Summations
In light of our results, we confirm that ADHD can be persistent into adulthood with high frequency and can predispose to the development of other psychiatric disorders or social maladjustment with detrimental consequences for quality of life in adulthood.
The high prevalence of antisocial behavior and/or criminality activities observed in adult ADHD suggests that antisocial personality disorder and criminal activities can be the evolution of childhood oppositional and impulsive behavior.
Anxiety and depressive disorders are the most frequent psychiatric disorders associated with ADHD in adulthood. Alcohol and cannabis use are the most frequent complications of adult persistent ADHD.
Considerations
The instability of ADHD diagnosis over time, much increased by cultural changes and scientific measures over a period of 35 years, may have conditioned the rate of adulthood persistence.
The lack of many data regarding specific population categories and outcomes limits the generalizability of our observations. Further prospective studies in different populations with differentiated outcomes need to confirm these results.
The high rate of persistent ADHD suggests that this condition may not just be a neurodevelopmental disorder, but more clinical trials are needed to properly diagnose and treat this “new disorder” in adulthood.
In this review, after an introduction concerning ADHD clinical issues, we evaluated the ADHD persistence in adulthood and the comorbidity occurrence of psychiatric disorders, substance/alcohol use and antisocial personality or criminal activities with conviction, and/or jail among individuals with ADHD diagnosis in childhood. Our review included the description of research strategies as well as methods, results, and conclusions of each study. After a qualitative and quantitative analysis of data collected from the studies included, the clinical relevance of ADHD and comorbid disorders and/or altered behavior in adulthood were discussed. Following a summary of findings, strengths, and limitations of this review, we highlighted the clinical issues related to ADHD and hypotheses for future research.
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a neuro-developmental disorder characterised by disability symptoms of inattention and/or hyperactivity–impulsivity, generally beginning by school age, causing impairment in more than one cognitive and functional dimension. The term ADHD was adopted by DSM-III-R and has been widely and steadily used since (American Psychiatric Association [APA], 1987). The DSM-IV added other presentations: predominantly hyperactive, predominantly inattentive, and combined (Lange et al., Reference Lange, Reichl, Lange, Tucha and Tucha2010). In the latest edition of DSM-5, an additional presentation, inattentive–restrictive with minimal hyperactive symptoms, was added (American Psychiatric Association [APA], 2013). ICD-10 requires both inattentive and hyperactive/impulsive symptoms for the diagnosis of ADHD, excluding children with co-occurring conduct disorders (World Health Organization [WHO], 1992). For this latter category, a combined diagnosis of hyperkinetic disorders and conduct disorder is provided, indicating the high prevalence of this association as well as its linkage with ADHD progression.
The ADHD prevalence ranges between 5% and 7% (Polanczyk et al., Reference Polanczyk, Willcutt, Salum, Kieling and Rohde2014; Thomas et al., Reference Thomas, Sanders, Doust, Beller and Glasziou2015) in childhood/adolescence, whereas the prevalence in adulthood is esteemed between 2.5% and 4% in adults (American Psychiatric Association [APA], 2013; Fayyad et al., Reference Fayyad, Sampson, Hwang, Adamowski, Aguilar-Gaxiola, Al-Hamzawi, Andrade, Borges, de Girolamo, Florescu, Gureje, Haro, Hu, Karam, Lee, Navarro-Mateu, O’Neill, Pennell, Piazza, Posada-Villa, Have, Torres, Xavier, Zaslavsky and Kessler2017). In general, it leads to a chronic impairment, with 60–85% of children diagnosed with ADHD continuing to display symptoms into adolescence (Pliszka, Reference Pliszka2007), and between 2% and 46% (self- and parent-report, respectively) into adulthood (Barkley et al., Reference Barkley, Fischer, Smallish and Fletcher2002). A meta-analysis estimated the prevalence of ADHD in adulthood to be 2.5% (Simon et al., Reference Simon, Czobor, Bálint, Mészáros and Bitter2009), another meta-analysis involving more than 26 000 participants, estimated that 2.8% of adults met criteria for ADHD (Fayyad et al., Reference Fayyad, Sampson, Hwang, Adamowski, Aguilar-Gaxiola, Al-Hamzawi, Andrade, Borges, de Girolamo, Florescu, Gureje, Haro, Hu, Karam, Lee, Navarro-Mateu, O’Neill, Pennell, Piazza, Posada-Villa, Have, Torres, Xavier, Zaslavsky and Kessler2017). Only about one in six youths with ADHD still met full diagnostic criteria for ADHD at age 25, and about half showed signs of residual impairment according to another meta-analysis (Faraone et al., Reference Faraone, Biederman and Mick2006). A recent review has reported that adult ADHD is persistent in 2.58% of individuals who presented this disorder in childhood, whereas 6.76% of individuals present symptomatic adult ADHD regardless of childhood onset (Song et al., Reference Song, Zha, Yang, Zhang, Li and Rudan2021).
