2006).
These negative attitudes can be related to demographic characteristics. That is, attitudes towards dementia may vary by age and level of educational attainment (Heese, Reference Heese2015). For example, younger adults have more positive attitudes towards dementia than older adults (Cheston et al., Reference Cheston, Hancock and White2016). On the other hand, middle-aged adults are more likely to be ashamed of having family members with dementia than are younger and older adults (Zhang et al., Reference Zhang, Loi, Zhou, Zhao, Lv, Wang, Wang, Lautenschlager, Yu and Wang2017). Contact with persons with dementia increases positive attitudes towards dementia (Cheston et al., Reference Cheston, Hancock and White2018). Finally, people with more dementia knowledge tend to have more positive attitudes towards dementia (Song, Reference Song2002; Lee, Reference Lee2012).
Personhood, a construct that is closely related to attitudes towards ageing and dementia, has been conceptualised as ‘a standing or status that is bestowed upon one human being, by others, in the context of relationship and social being … impl[ying], recognition, respect, and trust’ (Kitwood, Reference Kitwood1997: 8). If an individual is unable to communicate information verbally about his or her life because of dementia, it may become more challenging to ascribe personhood to that individual. In fact, persons with dementia tend to be ascribed less personhood than those without dementia (Miron et al., Reference Miron, McFadden, Hermus, Buelow, Nazario and Seelman2017). As well, dementia care decisions can be influenced by personhood perceptions (Malloy and Hadjistavropoulos, Reference Malloy and Hadjistavropoulos2004; Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013).
Our primary goal was to assess systematically whether attitudes towards ageing and a person's age influenced attitudes and perceptions regarding dementia. We also examined the influence of care-giver status, dementia knowledge, gender and education on attitudes towards dementia and personhood perceptions.
Methodology
Participants
Eligible participants included those who were between 18 and 35 years (i.e. younger adults), between 40 and 60 years (i.e. middle-aged adults) and over 65 years (i.e. older adults), including informal care-givers of at least one older adult with dementia. In order to maximise sample representativeness by not relying on a local sample, participants were recruited through the online Qualtrics panels system (https://www.qualtrics.com/). This widely adopted method of recruitment is increasingly used by many North American research universities (e.g. Tomfohrde and Reinke, Reference Tomfohrde and Reinke2016; Ammaturo et al., Reference Ammaturo, Hadjistavropoulos and Williams2017; Torres et al., Reference Torres, Yadav and Khan2017). The Qualtrics panels system maintains a database of several million North American residents and use of this system maximises sample representativeness by including a variety of participants from across North America who match the target demographic. Sampling strategies used by Qualtrics panels also minimise biases inherent in recruiting samples from the local community. In other words, Qualtrics panels have access to a more diverse demographic than can be found locally. Before they participate in a study through Qualtrics panels, potential participants complete detailed questionnaires about their demographics such as age, gender and level of education. This information is checked for accuracy by Qualtrics panels before potential participants are approved for the study. Checks for data accuracy are also incorporated throughout the survey. Incentive programmes are provided by Qualtrics panels to reward participants and promote engagement in research studies.
Qualtrics used a data-sampling method involving demographic screening questions (to assess eligibility for participation in this study based on age, gender and care-giving status) and our desired sample size. Compensation for participation in this study was provided via Qualtrics panels. Prior to participating in this study, participants provided informed consent. All information obtained as part of the study was kept confidential. Approval for this study was granted by our institutional ethics review board.
Measures
Demographics Information Sheet
The Demographic Information Sheet included questions about age, gender, level of education and contact with persons with dementia.
Dementia Knowledge Questionnaire
The Dementia Knowledge Questionnaire (DKQ; Graham et al., Reference Graham, Ballard and Sham1997) is a measure used to assess knowledge about dementia. We used a modified version of the DKQ that consisted of seven questions with the highest possible total score being 16. Knowledge in the areas of basic knowledge, epidemiology, symptoms and causes of dementia is assessed throughout the questionnaire. The DKQ has good predictive validity when comparing care-givers with varying degrees of contact with services for older adults with dementia (Graham et al., Reference Graham, Ballard and Sham1997). That is, care-givers in contact with an Alzheimer's support group were the most knowledgeable and care-givers with no contact with mental health services for older adults were the least knowledgeable.
