Chronic diseases are defined as conditions that last more than one year, require ongoing medical attention, and possibly limit daily activities (NCCDPHP 2020). Chronic diseases include a suite of illnesses that impact physical and mental health, such as arthritis, cancer, cardiovascular disease, chronic respiratory diseases, dementia, diabetes, inflammatory bowel diseases, fibromyalgia, mental illness, neurological conditions, and osteoporosis (Public Health Agency of Canada 2020).
This article focuses on three common chronic diseases—asthma, diabetes, and depression—and their relationship to archaeological fieldwork. Each section contains “best practice” recommendations for self-management for archaeologists working in the field with these conditions and for their group leaders and team members. Although many chronic conditions may have acute phases—or in some cases, even resolve fully—the purpose of this article is to address efforts to maintain these conditions beyond their acute phases. Aside from the three chronic diseases reviewed here, we encourage field directors to educate themselves about other diseases that their team members manage and to make appropriate preparations.
We chose these three because they are conditions that generally (1) do not severely limit or prevent fieldwork, (2) represent a range of physical and mental health conditions (which are often intertwined), (3) are variably visible, (4) involve differing levels of ease (and appropriateness) of disclosure, (5) can be triggered by the social and environmental factors involved in fieldwork, and—if not properly attended to—(6) can be life-threatening. Additionally, we have personally experienced the seriousness that these three chronic diseases have caused us or others during archaeological fieldwork (Supplemental Texts 1 and 2).
The following information is derived from medical literature. It is important to note, however, that we are not medical experts ourselves. If you have a chronic condition, please consult your physician and provide a thorough description of your field environment so as to design an individualized plan. If you are a field director, become educated on ways to be inclusive in how you structure the field environment (e.g., Phillips et al. Reference Phillips, Gilchrist, Hewitt, Le Scouiller, Booy and Cook2007), practice archaeology with compassion (e.g., New Ethnographer 2019), and become familiar with medical issues that may occur in the field and appropriate responses.
CHRONIC DISEASES AND ARCHAEOLOGY
Chronic diseases are prevalent. It is estimated that 6 in 10 adults in the United States have a chronic disease and that 4 in 10 adults have two or more (NCCDPHP 2020). Although the prevalence of these conditions among archaeologists has not been assessed directly, it is likely that these statistics carry over in a significant fashion to our profession.
Chronic diseases are often invisible to others until emergency situations arise (Joachim and Acorn Reference Joachim and Acorn2000). Even disclosure does not necessarily bring understanding, sensitivity, or accommodation of others to the social and physical demands of a chronic condition (Charmaz and Rosenfeld Reference Charmaz, Rosenfeld, Waskul and Vannini2006:43). Furthermore, with visibility may come stigmatization, and people with illnesses and disability often see reflections of their bodies and selves in the way others respond (Charmaz and Rosenfeld Reference Charmaz, Rosenfeld, Waskul and Vannini2006; Hoppe Reference Hoppe2010).
Chronic diseases impact everyday life, both in and out of the field. People with chronic illness deal with the stress of managing symptoms, ongoing treatment, the financial burden of medical care, and the emotional toll (e.g., loss of control, guilt, social isolation, self-definition by the disease, sense of ineffectiveness; Natale Reference Natale2019:13–20). Anthropology (and archaeology, in particular) often places a primacy on fieldwork, which is further wrapped in sexist connotations and ableism (e.g., “cowboy archaeology” and the need to “tough it out”; if one cannot perform x and y tasks, one is either not “cut out” to be an archaeologist or not a “true” archaeologist; Fitzpatrick Reference Fitzpatrick2019; New Ethnographer 2019; Vieth Reference Vieth2019). To previously published, powerful personal accounts on mental illness (e.g., Fitzpatrick Reference Fitzpatrick2018, Reference Fitzpatrick2019; Rocks-Macqueen Reference Rocks-Macqueen2016; Vieth Reference Vieth2019), we add how asthma and diabetes have impacted our career trajectories in archaeology (Supplemental Texts 1 and 2). We strongly encourage our readers, especially those without chronic diseases, to review these narratives because they lend perspective to the challenges faced by those with chronic diseases in our profession.