The prevalence of persistent adult ADHD (with a childhood onset) and symptomatic adult ADHD (regardless of a childhood onset) both decreased with advancing age. One systematic review focusing on the ADHD prevalence in adults older than 50 years identified only 4 studies and estimated that the prevalence ranged from 1.0% to 6.2% (Torgersen et al., Reference Torgersen, Gjervan, Lensing and Rasmussen2016). A large study carried out in India reported an adjusted prevalence of diagnosed ADHD of 0.22% or lower for persons aged 50 and older (Sagar et al., Reference Sagar, Dandona, Gururaj, Dhaliwal, Singh, Ferrari, Dua, Ganguli, Varghese, Chakma, Kumar, Shaji, Ambekar, Rangaswamy, Vijayakumar, Agarwal, Krishnankutty, Bhatia, Charlson, Chowdhary, Erskine, Glenn, Krish, Mantilla-Herrera, Mutreja, Odell, Pal, Sanjay, Damian, D K, Ravinder, Singh, Thakur, ThekkePurakkal, Varghese, Reddy, Swaminathan, Whiteford, Bekedam, Murray, Vos and Dandona2020). A meta-analysis found that the prevalence of ADHD in older adults differed according to the assessment methods: 2.18% (95% CI = 1.51%, 3.16%) based on diagnosis using validated scales, 0.23% (0.12%, 0.43%) based on clinical diagnosis, and 0.09% (0.06%, 0.15%) based on treatment rates (Dobrosavljevic et al., Reference Dobrosavljevic, Solares, Cortese, Andershed and Larsson2020).
ADHD etiology is not clearly established and many conditions may represent potential risk factors: genetic heritability, estimated at 76% (Faraone et al., Reference Faraone, Perlis, Doyle, Smoller, Goralnick, Holmgren and Sklar2005); neuroanatomical abnormalities with decreased volume of white and gray cortical matter (Sowell et al., Reference Sowell, Thompson, Welcome, Henkenius, Toga and Peterson2003); altered dopamine and serotonin pathway (Faraone et al., Reference Faraone, Perlis, Doyle, Smoller, Goralnick, Holmgren and Sklar2005); and neurophysiology dysfunction of fronto-striatal structures (Barry et al., Reference Barry, Clarke and Johnstone2003; Bush et al., Reference Bush, Valera and Seidman2005).
In pediatric age, ADHD diagnosis is essentially based on clinical observation and on information obtained from interviews with parents, teachers, and educators, since impairing symptoms must be present in more than one setting (American Psychiatric Association [APA], 2013). Semi-structured questionnaires or interviews were implemented for parents and teachers as were scales to measure the severity of the disorder and comorbid psychiatric symptoms. Similarly, neuropsychological tests are administrated to investigate the development of cognitive functioning. Unfortunately, no biological marker is available for diagnosis in either childhood or adulthood, although slow EEG rhythms (Jasper et al. Reference Jasper, Solomon and Bradley1938), and altered frontal–striatal–cerebellum dopaminergic pathway in neuroimaging have been suggested (Lenartowicz & Loo, Reference Lenartowicz and Loo2014). Due to this lack of biological markers, ADHD diagnosis can be influenced by cultural factors, as suggested by the differences in ADHD prevalence across the world (Sayal et al., Reference Sayal, Prasad, Daley, Ford and Coghill2018).
