Significant outcome
-
Non-volunteer soldiers presented impairment in both mood and health-related quality of life.
Limitations
The results depend on the volunteers’ honesty in responding to the instrument and their level of recall.
The participants were not submitted to a clinical diagnosis of depression and anxiety.
We did not evaluate their physiological parameters.
Introduction
Mental and behavioural disorders, including affective disorders, are medical conditions prevalent in modern society that afflict more than 650 million people around the world. (WHO, 2013) Anxiety and depression feature amongst the major disorders. Current predictions indicate that, by 2030, depression will be the leading cause of disease burden globally. Mental disorders account for 25.3% and 33.5% of years lived with a disability in low- and middle-income countries, respectively (WHO, 2011).
Depression and anxiety are multi factorial diseases that are more common among people of low socioeconomic (SE) status, low education level, unmarried, separated or divorced, from rural backgrounds and without intact families. (Browne et al., Reference Browne, Mora, Alonso, Levinson, Iwata, Andrade, Posada-Villa, Kostyuchenko, Hwang, Demyttenaere, Lépine, Bromet, Kaur, Williams, Viana, Karam, de Girolamo, Matschinger, de Graaf, Sampson, Kessler and Hu2011) It is also noteworthy that a higher prevalence of depression and anxiety may occur in clinical conditions and specific populations, such as in patients with epilepsy, (de Lima et al., Reference de Lima, de Lira, Arida, Andersen, Matos, de Figueiredo Ferreira Guilhoto, Yacubian, de Albuquerque, Tufik, dos Santos Andrade and Vancini2013; Vancini et al., Reference Vancini, de Lira, Andrade, Lima and Arida2015) cancer (Härter et al., Reference Härter, Baumeister, Reuter, Jacobi, Höfler, Bengel and Wittchen2007; Dalton et al., Reference Dalton, Laursen, Ross, Mortensen and Johansen2009) or diabetes (Härter et al., Reference Härter, Baumeister, Reuter, Jacobi, Höfler, Bengel and Wittchen2007) and in college students (Zivin et al., Reference Zivin, Eisenberg, Gollust and Golberstein2009; Mahmoud et al., Reference Mahmoud, Staten, Hall and Lennie2012; Ibrahim et al., Reference Ibrahim, Kelly, Adams and Glazebrook2013).
Particularly for the purpose of the present study, young soldiers were exposed to high physical and psychological demands during military service and it is reasonable to assume that they are potential candidates for developing mood disorders. Bachynski et al. (Reference Bachynski, Canham-Chervak, Black, Dada, Millikan and Jone2012) showed that suicidal deaths were 11 times more likely in soldiers with depression and 10 times more likely in soldiers with anxiety disorders, including post-traumatic stress disorders. Depression and anxiety among military personnel have received relatively little attention compared to other populations, despite being of great importance.
On a worldwide scale, 83 countries have mandatory enlistment in military service. (Leal, Reference Leal2008) In Brazil, every year 1.7 million individuals are enlisted in military service and 50–70 thousand are selected to meet mandatory military service. (Leal, Reference Leal2008) As those recruited include individuals who have no interest in following military service, the situation can induce high psychological demands that are linked to city and routine change, interruption of professional and/or academic career and distance from family. These personal situations are also associated with certain characteristics of military service, such as the hard disciplinary and hierarchical regime, which can predispose participants to develop mood disorders and lower levels of health status and quality of life. However, to the best of our knowledge, no studies have investigated the effects of mandatory military service on mood disorders and health-related quality of life.
Aims of the study
The present study’s primary aim was to describe the prevalence of mood disorders in a sample of Brazilian soldiers. A secondary aim was to compare the levels of mood disorders and health-related quality of life among volunteer group (VG) and non-volunteer group (NVG) of soldiers. We hypothesised that the NVG would present higher levels of mood disorders and poorer health-related quality of life than the VG.
Methods
Participants
A total of 353 male soldiers (age and anthropometric characteristics are displayed in Table 1) from the 41st Motorized Infantry Battalion (Jataí, Goiás, Brazil) agreed to participate in this study. They were assigned to one of two groups according to their personal desire to pursue military service: the 246 who volunteered and the 107 who did not volunteer for military service were assigned to a VG and NVG, respectively. Of these participants, 120 (46.9%) from the VG and 42 (39.3%) from the NVG did not reside in their city’s family. All the participants were supposedly healthy, had no neurological impairments and were using neither medications nor ergogenic aids known to influence neurological function/status and/or mood status. Each participant signed an informed consent form before the outset of the study. All the protocols were approved by the Federal University of Goias Human Research Ethics Committee and were in accordance with the Declaration of Helsinki’s ethical standards.