Finally, for those with chronic illnesses, archaeological fieldwork creates additional risk factors that can lead to medical emergencies, discussed below. Even if managed well, preexisting chronic medical conditions can cost comfort and productivity the field (Eifling and Klehm Reference Eifling and Klehm2020). What happens during fieldwork may have lasting impacts long after the season or project has been completed. Awareness of, and planning for, risk factors is an important complement to the creation of an accessible, inclusive field environment where team members feel free to disclose their conditions without being judged, where everyone is encouraged to monitor their health, and where all team members are supportive of prompt, sensible action.
ASTHMA
In the United States today, more than 25 million people (1 in 13 people) are affected by asthma, and more than 30 million Americans have experienced asthma in their lifetime (NACP 2020). Each year, more than 1.5 million U.S.-based emergency room visits and 439,000 hospitalizations occur due to asthma (Hsu et al. Reference Hsu, Sircar, Herman and Garbe2018). In the United States alone, asthma kills 4,000 people and is a factor in 7,000 additional deaths per year (NACP 2020).
Symptoms and Treatment
An asthma attack can progress through multiple stages if left untreated. First, the lining of the airways swells and becomes inflamed. Second, airways may become clogged with mucus, and muscles around the airways tighten. Third, damage to the ciliated lining cells in the lungs causes them to break away and accumulate as debris in the airway. All of these developments constrict the airway, making it difficult to breathe (NACP 2020). The National Institute of Health's National Heart, Lung, and Blood Institute (NHLBI 2007:6–7) gives more detailed clinical descriptions.
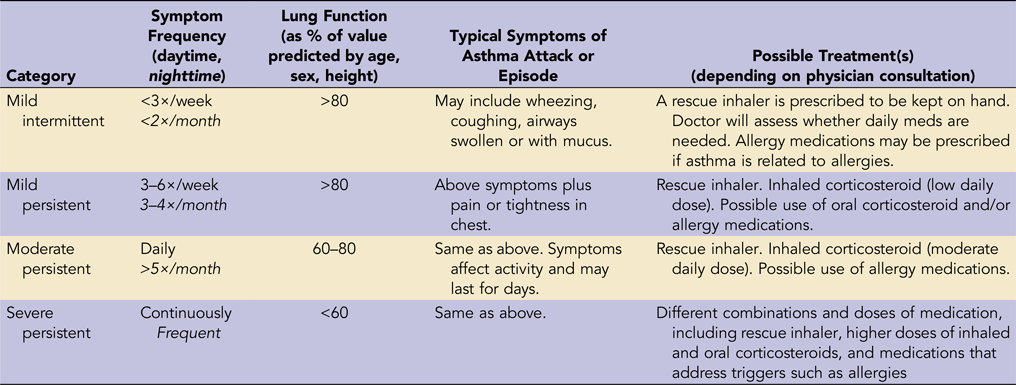
Asthma may be divided into four categories according to the severity and frequency of symptoms (Table 1), with different strategies for treatment. Some medications (e.g., inhaled or oral corticosteroid) aim to achieve long-term control by reducing inflammation and loosening muscles around the airway. These may be taken daily for extended periods (NHLBI 2007). Others are meant to provide fast relief during an acute episode (e.g., albuterol or other “rescue” inhalers). Asthmatics undertaking fieldwork may or may not be taking long-term medication, depending on their disease severity category. All asthmatics, however, should keep a rescue inhaler with them because acute episodes can occur at any time. Doses for rescue inhalers may vary depending on circumstances.
Table 1. Categories of Asthma and Associated Symptoms and Medications.

Source: Wells Reference Wells2019.
In many cases, an asthma attack may be momentarily resolved through prompt use of a rescue inhaler. Individuals experiencing more frequent or severe attacks during fieldwork should examine triggers and contingency treatment plans as outlined by their doctor in predeparture meetings (see below). If an attack is so severe that the asthmatic cannot speak, and the rescue inhaler does not result in rapid improvement, the asthmatic should be taken to the emergency room or an urgent care facility. There, treatments may include oral corticosteroids, bronchodilators such as ipratropium, oxygen, or in extreme cases, intubation and mechanical ventilation (Mayo Clinic 2020).
Prevention of Triggers during Fieldwork: A Team Effort
Asthma has multiple risk factors, proximate triggers, and escalating causes that can increase the severity of an episode. Occupation, for example, plays a role in one in six cases of adult-onset asthma (Hsu et al. Reference Hsu, Sircar, Herman and Garbe2018). Long-term risk factors include having a family or personal history of asthma or allergies; being overweight; smoking or experiencing regular secondhand smoke exposure; and spending time in areas with pollution, fumes, or occupational chemicals. Proximate triggers can include intense aerobic exercise (especially for people with mild, intermittent asthma) or exposure to long-standing or new allergens. Hormonal changes, or respiratory illnesses such as pneumonia or bronchitis, may escalate more manageable categories of asthma into severe, persistent asthma (Hsu et al. Reference Hsu, Sircar, Herman and Garbe2018; Wells Reference Wells2019).