In the childhood population, ADHD is more frequent in males, with a ratio of 2:1 (American Psychiatric Association [APA], 2013; Sayal et al., Reference Sayal, Prasad, Daley, Ford and Coghill2018). Some authors highlighted a smaller difference between the two sexes, suggesting that inattentive ADHD dimension emerged the most prevalent, often undiagnosed, ADHD presentation and among females (Ramtekkar et al., Reference Ramtekkar, Reiersen, Todorov and Todd2010; Nussbaum, Reference Nussbaum2012).
ADHD impulse control and attention deficits foster the impairment of many social skills resulting in educational issues (school dropouts and/or failures, discipline problems, etc.) (Kuriyan et al., Reference Kuriyan, Pelham, Molina, Waschbusch, Gnagy, Sibley, Babinski, Walther, Cheong, Yu and Kent2013), antisocial behavior (Young et al., Reference Young, Gudjonsson, Chitsabesan, Colley, Farrag, Forrester, Hollingdale, Kim, Lewis, Maginn, Mason, Ryan, Smith, Woodhouse and Asherson2018), substance use (Gudjonsson et al., Reference Gudjonsson, Sigurdsson, Sigfusdottir and Young2012; Estevez et al., Reference Estevez, Dey, Eich-Hochli, Foster, Gmel and Mohler-Kuo2016; Zamboni et al., Reference Zamboni, Marchetti, Congiu, Giordano, Fusina, Carli, Centoni, Verlato and Lugoboni2021), incidents, unemployment, occupational and relational instability (Sayal et al., Reference Sayal, Prasad, Daley, Ford and Coghill2018). In childhood and adolescence, ADHD is often associated with other psychiatric disorders, such as oppositional defiant disorder, conduct disorder and depressive disorders (Powell et al., Reference Powell, Riglin, Hammerton, Eyre, Martin, Anney, Thapar and Rice2020), which can further impair the social adjustment, increasing the complexity of treatments (Erskine et al., Reference Erskine, Norman, Ferrari, Chan, Copeland, Whiteford and Scott2016). Moreover, individuals with ADHD present a higher mortality rate compared to the rest of the population, as highlighted by a nationwide cohort study and a recent systematic review (Dalsgaard et al., Reference Dalsgaard, Ostergaard, Leckman, Mortensen and Pedersen2015; Ruiz-Goikoetxea et al., Reference Ruiz-Goikoetxea, Cortese, Aznarez-Sanado, Magallón, Alvarez Zallo, Luis, Castro-Manglano, Soutullo and Arrondo2018).
The most widely used treatment in school age is represented by catecholaminergic stimulant medication, e.g., dopaminergic stimulation with methylphenidate and atomoxetine. In general, non-pharmacological treatments including parent training, psychoeducational support, and psychotherapies are often associated (Storebø et al., Reference Storebø, Ramstad, Krogh, Nilausen, Skoog, Holmskov, Rosendal, Growth, Magnusson, Moreira-Maia, Gillies, Rasmussen, Gauci, Zwi, Kirubakaran, Forsbøl, Simonsen and Gluud2015).