Dementia Attitudes Scale
The Dementia Attitudes Scale (DAS; O'Connor and McFadden, Reference O'Connor and McFadden2010) is a measure of attitudes towards dementia. It consists of 20 items with a two-factor structure. Items in Factor 1 (i.e. social comfort) address the affective and behavioural domains of dementia while items in Factor 2 (i.e. dementia knowledge) address the cognitive domain. Higher scores on this scale are indicative of more positive attitudes. The measure was validated among college students and certified nursing assistant students. Cronbach's alpha values for the DAS were between 0.83 and 0.85. Significant correlations were reported between the DAS and other relevant measures (e.g. Attitudes Toward Old People Scale – Kogan, Reference Kogan1961; Scale of Ageism – Fraboni et al., Reference Fraboni, Saltstone and Hughes1990), providing supportive evidence of convergent validity for the DAS. Further evidence of construct validity is supported by the finding that more frequent contact with persons with dementia was positively correlated with more positive attitudes on the DAS (Jackson et al., Reference Jackson, Cherry, Smitherman and Hawley2008). In our study, both the social comfort and dementia knowledge sub-scales of the DAS had good internal reliability with Cronbach's alpha values of 0.811 and 0.817, respectively.
Ambivalent Ageism Scale
The Ambivalent Ageism Scale (AAS; Cary et al., Reference Cary, Chasteen and Remedios2017) is a 13-item measure of attitudes towards older adults. The measure includes two sub-scales: benevolent items represent patronising behaviours and paternalistic attitudes, and hostile items represent hostile behaviours and attitudes towards older adults. The AAS is a psychometrically sound instrument with good test–retest reliability (α = 0.80) and excellent internal consistency (α = 0.91). The AAS was shown to be highly correlated with the Fraboni Scale of Ageism (FSA; Fraboni et al., Reference Fraboni, Saltstone and Hughes1990). High hostile ageist beliefs are linked to a perception of older adults as cold and incompetent, regardless of benevolent beliefs (Cary et al., Reference Cary, Chasteen and Remedios2017). In contrast, low hostile ageist beliefs and high benevolent ageist beliefs are accompanied by a perception of older adults as warm and incompetent (Cary et al., Reference Cary, Chasteen and Remedios2017). This finding is of relevance because it reveals that the two sub-scales predict warmth and competence in different ways. In our study, the benevolent and hostile sub-scales of the AAS had good internal reliability with Cronbach's alpha values of 0.899 and 0.879, respectively.
Personhood in Dementia Questionnaire
The Personhood in Dementia Questionnaire (PDQ; Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013) is a 20-item measure of health-care professionals’ person-centred attitudes towards those with dementia. The PDQ is comprised of ten themes centring on personhood (e.g. emotional capacity, cognitive capacity, personality, psychological continuity; Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013). For the purposes of this study, since informal care-givers and laypersons were asked to complete this questionnaire rather than only health-care professionals, the term ‘residents’ was replaced with ‘individuals’ in the PDQ. The PDQ has been found to have a Cronbach's alpha value of 0.79 (Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013). The Pearson product-moment correlation between the PDQ and a modified version of the personhood sub-scale of the Person-directed Care measure showed moderate convergent validity (Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013). The PDQ has been shown to predict clinical care intentions (Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013), long-term care staff resilience (Williams et al., Reference Williams, Hadjistavropoulos, Ghandehari, Malloy, Hunter and Martin2015) and long-term care staff burnout (Hunter et al., Reference Hunter, Hadjistavropoulos, Thorpe, Malloy and Lix2016). In our study, the PDQ had good internal reliability with a Cronbach's alpha value of 0.857.
Procedure
Prior to beginning the study, participants completed a demographic information sheet which included questions about age, gender, level of education and contact with persons with dementia. First, participants completed the DKQ to capture their existing dementia knowledge (i.e. DKQ1). Second, information about dementia (see Table 1) was presented to participants in audio and written form. This was done in order to ensure that participants had a reasonable understanding of dementia prior to filling out the various questionnaires. Third, participants completed the DKQ a second time (i.e. DKQ2) to examine if their dementia knowledge increased as a result of being presented with the information about dementia. Finally, participants completed the AAS, DAS and PDQ to assess attitudes towards ageing, attitudes towards dementia and personhood perceptions, respectively.