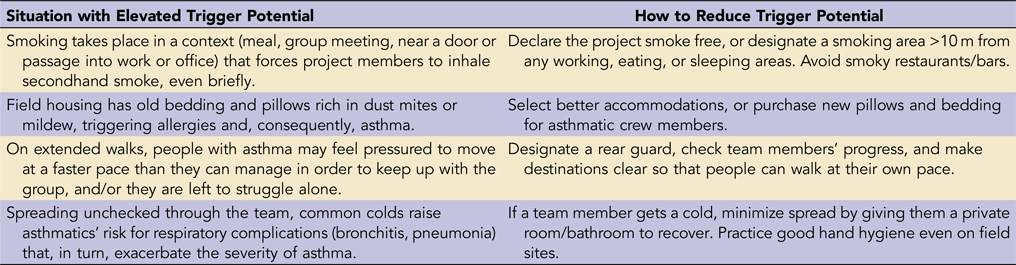
Many people with asthma have excellent working knowledge of how their condition manifests in regular, non-fieldwork life, and they follow routine safeguards and medication regimens to minimize the frequency and severity of symptoms. Nevertheless, all archaeologists (with or without a history of asthma) must recognize that field environments (both on-site and after-hours) may pose special risks for triggering or amplifying asthma. Minimizing this risk is part of the job of everyone on the project. Table 2 provides examples of common situations where decisions by project leaders or behavior of crew members might trigger an onset or escalation of symptoms. It also details simple changes that could reduce or eliminate those triggers.
Table 2. Field Archaeology Scenarios That May Trigger an Asthma Attack and Suggestions for Mitigating These Risk Factors.

Essentials for the Field-Bound Asthmatic: Self-Recognition, Preparation, and Monitoring
Recognizing that one is an asthmatic is the essential first step in preparing for field situations. Surprisingly, some asthmatics are reluctant to do so, particularly those who are typically in the “mild intermittent” category. Successful home regimens (e.g., using hypoallergenic bedding and HEPA filters, foregoing pets) can lead to complacency and an “I don't really have asthma” attitude. But one of us (EH) has known someone with very mild intermittent symptoms at home who experienced a sudden, dramatic, and life-threatening escalation in the field.
Preparing for fieldwork requires knowing one's baseline symptoms as well as considering typical and new potential triggers. Baseline knowledge of the frequency and severity of symptoms at home is essential for recognizing changes in condition during fieldwork. Peak flow meters (which cost around $14) are simple handheld, nonelectric devices that help track typical range of lung function over time. It is also good for asthmatics to keep a record of home episodes and likely triggers, as well as the treatments that they and/or medical professionals used in response.
If you have asthma, prior to a field project, you should review your home baseline for the previous year with your doctor. This can help you both anticipate scenarios and strategize appropriate responses (either in reducing the trigger or altering the medication regime to compensate). Your medical visit should not yield simply a set of refilled prescriptions for medications taken at home. It should also generate an “asthma action plan” (Nall Reference Nall2020) of preventative measures, known triggers, medicines, and contingency protocol. To provide for escalation scenarios, your doctor might instruct you on possible higher doses of medications you already use or give you additional prescriptions.
Before leaving for the field, you should also meet with the project director or another senior project member (if you are the director). Provide detailed information about your condition, the typical severity and frequency of symptoms, known triggers, and potential escalation, along with a streamlined version of your “action plan” (a second copy should be taped into your field notebook or first aid kit in case you become incapacitated). Together, review the action plan and explore triggers that could occur in the field, as well as ways to minimize their likelihood. Inquire about the availability of nearby emergency medical care.
After arriving in the field, assess potential triggers and mitigation strategies using on-the-ground knowledge. If necessary, bring problems to the attention of the director (or another senior staff member). Verify the accessibility of medical care, and make sure your medicines accompany you at all times, even if you don't expect to need them. Implement the medication regime your doctor recommended. Monitor lung function daily to establish new field baselines and track improvement or deterioration.