The choice of different treatments depends on the age of patients, because non-pharmacological treatments, such as parent training in behavior management techniques, are preferred in pre-school age or at the onset of ADHD, as recommended by most guidelines (Italian Society of Child And Adolescent Neuropsychiatry, 2002; National Institute for Health and Clinical Excellence [NICE], 2009; American Psychological Association [APA], 2012). If those interventions fail, methylphenidate may be considered only in case of moderate-to-severe symptoms as indicated by APA guidelines (American Psychological Association [APA], 2012). The Multimodal Treatment Study of Children with ADHD (MTA) and subsequently Swanson et al. (Reference Swanson, Kraemer, Hinshaw, Arnold, Conners, Abikoff, Clevenger, Davies, Elliott, Greenhill, Hechtman, Hoza, Jensen, March, Newcorn, Owens, Pelham, Schiller, Severe and Wu2001) analyzed the efficacy of stimulant therapies, highlighting that the success rate was only 56%, whereas behavioral treatments were even less effective (The MTA Cooperative Group [MTA], 1999). No consistent results concerning the efficacy of stimulant medication in preventing adulthood ADHD persistence and/or the occurrence of other comorbid psychiatric disorders were highlighted. The longer-term consequences of pharmacological treatments in childhood have been investigated by several studies and some systematic reviews, but without conclusive results (Shaw et al., Reference Shaw, Hodgkins, Caci, Young, Kahle, Woods and Arnold2012).
Recently, more attention has been drawn to the previously questioned persistence of ADHD in adulthood and more studies have been implemented to explore this issue. In particular, recent long-term studies on the evolution of ADHD onset in childhood and its consequences in adulthood have contributed to recognizing that ADHD can be a lifetime chronic disorder with a significant impairment of quality of life (Hodgkins et al., Reference Hodgkins, Arnold, Shaw, Caci, Kahle, Woods and Young2012). Therefore, early diagnosis and appropriate treatments of ADHD have become important targets to prevent long-term outcomes (National Institute for Health and Clinical Excellence [NICE], 2009). As a matter of fact, a recent study pointed out the importance of diagnosis among adults with ADHD: diagnosed patients experience better functioning, Health-Related Quality of Life (HRQoL), and self-esteem in comparison with symptomatic, but undiagnosed ADHD patients (Pawaskar et al., Reference Pawaskar, Fridman, Grebla and Madhoo2020).
The criteria for ADHD diagnosis can greatly affect the adult prevalence rate, since if the DSM-IV partial remission criteria are adopted, the rate of persistence in adulthood is much higher (Faraone et al., Reference Faraone, Perlis, Doyle, Smoller, Goralnick, Holmgren and Sklar2005). Another study (Biederman et al., Reference Biederman, Petty, Clarke, Lomedico and Faraone2011) pointed out that severe social impairment, psychiatric comorbidities, and exposure to maternal psychopathology at the onset of ADHD can be significant predictors for adult ADHD persistence. The World Mental Health Survey Initiative highlighted a rate of persistent ADHD in adulthood of 50% on average and identified many predictors of persistence: ADHD symptom severity and type of symptoms (attentional plus impulsive–hyperactive type), comorbid major depressive disorder, paternal (but not maternal) anxiety–mood disorder, and parental antisocial personality disorder (Lara et al., Reference Lara, Fayyad, de Graaf, Kessler, Aguilar-Gaxiola, Angermeyer, Demytteneare, de Girolamo, Haro, Jin, Karam, Lépine, Mora, Ormel, Posada-Villa and Sampson2009). Many adults with ADHD may be undiagnosed and untreated or, otherwise, many false positive cases can be incorrectly treated (Sibley et al., Reference Sibley, Mitchell and Becker2016). Other studies questioned that adult ADHD can represent a childhood-onset neurodevelopmental disorder. A recent study identified among the heterogeneous adult ADHD population a large group with late-onset ADHD without childhood diagnosis and with minimal neuropsychological impairment (Agnew-Blais et al., Reference Agnew-Blais, Polanczyk, Danese, Wertz, Moffitt and Arseneault2016). Another study did not confirm that adulthood ADHD is always a childhood ADHD persistence, suggesting the possibility that 2 syndromes with different developmental trajectories can be presented with similar symptom profile at different ages (Caye et al., Reference Caye, Rocha, Anselmi, Murray, Menezes, Barros, Gonçalves, Wehrmeister, Jensen, Steinhausen, Swanson, Kieling and Rohde2016).