Table 1. Age and anthropometric characteristics of the volunteer group (VG) and non-volunteer group (NVG) soldiers

Data are means ± SD.
Study design
Participants from both groups completed the following questionnaires: (1) Beck Depression Inventory (BDI) to evaluate depression symptoms; (2) State-Trait Anxiety Inventory (STAI) to assess anxiety symptoms, (3) Profile of Mood States (POMS) to yield a global measure of mood, (4) medical outcomes study SF-36 questionnaire to assess the level of health-related quality of life, (5) Baecke questionnaire to assess the level of habitual physical activity (HPA) and (6) SE status questionnaire. Each of the participants, who were recruited at the beginning of mandatory service, answered all these questionnaires in random order on the same day.
Beck Depression Inventory (BDI)
The BDI (Beck et al., Reference Beck, Ward, Mendelson, Mock and Erbaugh1961) is a widely used 21-item self-reported scale, well validated and developed to measure the severity of depression. The questionnaire, translated and validated for Brazilian Portuguese, (Gorenstein & Andrade, Reference Gorenstein and Andrade1996) consists of statements divided into 13 categories that assess the individual’s emotional state. The inventory items assess attitudes and symptoms such as sadness, pessimism, sense of failure, lack of satisfaction, feelings of guilt and punishment, among others. Each question has scores ranging from 1 to 4. This study considered a BDI score of 0–9 as normal, 10–15 as mild depression, 16–19 as mild to moderate depression, 20–29 as moderate to severe depression and 30–63 as severe depression. The BDI’s internal consistency is good, with Cronbach’s alpha of around 0.9 (Storch et al., Reference Storch, Roberti and Roth2004; Gomes-Oliveira et al., Reference Gomes-Oliveira, Gorenstein, Neto, Andrade and Wang2012; Wang & Gorenstein, Reference Wang and Gorenstein2013).
State-Trait Anxiety Inventory
The STAI, (Spielberger et al., Reference Spielberger, Gorsuch and Lushene1970) translated and validated for Brazilian Portuguese, (Biaggio et al., Reference Biaggio, Natalício and Spielberger1977) is a 40-item self-reported assessment scale made up of two 20-item anxiety subscales: state anxiety (A-state) and trait anxiety (A-trait). The A-state scale describes an individual’s feelings at a particular time and under particular conditions, whereas the A-trait scale describes an individual’s usual feelings. Each STAI item is given a score of 1–4. A rating of 4 indicates the presence of high levels of anxiety for some items, and the scoring weights for the anxiety-absent items are reversed. Scores for both the A-state and A-trait scales can vary from a minimum of 20 to a maximum of 80: scores of more than 30 indicate the presence of anxiety; 31–49, an intermediate level of anxiety and greater than or equal to 50, a higher degree of anxiety. (Spielberger et al., Reference Spielberger, Gorsuch and Lushene1970) The internal consistency of both subscales is good, with Cronbach’s alpha of 0.93 and 0.87, respectively (Knight et al., Reference Knight, Waal-Manning and Spears1983).
Profile of Mood State
The mood profile was assessed by the POMS questionnaire, (McNair et al., Reference McNair, Lorr and Droppleman1971) translated and validated for Brazilian Portuguese. (Peluso, Reference Peluso2003) This is a self-reported questionnaire consisting of 65 items that fit into six categories: tension–anxiety, depression, anger–hostility, vigour, fatigue and confusion. Scoring is from 1 to 4, according to severity. (McNair et al., Reference McNair, Lorr and Droppleman1971) The questionnaire yields a global measure of mood. The global score is computed by subtracting the positive category (vigour) from the sum of the five negative categories (tension, depression, anger, fatigue and confusion). This study used the standard instructional set of the POMS questionnaire (McNair et al., Reference McNair, Lorr and Droppleman1971) because of its reliability, validity, feasibility and common use in psychometric studies. (Morgan et al., Reference Morgan, Costill, Flynn, Raglin and O’Connor1988) Its internal consistency is good, with a Cronbach’s alpha of 0.90 (Morfeld et al., Reference Morfeld, Petersen, Krüger-Bödeker, von Mackensen and Bullinger2007).