Project Director Essentials
If you are a director, listen carefully to the information provided by your asthmatic colleagues (above), and make sure you give them the time and discussion space to brief you as fully as they can before departure. Ask follow-up questions where appropriate. Together, identify and reduce potential triggers during work hours or nighttime. Work with them to plan for contingencies, including in-field medical treatment or emergency evacuation. Before departure—as part of general project guidance about health, safety, and ethics—communicate essential information to all team members so as to avoid unnecessary triggers. Soon after arrival in the field, check to see if any unanticipated triggers are present and work to reduce them. Create opportunities for your asthmatic colleagues to update you privately on their condition. Cultivate a team atmosphere of respect for people's medical needs and mutual assistance, and make sure team members are complying with health/safety/ethics protocols.
DIABETES
Diabetes is prevalent in the United States. Just over one-tenth of the population has diabetes, or 34.2 million people (CDC 2020). It is the seventh leading cause of death in the United States, and 1.5 million cases are diagnosed yearly (American Diabetes Association 2020). There are two types of diabetes—Type I and Type II. Type I diabetics do not produce insulin and must inject it. Type II diabetics have a combination of diminished insulin production in the pancreas and decreased sensitivity to insulin's effects. Consequently, they take pills to stimulate production, but they may also inject insulin. Diet and exercise help control both types.
Diabetics monitor their blood sugar levels to prevent complications, which may be short term (including diabetic coma, ketoacidosis), long term (such as blindness, kidney damage, and nerve damage), or even death. Diabetics strive to maintain their blood sugar level between 80 and 130 mg/dL before meals, and under 180 after meals (Campbell Reference Campbell2020), although this can vary by individual and is determined in consultation with a physician. Blood sugar is monitored using a glucometer, in which a drop of blood is obtained through a finger prick. Alternatively, blood sugar can be measured through a continuous glucose monitoring (CGM) sensor inserted into the skin. Readings are taken every five minutes and sent electronically to a system, usually part of an insulin pump (see below). Sensors, however, need to be calibrated with a glucometer and finger prick at least twice daily.
Type I and some Type II diabetics inject insulin through either the use of syringes or insulin pumps. In a general sense, insulin converts carbohydrates into energy for the body. Without insulin, glucose from carbohydrates builds up and eventually results in ketoacidosis and death. Insulin pumps administer insulin from a reservoir in the pump through tubing into a cannula inserted into the individual's subcutaneous fat layer, although pump delivery systems vary. The cannula, tubing, and reservoir are generally replaced every three days. If insulin pumps are also CGMs, some pumps can self-regulate and adjust insulin needs as blood sugar varies throughout the day. All pumps deliver insulin in two modes: basal and bolus. Basal modes inject rates of insulin throughout the day. Rates are set based on blood sugar patterns. For example, some diabetics experience the “dawn phenomenon,” where rising cortisol levels increase blood sugar in early morning hours, and pumps can be set to deliver more insulin at this time. Bolus insulin delivery is done when the individual eats food containing carbohydrates. They have a set insulin/carbohydrate ratio, so that, for example, every x number of carbohydrates they eat requires y number of units of insulin to be processed appropriately. Total insulin rates vary per individual, and they are determined by diet, weight, and personal insulin sensitivity. Glucometer and pump data can be downloaded on a regular basis so that patterns can be identified and adjustments made.
Diabetes impacts life both in and out of the field. Because diabetes can compromise the immune system, diabetics may have increased doctor visits and sick days, and they are more prone to infections. The cost of diabetes can be prohibitive, given that insulin pump supplies, pump sensors, test supplies, and insulin can cost hundreds of dollars per month in the United States with insurance, let alone without. Diabetics are also prone to higher rates of depression (discussed later this article).
Managing Diabetes in the Field
There are three primary areas of concern when considering diabetes in the field that both field directors and diabetics (if different) should be aware of: hypoglycemia (low blood sugar), hyperglycemia (high blood sugar), and weather extremes.