Despite growing interest in adult ADHD, until now, its clinical course in adulthood has been evaluated by few studies. A prospective 33-year follow-up study of childhood ADHD observed that 22% of original cohort presented ongoing ADHD at mean age 41 (Klein et al., Reference Klein, Mannuzza, Olazagasti, Roizen, Hutchison, Lashua and Castellanos2012). The Massachusetts General Hospital Longitudinal Studies of ADHD reported that in both sexes, this disorder is associated with high levels of persistence into adulthood and documented its neural basis using neuroimaging (Uchida et al., Reference Uchida, Spencer, Faraone and Biederman2018).
Similarly, a 7-year follow-up study of adults with ADHD showed that approximately a third of the sample did not maintain ADHD criteria and 12.4% presented full remission (<4 symptoms) (Karam et al., Reference Karam, Breda, Picon, Rovaris, Victor, Salgado, Vitola, Silva, Guimarães-da-Silva, Mota, Caye, Belmonte-de-Abreu, Rohde, Grevet and Bau2015). During follow-up study, symptoms declined in all ADHD domains, but rises in inattentive, hyperactive, and impulsive symptoms were observed in approximately 13%, 25%, and 17% of patients, respectively (Karam et al., Reference Karam, Rovaris, Breda, Picon, Victor, Salgado, Vitola, Mota, Silva, Meller, Rohde, Grevet and Bau2017). Different predictors influenced ADHD dimensions: oppositional defiant disorder and social phobia were associated with the maintenance of symptoms, while alcohol use disorder was associated with both maintenance and rise of symptoms (Karam et al., Reference Karam, Rovaris, Breda, Picon, Victor, Salgado, Vitola, Mota, Silva, Meller, Rohde, Grevet and Bau2017).
Although the lifetime “instability in diagnosis” highlighted by some authors (Sibley et al., Reference Sibley, Mitchell and Becker2016), ADHD is currently interpreted as a chronic condition, which can be present in adulthood and can be associated with other disorders and/or social maladjustment.
This systematic review is aimed at highlighting the clinical and social consequences among adults who suffered from ADHD in their childhood/adolescence.
Methods
The review has been planned ahead and registered in the international database PROSPERO (registration number: CRD42020173960; published on April 28, 2020).
Research questions
-
– Is the childhood and adolescence ADHD clinically remitted in adulthood?
In adults who were diagnosed with ADHD in childhood and adolescence, what is the prevalence of the following conditions, independently of the presence of ADHD diagnoses in adulthood:
-
– social maladjustment (incarceration or legal problems)
-
– psychiatric disorders ascertained by clinical evaluation
-
– substance and/or alcohol use ascertained by clinical evaluation?
Study identification
We adopted the PRISMA (Moher et al., Reference Moher, Shamseer, Clarke, Ghersi, Liberati, Petticrew, Shekelle and Stewart2015) flow diagram to describe the sequence of steps (identification, screening, eligibility, and inclusion) for the collection and identification of eligible studies. Following the formulation of the research questions reported above, we selected the keywords, with which we interrogated the PubMed, PsycINFO, and Scopus electronic databases.
We restricted our electronic search to the last 5 years, and searched other studies reviewing references from previous systematic reviews on articles published before 2015 on the same topics, to highlight updated data.
Studies were identified by searching the titles and abstracts of the last 5 years for the following search string: ((“Attention Deficit Disorder with Hyperactivity“[Mesh] OR “attention deficit hyperactivity disorder”[title] OR ADHD[title]) AND (adult[mesh] OR adult[ti] OR child[mesh] OR child[ti] OR children[ti] OR adolescent[mesh] OR adolescent[ti] OR adolescence[ti]) AND therapy)) AND (follow-up studies[mesh] OR follow-up[title] OR outcome OR prognosis)).
The titles of studies published in the 5 years were retrieved by a primary reviewer using the search strategy to detect potentially eligible articles. To increase the period of study publication, we systematically screened previous review articles published before 2015 and focused on the same topics (Hodgkins et al., Reference Hodgkins, Arnold, Shaw, Caci, Kahle, Woods and Young2012; Shaw et al., Reference Shaw, Hodgkins, Caci, Young, Kahle, Woods and Arnold2012; Erskine et al., Reference Erskine, Norman, Ferrari, Chan, Copeland, Whiteford and Scott2016; Sibley et al., Reference Sibley, Mitchell and Becker2016).