Medical outcomes study SF-36 questionnaire
The SF-36 Health Survey is a multidimensional questionnaire that contains 36 items covering eight health domains: physical functioning; role limitations due to physical health problems; bodily pain; general health; vitality; social functioning; role limitations due to emotional problems and mental health. The scores lie in the range 0–100, with a higher score indicating better health-related quality of life. (Ware et al., Reference Ware, Kosinski and Keller1994) The SF-36 questionnaire, translated and validated for Brazilian Portuguese, (Ciconelli et al., Reference Ciconelli, Ferraz, Santos, Meinão and Quaresma1999) has good internal consistency with a Cronbach’s alpha of 0.76–0.90 for all its subscales (Jenkinson et al., Reference Jenkinson, Wright and Coulter1994).
Habitual physical activity assessment
The HPA evaluated by the Baecke questionnaire (Baecke et al., Reference Baecke, Burema and Frijters1982) was validated and translated for Brazilian Portuguese. (Florindo et al., Reference Florindo, Dias de Oliveira Latorre, Constante Jaime, Tanaka and de Freitas Zerbini2004) This questionnaire involves three HPA scores relating to the previous 12 months and consists of 16 questions: eight questions on occupational physical activity (OPA) and four questions each on physical activity in leisure time (PAL) and sport physical activity (SPA). The total score for HPA was obtained by summing the OPA, PAL and SPA scores. The higher the score achieved, the higher the level of HPA. Cronbach’s alpha for OPA, PAL and SPA is 0.52, 0.52 and 0.62, respectively (Florindo et al., Reference Florindo, Dias de Oliveira Latorre, Constante Jaime, Tanaka and de Freitas Zerbini2004).
Socioeconomic assessment
The SE profile was assessed using an instrument that determines the social classification of individuals. (ABEP, 2008) This instrument is specific for the Brazilian population and considers the head of the household’s education level and the number of items in the home, such as refrigerators, automobiles, televisions, etc. The questionnaire assigned scores of 0–46 points and, based on the scores obtained, participants were grouped into the following classes: A1 (score 42–46), A2 (score 35–41), B1 (score 29–34), B2 (score 23–28), C1 (score 18–22), C2 (score 14–17), D (score 8–13) and E (score 0–7). The higher scores indicate a higher SE level.
Statistical analysis
The variables analysed were not normally distributed according to the Kolmogorov–Smirnov test, hence the data were expressed as medians (quartiles 1 and 3);the Mann–Whitney U-test was used to compare variables between the groups (VG vs. NVG) and the chi-square test of independence was used to find associations between the groups (VG vs. NVG).Using the Graph Pad Prism (version 5.0, San Diego, USA),the level of significance adopted in all the statistical analyses was 5%, with a 95% confidence interval.
Results
In total, 118 (33.5%) individuals did not present depressive symptoms, 127 (36.0%) had mild depressive symptoms, 45 (12.7%) had mild to moderate depressive symptoms, 59 (16.9%) had moderate to severe depressive symptoms and 4 (1.1%) had severe depressive symptoms. When categorised into VG and NVG, respectively, the scores were: 97 (39.5%) and 21 (19.7%) individuals did not show symptoms, 82 (33.3%) and 45 (42%) showed mild symptoms, 30 (12.2%) and 15 (14%) showed mild to moderate symptoms, 35 (14.2%) and 24 (22.4%) showed moderate to severe symptoms and 2 (0.8%) and 2 (1.9%) showed severe symptoms. The chi-square test of independence showed a significant association between groups and the level of depressive symptoms [χ2(4) = 14.256; p = 0.007].
The total prevalence of the A-state was based on the scores of this questionnaire. In total, 15 (4.2%) showed low levels of anxiety, 240 (68%) showed intermediate levels and 98 (27.8%) showed high levels of symptoms. When categorising into VG and NVG, respectively, the A-state scores revealed that 14 (5.7%) and 1 (0.9) had low levels of anxious symptoms, 189 (77%) and 51 (47.6%) had intermediate levels and 43 (17.3%) and 55 (51.5%) had high levels of anxious symptoms. The chi-square test of independence showed a significant association between groups and the level of A-state symptoms [χ2(2) = 44.207; p < 0.001].