Hypoglycemia occurs when blood sugar drops below 70 mg/dL. This may be due to exercise, too much insulin, too little food, or a combination of these. Hot weather conditions also make hypoglycemia more likely for many individuals. If not treated, blood sugar continues to drop until the individual passes out, and death can occur. Symptoms of low blood sugar include dizziness, shaking, pallor, and slurred speech, but other symptoms can be specific to individuals or situations. It is a good idea to ask the diabetic what their particular signs of hypoglycemia are before fieldwork begins so that symptoms can be recognized promptly. Hypoglycemia can be quickly halted by ingesting a fast-acting form of glucose, such as regular (not diet) soda, juice, honey, or candy. Diabetics should carry fast-acting forms of sugar with them, such as juice boxes or glucose tablets. These can also be part of the field medical kit as a backup. If the individual is having difficulty swallowing, honey or candy in the mouth can be absorbed through the oral mucous membranes. If the individual loses consciousness, 911 or other local emergency medical service numbers should be called. In addition, a rapid-reversal agent called “glucagon,” a hormone that stimulates the liver to release glucose into the bloodstream, can be given as an injection (liquid) or a nasal spray (powder). Again, individuals should carry these items with them and instruct a member of the team about its location and use. Individuals with low blood sugar often need a few minutes to recover. Some individuals, in consultation with their physician, may need to eat a snack with fats and complex carbohydrates before returning to work.
Hyperglycemia, or high blood sugar, occurs when the blood sugar is over 250 mg/dL. In extreme cases, diabetics can enter a state of ketoacidosis, which can cause extreme thirst, frequent urination, vomiting, rapid heartbeat, and loss of consciousness. Hyperglycemia is caused by a lack of insulin, possibly due to blockage in a pump, a missed injection, or insufficient insulin for food needs. In addition, expired insulin or insulin that has been either frozen or overheated will lose its effectiveness. If an individual appears to be in ketoacidosis, give plenty of water, and call the appropriate local emergency number. A person may need a few hours to recover before returning to work, but this can vary.
As stated above, extreme heat makes low blood sugar more common for some diabetics. Cold weather can inhibit a glucometer's ability to work (and make finger pricking difficult). Heat can alter the effectiveness of insulin, so it needs to be kept cool. Heat can also affect the tape used to attach the cannula and sensor of a pump or CGM to the skin, which can result in these falling out—unbeknownst to the diabetic—and causing hyperglycemia. Special tape and skin glues can be used to avoid these problems.
Diabetics should travel with backup supplies, particularly if they are far from home, and they should consider storing them in a waterproof bag. Keeping injection areas and finger-prick sites clean is important in order to decrease the risk of infection, and it is especially critical and often difficult in the field. It is also good practice to wear a medic alert or a similar type of bracelet. That said, there is a line between the necessity of discussing the concerns and needs of diabetic employees and their right to privacy. As a director, you can urge all employees to discuss any health issues and needs with supervisors as soon as possible so as to ensure a smooth field season—or as a supervisor, with the crew.
Diabetes is not a barrier to archaeological fieldwork. Knowledge, preparation, and support can help ensure safe field experiences.
DEPRESSION
As of 2018, 17.3 million U.S. adults, or 7.1%, of the population have suffered from at least one depressive episode during the last 12 months, and this number is nearly doubled (13.1%) for those aged 18–25 (CBHSQ 2018). Depression is the largest contributor to nonfatal health loss around the world. It is often a taboo topic in archaeology, where it may be viewed as weakness that will lead to discrimination, stigmatization, or even unemployment (but see Fitzpatrick Reference Fitzpatrick2018, Reference Fitzpatrick2019; New Ethnographer 2019; Rocks-Macqueen Reference Rocks-Macqueen2016). Here, we wish to emphasize the population at risk in order to recommend how to prepare for, identify, and manage depression in the field. The topic of mental health is also covered in greater depth in Eifling (Reference Eifling2021a).
Depressive disorders are among the suite of mental health disorders that impact mood, thoughts, and behavior and causes significant interruption in everyday activities (American Psychiatric Association 2013; McGladrey and Campisi Reference McGladrey, Campisi and Hawkins2018:413–414). Depressive disorders are common, occurring in 7.6% of the population in the United States over the age of 12, and in 4.4% of the global population (CBHSQ 2018; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators 2018). Women are one-and-a-half to three times as likely to experience depression, beginning in adolescence. As is the case with the related affliction of anxiety, depression is more likely among those with genetic vulnerability, early childhood trauma, current life stressors, and certain belief structures. Current life stressors are particularly relevant for archaeologists, given that work stress may be exacerbated by office (or out-of-field) environments as well as personal life circumstances. Depression is a common comorbidity to other chronic diseases (Clark and Currie Reference Clarke and Currie2009) as well as sexual harassment and assault—prominent issues in archaeological fieldwork (e.g., Meyers et al. Reference Meyers, Horton, Boudreaux, Carmody, Wright and Dekle2018; VanDerwarker et al. Reference VanDerwarker, Brown, Gonzalez and Radde2018) that also may contribute to depression.