Inclusion criteria: prospective studies, studies with patients with ADHD diagnosed in childhood/adolescence (between the age of 5 and 18) and followed-up to adulthood, studies in which the diagnosis of ADHD was carried out using clinical and/or scale assessments, published in English or Italian.
Exclusion criteria: studies including subjects diagnosed after the age of 18, or diagnosed in childhood/adolescence, but without any follow-up evaluation in adulthood, or without clinical and/or scale assessment of ADHD. Book chapters were also excluded.
Following, three reviewers independently screened the abstracts and discrepancies were resolved after collective discussion. After the title and abstract screening phase, full texts were assessed for eligibility by the three reviewers, and again, any disagreement was resolved through discussion with the help of another reviewer in case of conflict on the final decision. Finally, three reviewers independently extracted relevant data using a form, designed ad hoc for the purposes of this review, including the following information: authors, year of publication, study design, sample size, interventions, and results for each investigated outcome. In particular, for the quantitative analysis, data regarding the number of adult patients with ADHD persistence, psychiatric disorders, substance use, and social maladjustment were extracted to find out: 1) the percentage of adult individuals with ADHD persistence at the end of follow-up period and 2) the percentage of adult patients affected by a psychiatric disorder (schizophrenia and other psychoses, bipolar disorders), alcohol and/or substance abuse, and social maladjustment (number of patients incarcerated or with legal problems, unemployed, and/or with other social problems), after having suffered from ADHD in childhood and adolescence.
Risk of bias (quality) assessment
Two authors independently assessed the risk of bias of the included studies using the Newcastle–Ottawa Scale (NOS). Briefly, the NOS tool is based on a star system assessing three domains: the ‘selection’ of the study groups, the ‘comparability’ of the groups, and the ascertainment of either ‘outcome’ or ‘exposure’ of interest for cohort or case–control studies, respectively (Muka et al., Reference Muka, Glisic, Milic, Verhoog, Bohlius, Bramer, Chowdhury and Franco2020). A score of six or less stars indicates a high risk of bias, seven or eight stars indicates a moderate risk, while nine stars indicates a low risk of bias.
Statistical analysis
We calculated the weighted mean (WM) with corresponding 95% confidence interval (CI) of investigated outcomes, namely, percentage of ADHD persistence in adulthood, presence of psychiatric disorders, substance use disorders, and antisocial/criminal activities. We weighted the analysis using the population size of each study, considering the total population or a specific subgroup alternatively. When several studies were carried out on the same cohort reporting several outcomes at different time levels, the study with the longest follow-up period was considered for the analysis of a specific outcome. We used the Stata software (release 16.1 2021; Stata Corp. College Station, Texas) for all data analyses.
Results
Selected studies
In Fig. 1, results of study retrieval and identification are shown. We identified a total number of 1899 articles through online database search and 583 through backward citation and reference scanning of relevant studies and previous reviews.

Fig. 1. PRISMA flow-chart of study identification and selection.
After exclusion of 2268 records based on title and abstract and of 3 articles because of duplicate studies, 211 articles were deemed eligible. After full-text evaluation, 172 articles were excluded on the basis of three main excluding criteria: 70 due to non-prospective design, 71 due to sample age <18 years at follow-up, 24 due to different outcomes, and 7 due to more than one reason (Fig. 1). Finally, 39 articles were included in the qualitative analysis of overall studies, with 5 studies carried in the same cohort of a more recent study which was considered for the quantitative synthesis. After risk of bias quality assessment, seven articles considered of low quality were excluded, leaving 27 studies to be included in the quantitative analysis of high-quality studies.