Concerning the A-trait, 55 (15.6%) presented low levels of anxious symptoms, 268 (76%) showed intermediate levels and 30 (8.4%) showed high levels of anxious symptoms. The scores when divided into VG and NVG were as follows: 47 (19.1%) and 8 (7.5%) showed the presence of symptoms, 188 (76.4%) and 80 (74.7%) showed intermediate levels and 11 (4.5%) and 19 (17.8%) showed high levels of symptoms. The chi-square test of independence showed a significant association between groups and the levels of A-trait symptoms [χ2(2) = 136.064; p < 0.001].
The BDI score for the NVG [13 (10–19)] was significantly higher (Δ% = +25%, U = 10660, p = 0.0045) than that for the VG [11 (8–16)]. Furthermore, higher A-state scores (Δ% = +17%, U = 7563, p < 0.0001) were observed for the NVG [48 (43–55)] than the VG [40 (35–47.25)]. The A-trait scores were also higher (Δ% = +11%, U = 9747, p = 0.0001) in the NVG [40 (35–44)] than the VG [36 (32–42)].
The HPA between groups did not present any statistical difference (p = 0.2743). Regarding SE status, individuals of the VG and NVG belonged to the B2 level (24 ± 6 and 25 ± 6, respectively) and no statistical difference was found (p = 0.64) (Table 2).
Table 2. Scores for depression, anxiety, habitual physical activity and socioeconomic (SE) level in the volunteer group (VG) and non-volunteer group (NVG) soldiers

Data are medians (quartiles 1–3). *Statistically significant difference in relation to the VG (Mann–Whitney U-test). BDI, Beck Depression Inventory; STAI, State-Trait Anxiety Inventory; A-state, state anxiety; A-trait, trait anxiety; HPA, habitual physical activity.
All domains of the POMS showed statistical differences between the VG and the NVG, respectively: tension, 5 (2–8) and 7 (3–12), p = 0.0005; depression, 4 (1–8) and 6 (2–12, p = 0.001; anger, 5 (2–9) and 7 (3–13), p = 0.0007; vigour,18 (14–21) and 16 (12–20), p = 0.0154; fatigue, 4 (2–7) and 6 (3–11), p < 0.0001; confusion, 1 (−1 to 4) and 2 (0–5),p = 0.0247 and total mood disorders, 2 (−10 to 18.25) and 14 (−2 to 37), p < 0.0001. The scores were also higher (Δ% = +263%, U = 9419, p < 0.0001) in the NVG (21 ± 32) compared to the VG (6 ± 21) (Table 3).
Table 3. Scores for the domains of the Profile Mood State (POMS) in the volunteer group (VG) and non-volunteer group (NVG) soldiers
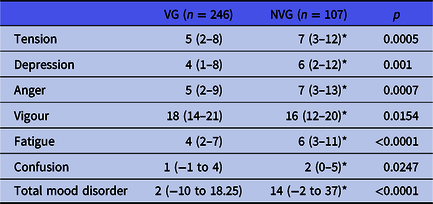
Data are medians (quartiles 1–3). *Statistically significant difference in relation to the VG (Mann–Whitney U-test).
Five of the eight subscales of the SF-36 showed statistical differences for VG and NVG, respectively: functioning capacity, 95 (85–100) and 90 (80–95), p = 0.0046; role limitations due to physical problems, 100 (75–100) and 100 (75–100), p = 0.3252; pain, 72 (61–84) and 62 (51–84), p = 0.0011; general health perceptions, 81 (67–92) and 77 (62–92), p = 0.1448 and social functioning, 87.5 (62.5–100) and 87.5 (50–100), p = 0.0613. However, the other three subscales showed no statistical differences: vitality, 75 (65–85) and 60 (45–75), p < 0.0001; role limitations due to emotional problems, 100 (66.67–100) and 100 (33.33–100), p < 0.0001 and mental health, 80 (68–92) and 68 (48–84), p < 0.0001 (Table 4).
Table 4. Scores from the domains of the SF-36 in the volunteer group (VG) and non-volunteer group (NVG) soldiers

Data are medians (quartiles 1–3). SF-36: short form survey. *Statistically significant difference in relation to the VG (Mann–Whitney U-test).
Discussion
The aims of this study were to: (i) describe the prevalence of mood disorders in a sample of Brazilian soldiers; (ii) compare the levels of mood disorders and health-related quality of life in volunteer and non-volunteer soldiers; (iii) compare the level of HPA between the groups and (iv) compare the SE level between groups. The main findings were that non-volunteer soldiers presented impairment in mood and health-related quality of life.