Table 1. Dementia information

Statistical analyses
All dependent variables were screened for accuracy of data entry and missing values through the examination of descriptive statistics. Values for each variable were within range. Means and standard deviations (SD) for each variable were plausible. Missing values were not identified. The variables were then examined for univariate outliers. As recommended by Tabachnick and Fidell (Reference Tabachnick and Fidell2013), cases in which standardised z-scores exceeded 3.29 were considered as potential univariate outliers. Univariate outliers were not identified.
Finally, an examination of histograms, skewness and kurtosis statistics, and probability plots for comfort around people with dementia, knowledge about dementia and personhood perceptions was carried out. Residual plots for each of the dependent variables suggested an adequate normality assumption for the regression model. Pairs plots suggested negative associations between attitudes towards ageing and each of the dependent variables (see Figure 1). Boxplots provided a comparison of the distributions of the dependent variables by care-giver status, age groups, gender and education (see Figure 2).

Figure 1. Pairs plots showing correlations between attitudes towards ageing, attitudes towards dementia and personhood perceptions.
Notes: AAS: Ambivalent Ageism Scale. DAS: Dementia Attitudes Scale. PDQ: Personhood in Dementia Questionnaire.

Figure 2. Boxplots comparing the distributions of each dependent variable by age groups, care-giver status, gender and education.
Notes: DAS: Dementia Attitudes Scale. PDQ: Personhood in Dementia Questionnaire.
As a manipulation check, differences in dementia knowledge prior to (mean = 7.5459, SD = 2.92521) and following (mean = 13.3367, SD = 3.72777) the presentation of dementia information was examined. This was done to ensure that our educational intervention was successful in increasing dementia knowledge. A paired-samples t-test was conducted. As expected, a significant main effect of dementia knowledge before and after the presentation of dementia-related information was found, t(195) = −23.542, p < 0.001.
For the primary analysis, a series of multiple regression models were conducted to examine if attitudes towards ageing, age groups, care-giver status, dementia knowledge, gender and education predicted attitudes towards dementia and personhood perceptions. Interactions between age group and dementia knowledge were also investigated. A separate multiple regression model was carried out for each dependent variable (i.e. DAS – Comfort, DAS – Knowledge, PDQ). For each multiple regression model, the full model as well as each independent variable's unique contribution to the dependent variable after all other independent variables have been controlled for was examined.
Results
The final sample included 196 participants. The sample's demographic characteristics are summarised in Table 2. Relevant means and standard deviations across age groups and care-giver status are presented in Table 3. For each of the three response variables (i.e. comfort around people with dementia, knowledge about dementia, personhood perceptions), a multiple regression model was fitted. The independent variables included attitudes towards ageing, age groups, care-giver status, dementia knowledge prior to and following the presentation of dementia information, gender, education, and the interaction between age groups and dementia knowledge prior to the presentation of dementia information. Prior to these analyses, attitudes towards ageing and dementia knowledge were centred to be more representative of scores across age groups.
Table 2. Frequencies for demographic characteristics of the sample

Table 3. Relevant means and standard deviations (SD) for the sample

Notes: DAS: Dementia Attitudes Scale. PDQ: Personhood in Dementia Questionnaire.
Tables 4–6 show the regression models that were fitted. Each of the three response variables were significantly predicted by the full model, p < 0.001. Thus, an examination of each independent variable's unique contribution to the full model was carried out for each response variable. Age groups, gender and education were not associated with any of the response variables. Significant associations for each of the response variables are discussed in the paragraphs below.
As shown in Table 4, attitudes towards ageing (p < 0.001), care-giver status (p < 0.001), dementia knowledge prior to the presentation of dementia information (p < 0.05), and the interaction between age groups and dementia knowledge prior to the presentation of dementia information (p < 0.05) made independent and unique contributions to the full model predicting DAS – Comfort scores. That is, more negative attitudes towards ageing were a significant predictor of less comfort around people with dementia. Care-givers (compared to non-care-givers) were more comfortable around people with dementia. Those who had greater knowledge about dementia prior to the presentation of dementia information were less comfortable around people with dementia. However, upon examination of the interaction of dementia knowledge and age group, it was revealed that older adults who had greater knowledge about dementia prior to the presentation of dementia information were more comfortable around those with dementia compared to their older adult counterparts who had less prior dementia knowledge.