Study designs and findings
Most of the studies included (28 of 39) were published after the year 2000, 5 of them in the last 5 years, whereas another four research papers were published many years ago (before 1990), as shown in Table 1. Most of the selected studies (74%) were conducted in the USA, whereas only 26% of them were carried out in Canada (Hechtman et al., Reference Hechtman, Weiss and Perlman1984; Hechtman & Weiss, Reference Hechtman and Weiss1986; Greenfield et al., Reference Greenfield, Hechtman and Weiss1988), Denmark (Mohr-Jensen et al., Reference Mohr-Jensen, Müller Bisgaard, Boldsen and Steinhausen2019), Germany (Döpfner et al., Reference Döpfner, Ise, Breuer, Rademacher, Metternich-Kaizman and Schürmann2016), The Netherlands (van Lieshout et al., Reference van Lieshout, Luman, Twisk, van Ewijk, Groenman, Thissen, Faraone, Heslenfeld, Hartman, Hoekstra, Franke, Buitelaar, Rommelse and Oosterlaan2016), New Zealand (Fergusson et al., Reference Fergusson, Horwood and Ridder2007; Moffitt et al., Reference Moffitt, Houts, Asherson, Belsky, Corcoran, Hammerle, Harrington, Hogan, Meier, Polanczyk, Poulton, Ramrakha, Sugden, Williams, Rohde and Caspi2015), Sweden (Rasmussen & Gillberg, Reference Rasmussen and Gillberg2000), and Taiwan (Shyu et al., Reference Shyu, Yuan, Lee, Yang, Yang, Lee and Wang2015). The majority of included studies had a prospective cohort design, with only two that were case–control studies (De Sanctis et al., Reference De Sanctis, Newcorn and Halperin2014; Döpfner et al., Reference Döpfner, Ise, Breuer, Rademacher, Metternich-Kaizman and Schürmann2016). The follow-up of selected studies ranges between 5 and 33 years (mean = 14.88 ± 6.72 SD years).
Table 1. Characteristics of included studies
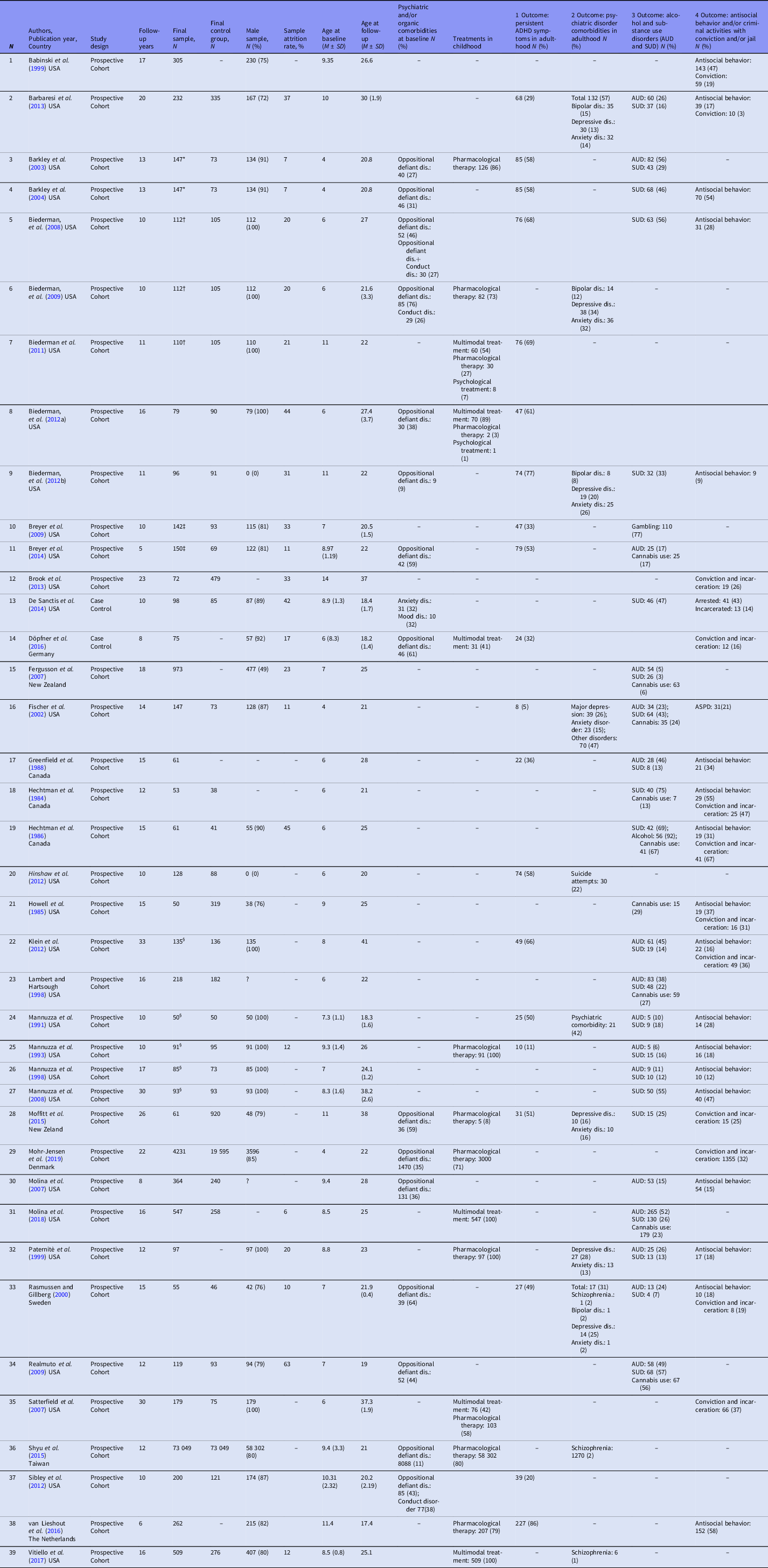
Notes: M, mean; N, number; SD, standard deviation, *same sample, †the Massachusetts General Hospital Sample, ‡same sample, §the New York Sample.