According to the BDI data for both groups, 66.5% of the soldiers showed at least mild depressive symptoms. Additionally, according to the STAI data, 27.8% and 8.4% of the soldiers showed high A-state and A-trait scores, respectively. These results are a cause for concern because the prevalence is above that found in general (Mahmoud et al., Reference Mahmoud, Staten, Hall and Lennie2012) and clinic conditions. (Naicker et al., Reference Naicker, Johnson, Skogen, Manuel, Øverland, Sivertsen and Colman2017; Vidigal-Lopes et al., Reference Vidigal-Lopes, Prado, Prado, Bicalho, Souza, Gomez and Teixeira2017) According to the World Health Organization (WHO) in 2015, 4.4% of the world’s population had depression and 3.6% had anxiety (WHO, 2017). Specifically, in relation to the Brazilian population, the WHO estimates that the prevalence of depression and anxiety is 5.8% and 9.3%, respectively (WHO, 2017). The results found by the current study are probably due to the elevated physical and psychological pressures inherent in military service.
The transition to adulthood, spanning late adolescence to the mid-20s, is marked by high rates of major depression (Kessler et al., Reference Kessler, McGonagle, Zhao, Nelson, Hughes, Eshleman, Wittchen and Kendler1994; Reinherz et al., Reference Reinherz, Paradis, Giaconia, Stashwick and Fitzmaurice2003) as individuals acquire more responsibilities, have to make professional choices, become more autonomous, move away from their families, have to unravel their own problems and face major identity crises. All these changes in a short period of time make this segment of the population potential candidates for developing mood disorders. One of the factors cited by the literature that causes the development of mood disorders in adolescents/students is any alteration in family relationships. (Ibrahim et al., Reference Ibrahim, Kelly, Adams and Glazebrook2013) In our sample, 120 (46.9%) participants in the VG and 42 (39.3%) in the NVG did not reside in city’s family. Taken together, these are reasonable explanations for our results.
As a consequence of the poor results in the BDI, STAI and POMS, health-related quality of life in the NVG was also lower. Soldiers are subjected to conditions such as high psychological pressure, intense exercise and lack of sleep, which can adversely affect their health-related quality of life and/or trigger psychological disturbances, (Minayo et al., Reference Minayo, Assis and Oliveira2011; Vancini et al., Reference Vancini, de Lira, Anceschi, Rosa, Lima-Leopoldo, Leopoldo, Rufo-Tavares, Andrade, Nikolaidis, Rosemann and Knechtle2018) particularly in those who did not volunteer for military service.
This study also evaluated the participants’ HPA and SE class but found no statistical difference between the groups. Hence, the difference in mood disorders and health-related quality of life between groups cannot be attributed to any difference in HPA and SE class. These results sustained our hypothesis that mandatory military service can cause extremely accentuated psychological demands, mostly on individuals in the NVG. As the military environment is characterised by a rigid disciplinary structure due to its hierarchy, these conditions might have been the cause of the elevated levels of mood disorders found.
Several limitations of this study must be noted. As in all studies using questionnaires, the results depend on the volunteers’ honesty in responding to the instrument and their level of recall. Furthermore, the participants were not submitted to a clinical diagnosis of depression and anxiety. In addition, we did not evaluate their physiological parameters.
To summarize, we found a high prevalence of mood disorders in Brazilian soldiers, especially among those who did not volunteer for mandatory military service. Furthermore, mood disorder levels were higher and health-related quality of life was lower in non-volunteers compared to those who had volunteered. Considering the signs and symptoms of anxiety and depression and their economic and social burden, it would be desirable for the military services to recruit only individuals who wish to follow a military career. Finally, it is desirable that the armed forces provide soldiers with psychological support.
Acknowledgements
We would like to thank all the participants who volunteered for this study. We are also grateful to the commander of the 41st Motorized Infantry Battalion (Jataí, Goiás, Brazil).
Author contributions
C.A.B.L., T.M. and A.G.B. designed the study, C.A.B.L., T.M., A.G.B., N.S.M. and V.A.M. collected the data, C.A.B.L., M.S.A. and N.S.M. performed the statistical analysis and R.L.V. contributed meaningfully to the intellectual content of this paper. All authors agreed upon the final version of the paper.
Financial support
This study was supported by the Fundação de Amparo à Pesquisa do Estado de Goiás (FAPEG, Brazil; grant number 201200547780809).
Conflict of interest
The authors declare that there are no competing interests.