Risk Factors for Depression
Archaeologists, whether in academia or cultural resource management, carry significant risk for anxiety and depression. Academic work is often poorly compensated, rarely sticks to 40 hours per week, and smuggles emotional labor within the tacit expectation to work longer hours and to publish more, along with a fear of falling “behind” (Tucker and Horton [Reference Tucker and Horton2018] for summary). One-third of graduate students are at risk of having or developing a mental health condition (Levecque et al. Reference Levecque, Anseel, De Beuckelaer, Van der Heyden and Gisle2017). In both the academic and cultural resource management worlds, archaeologists may regularly experience unemployment, underemployment, poverty, frequently changing schedules, and labor-intensive work that may lead to or exacerbate injuries and chronic pain. Active smoking and drinking cultures within archaeology share comorbidity with depression.
Extended travel heightens the risk of developing or deepening depressive episodes (Valk Reference Valk, Keystone, Kozarsky, Connor, Nothdurft, Mendelson and Leder2019). Fieldwork in other countries introduces aggravators such as culture shock, foreign language, varying cultural approaches to mental illness, variable treatments that may or may not be compatible with a patient's prescription, and minimal or a complete absence of medical infrastructure to obtain psychotropic medications or professional help in-country. Travel insurance does not always cover psychiatric illness, which may skyrocket treatment costs, especially if medical evacuation is required. Fieldwork can contribute to travel anxiety in multiple and often layered ways: being away from home, supportive friends and family, and professional health support; being in a challenging physical and/or social environment; living communally, in unfamiliar territory; experiencing eating and sleeping arrangements that may lead to poor nutrition, poor sleep, and a lack of privacy; completing tasks in groups; and being asked to divulge personal responses (Birnie and Grant Reference Birnie and Grant2001; Tucker and Horton Reference Tucker and Horton2018).
Depression in the Field: Preparation, Prevention, Recognition, and Management
Before travel, individuals dealing with depression should consult with a travel medicine specialist, and potentially a psychiatrist who is familiar with international travel risks (Valk Reference Valk, Keystone, Kozarsky, Connor, Nothdurft, Mendelson and Leder2019:465). Those with recurring major depressive episodes that have not been stabilized on medication should recognize that they may be at higher risk. They should work with medical professionals before fieldwork to evaluate the severity of illness, the long-term stability of treatment, and the availability of psychiatric resources and medications that they may need. Even those who are stable may need to adjust lithium dosing for exercise, diet, and hydration changes. Along similar lines, the antimalarial mefloquine (which used to be routinely prescribed but now carries a black box warning from the United States Food and Drug Administration) can induce psychotropic effects in fieldworkers who are stable or have no history of depression (US-FDA 2013). Those with a history of depression should consider other antimalarials.
Alcohol and substance abuse at home can lead to withdrawal in the field. Also, fieldworkers who are in recovery from alcohol/substance abuse may find fieldwork challenging due to the absence of recovery support networks. If you suspect a substance abuse disorder that will be disruptive during the field season, consider referring your peers to Substance Abuse and Mental Health Services Administration's free, 24/7 hotline (1-800-662-4357), which provides referrals to local treatment facilities, support groups, and community-based organizations in the United States.
Archaeological field directors can work toward creating a more relaxing and affirmative field season by allowing the crew to identify good/bad days for participation without fear of resentment, enabling full integration of the crew into social aspects (if social contact is beneficial), and encouraging a buddy system of disclosure (see Phillips et al. Reference Phillips, Gilchrist, Hewitt, Le Scouiller, Booy and Cook2007:29). Student-to-student or peer-to-peer monitoring has proven to be especially effective as a way to assess mental health. Days off from fieldwork can be particularly resetting for a field crew.
Foreknowledge of risk factors and recognition of symptoms (see below) are also important. Depending on university or company regulations, medical screening and disclosures can help assess the level of risk among field participants. Self-disclosure might not be allowed in all contexts, and when it is, directors should consider reciprocal measures of confidentiality and statements of where and how that information will be used. Due to systemic ableism, many archaeologists with mental health disabilities may make the reasonable choice of not disclosing their diagnoses. Field directors should not expect or press for disclosures of diagnoses of mental health disabilities from colleagues. Although field directors may have procedures for storing and taking medications, they should permit archaeologists with mental health conditions to manage their own medications in order to protect their privacy.