Table 4. Results for the linear regression model for comfort around people with dementia (Dementia Attitudes Scale – comfort)

Notes: AAS: Ambivalent Ageism Scale. DKQ1: first administration of the Dementia Knowledge Questionnaire. DKQ2: second administration of the Dementia Knowledge Questionnaire. SE: standard error.
As shown in Table 5, attitudes towards ageing (p < 0.001) and care-giver status (p < 0.001) made independent and unique contributions to the full model predicting DAS – Knowledge scores. More negative attitudes towards ageing was a significant predictor of less knowledge about dementia. Care-givers had more knowledge about dementia compared to non-care-givers.
Table 5. Results for the linear regression model for knowledge about dementia (Dementia Attitudes Scale – knowledge)

Notes: AAS: Ambivalent Ageism Scale. DKQ1: first administration of the Dementia Knowledge Questionnaire. DKQ2: second administration of the Dementia Knowledge Questionnaire. SE: standard error.
As shown in Table 6, attitudes towards ageing (p < 0.05) and care-giver status (p < 0.001) made independent and unique contributions to the prediction of PDQ scores. More negative attitudes towards ageing was a significant predictor of ascribing less personhood to persons with dementia. Compared to non-care-givers, care-givers ascribed more personhood to persons with dementia.
Table 6. Results for the linear regression model for personhood perceptions (Personhood in Dementia Questionnaire)
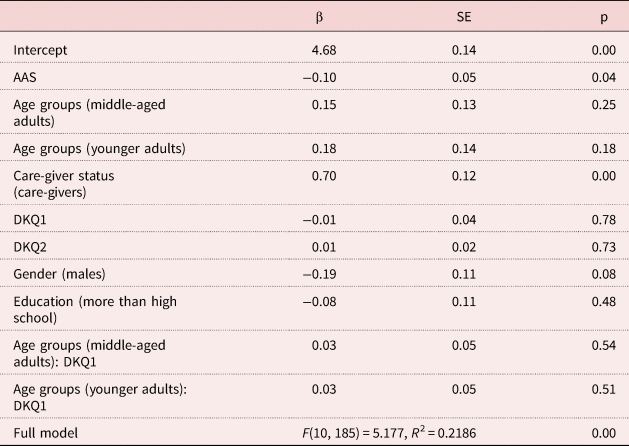
Notes: AAS: Ambivalent Ageism Scale. DKQ1: first administration of the Dementia Knowledge Questionnaire. DKQ2: second administration of the Dementia Knowledge Questionnaire. SE: standard error.
Discussion
This study involved a systematic evaluation of differences in attitudes towards dementia and personhood perceptions as a function of age, attitudes towards ageing and care-giver status. The influence of dementia knowledge, gender and education was also examined. Age-related differences in attitudes towards dementia and related personhood perceptions have not been investigated previously in a systematic fashion. Thus, evaluation of age-related differences in perceiving people with dementia makes a novel contribution to the literature.
Impact of age- and care-giver-related variables on attitudes towards and perceptions of dementia
While the Social Identity Theory (Tajfel and Turner, Reference Tajfel, Turner, Austin and Worchel1979) suggests that younger adults would likely have more negative attitudes towards older people (and, consequently, towards dementia) when compared to middle-aged and older adults, the Terror Management Theory (Greenberg et al., Reference Greenberg, Pyszczynski, Solomon and Baumeister1986) suggests that younger adults would likely have more positive attitudes because they are able to psychologically distance themselves from older adults (Calastanti, Reference Calasanti2005). Contrary to our expectation, findings from this study did not provide support for either of these theories within the context of attitudes towards older people with dementia. That is, being a younger adult was not significantly associated with being more comfortable around persons with dementia, having more knowledge about dementia or ascribing higher personhood to those with dementia.
It is possible that age itself was not as salient a factor in predicting attitudes towards dementia and personhood perceptions as attitudes towards ageing. That is, our study demonstrated that more negative attitudes towards ageing was predictive of less comfort around people with dementia, less knowledge about dementia and lower ascribed personhood to those with dementia. Thus, regardless of age, attitudes towards ageing appear to play a central role in attitudes and perceptions regarding dementia. As well, those with more dementia knowledge prior to the presentation of dementia information were likely to be more comfortable around people with dementia. When controlling for this prior dementia knowledge, older adults appeared to be significantly more likely to be comfortable around persons with dementia than their younger or middle-aged counterparts.