Field directors and field participants alike should look for physical manifestations of depression in themselves and others. Depression can range from subtle changes in energy of the individual to total disruption of behavior and/or suicidal ideation (McGladrey and Campisi Reference McGladrey, Campisi and Hawkins2018:413). People's reactions to depression manifest through a variety of emotions: shame, frustration, betrayal, embarrassment, desperation, and feeling unsupported, among others (Pollard Reference Pollard2009). Weight loss or gain may be difficult to see with daily exposure, but other symptoms may be more visible. These include decreased energy, sleep disturbance, isolation, fatigue, rumination, worry, anxiety, and decreased ability to concentrate, complete tasks, and/or make decisions (McGladrey and Campisi Reference McGladrey, Campisi and Hawkins2018:418). Increased drinking is often a sign of depression.
In the field, all levels of care should be provided, including recognition that depression is the issue, both by the field member and the appropriate supervisor; provision of support and validation (i.e., connection with the patient); and forthright questioning with regard to suicidal ideations (McGladrey and Campisi Reference McGladrey, Campisi and Hawkins2018:419; see also Eifling Reference Eifling2021a). If an individual engages in self-harm, staff should evaluate and treat immediate wounds and/or bring that individual to a medical professional or emergency department, as is appropriate given the severity and field settings.
Unfortunately, there are no fast-acting medications or universal preventative measures for eliminating depression. However, preparation by both field directors and participants, recognition of symptoms, and proactive efforts to build an inclusive field environment can help mitigate the incidence in the field.
CONCLUSION
Accommodating and welcoming colleagues with chronic diseases into the profession and in fieldwork is a vital part of archaeology's pursuit to become more diverse and inclusive. It is the responsibility of archaeological projects to be accessible to all participants. Following Phillips and colleagues (Reference Phillips, Gilchrist, Hewitt, Le Scouiller, Booy and Cook2007:17–19), an attitude of acceptance, awareness of limitations and potential and emerging issues, responsiveness, and flexibility are foundational to creating successful, enjoyable, and safe field seasons for those with chronic conditions.
We stress the importance of this often overlooked, significant, even life-threatening topic of chronic illnesses, especially in the context of fieldwork, which introduces novel situations and other challenges for management. Many of these problems can be anticipated, prepared for, and mitigated with adequate knowledge. Further resources on mental health (Eifling Reference Eifling2021a), disability and archaeology (Fraser Reference Fraser2008; O'Mahony Reference O'Mahony2015; Phillips et al. Reference Phillips, Gilchrist, Hewitt, Le Scouiller, Booy and Cook2007), sexual harassment and assault (Colaninno et al. Reference Colaninno, Lambert, Beahm and Drexler2020; Nelson et al. Reference Nelson, Rutherford, Hinde and Clancy2017), building a safe and inclusive culture in archaeology (New Ethnographer 2019; Peixotto et al. Reference Peixotto, Klehm and Eifling2021; Phillips and Gilchrist Reference Phillips, Gilchrist, Skeates, McDavid and Carman2012; Phillips et al. Reference Phillips, Gilchrist, Hewitt, Le Scouiller, Booy and Cook2007), and medical emergency and safety preparedness (Davis et al. Reference Davis, Meehan, Klehm, Kurnick and Cameron2021; Eifling Reference Eifling2021b; Emerson Reference Emerson2021; Hawkins and Simon Reference Hawkins and Simon2021; Hawkins and Winstead Reference Hawkins and Winstead2021; Meyers et al. Reference Meyers, Breetzke and Holt2021; White Reference White2021) may also be of use.
Acknowledgments
The authors wish to acknowledge the 2019 SAA forum titled “Medical Needs of Archaeological Field Camps: Improving Readiness and Response,” which is the event that brought the three of us together to discuss this often overlooked topic. We would like to thank those colleagues and students who have helped us “make visible” these issues through our own field experiences, and we thank those who have supported us and others. We also thank our peer reviewers and the editors of Advances in Archaeological Practice for their support and advice on this important topic. No permit was required for this research.
Data Availability Statement
No original data were presented in this article.
Supplemental Materials
For supplemental material accompanying this article, visit https://doi.org/10.1017/aap.2020.49.
Supplemental Text 1. Author essay: a career in archaeology with diabetes.
Supplemental Text 2. Author essay: a career in archaeology with asthma.