In addition to age-related factors, we studied the role of care-giver status in attitudes towards dementia and personhood perceptions. In our study, being a care-giver was predictive of being more comfortable around people with dementia and having more knowledge about dementia. This is consistent with previous research reporting more positive attitudes towards dementia being associated with more dementia contact (e.g. Moyle et al., Reference Moyle, Murfield, Griffiths and Venturato2011; Cheston et al., Reference Cheston, Hancock and White2018). Seeing as care-givers spend more time with older adults with dementia, it was also expected that care-givers would ascribe higher levels of personhood to those with dementia compared to non-care-givers (Wimo et al., Reference Wimo, von Strauss, Nordberg, Sassi and Johansson2002). Our findings were consistent with this hypothesis. That is, care-giver status was predictive of personhood perceptions, with care-givers ascribing higher levels of personhood to those with dementia compared to non-care-givers. This finding may be explained by the increased contact that care-givers have with persons with dementia compared to dementia-related contact of non-care-givers. Care-givers in this study had at least one family member with dementia and were in contact with this family member at least once per month. This interaction creates opportunities for care-givers to provide person-centred care, which has been shown to effectively increase the likelihood of ascribing personhood in those with dementia (Moyle et al., Reference Moyle, Murfield, Griffiths and Venturato2011).
Directions for future research
Several limitations should be considered when interpreting findings from this study. Online recruitment may lead to limited generalisability of the findings. For example, persons without internet access would have been excluded from the study. In future studies, participants could also be recruited within the local community to include those without internet access. Moreover, the findings from our study are correlational in nature. Thus, further experimental investigations in this area would provide a clearer and more comprehensive understanding of differences in attitudes towards dementia and personhood perceptions. A longitudinal study could be carried out to assess the effects of attitudes towards ageing, age and care-giver status over a longer period of time. Given that attitudes towards ageing and care-giver status were consistently predictive of attitudes towards dementia and personhood perceptions, future investigations could examine whether the presentation of information that tackles ageist beliefs and/or increased opportunities to care for older adults with dementia improves attitudes towards and perceptions of those who have dementia. Finally, the measurement of attitudes through the use of self-report scales does not necessarily translate into actual behaviours. It would be valuable for experimental studies to investigate the role of attitudes towards ageing, age and care-giver status in behaviours that persons engage in when interacting with older persons with dementia.
Conclusion
Results from this study elucidated the role of age- and care-giver-related factors in attitudes towards dementia and personhood perceptions. This study demonstrated that more positive attitudes towards ageing and being a care-giver was predictive of being more comfortable around people with dementia, having more knowledge about dementia and ascribing higher personhood to those with dementia. Compared to younger adults, older adults were also found to be more comfortable around people with dementia. Furthermore, older adults with more dementia knowledge prior to the presentation of dementia information were more comfortable around those with dementia. Our findings allow for the identification of populations that are less comfortable being with people who have dementia, have less knowledge about dementia and who ascribe reduced personhood to them. As age did not play a role in attitudes towards dementia and personhood perceptions, attitudes towards ageing may be a better target for interventions. Our findings also indicate that increasing public awareness and knowledge about dementia should lead to improved attitudes towards dementia. Ultimately, a better understanding of the role of age- and care-giver-related factors in attitudes towards dementia and personhood perceptions could lead to interventions that could reduce the marginalisation of individuals with dementia living in our communities.
Author contributions
TH prepared the grant application that funded the study, played a major role in its conceptualisation, and guided and supervised every aspect of this investigation, including a major contribution to the write-up and interpretation of the results. CN assisted with the development of the data collection protocol, data collection, data analysis/interpretation, write-up and literature review. NLG played a major role in data analysis, interpretation and write-up. YCM played a major role in the data analysis and assisted with the write-up of the results. All authors discussed the results as well as read, edited and approved the final manuscript.
Financial support
This work was supported by an operating grant from the Saskatchewan Health Research Foundation.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
Approval for this study was granted by the University of Regina's Ethics Review Board.