The samples collected by our studies were composed of more than 80 000 individuals, ranging between 50 and 73 049. The attrition rate, which was reported by only 22 studies, ranged between 6% (Molina et al., Reference Molina, Howard, Swanson, Stehli, Mitchell, Kennedy, Epstein, Arnold, Hechtman, Vitiello and Hoza2018) and 63% (Realmuto et al., Reference Realmuto, Winters, August, Lee, Fahnhorst and Botzet2009). Only six studies (15%) did not collect a control group to compare the variables of the sample.
The average age at baseline ranged between 4 and 14 years (mean = 7.11 ± 2.5 SD years), whereas the age at follow-up was between 19 and 41 years (mean = 25.65 ± 5.9 SD years). One study (Biederman et al., Reference Biederman, Petty, O’Connor, Hyder and Faraone2012b) recruited a sample of females only, whereas 11 studies collected samples of males only (Mannuzza et al., Reference Mannuzza, Klein and Addalli1991; Mannuzza et al., Reference Mannuzza, Klein, Bessler, Malloy and La Padula1993; Mannuzza et al., Reference Mannuzza, Klein, Bessler, Malloy and La Padula1998; Paternitè et al., Reference Paternitè, Loney, Salisbury and Whaley1999; Satterfield et al., Reference Satterfield, Faller, Crinella, Schell, Swanson and Homer2007; Biederman et al., Reference Biederman, Petty, Dolan, Hughes, Mick, Monuteaux and Faraone2008; Mannuzza et al., Reference Mannuzza, Klein and Moulton2008; Biederman et al., Reference Biederman, Monuteaux, Spencer, Wilens and Faraone2009; Biederman et al., Reference Biederman, Petty, Clarke, Lomedico and Faraone2011; Klein et al., Reference Klein, Mannuzza, Olazagasti, Roizen, Hutchison, Lashua and Castellanos2012; Biederman et al., Reference Biederman, Petty, Woodworth, Lomedico, Hyder and Faraone2012a). The remaining study samples were mainly composed of males with a proportion ranged between 49% and 91%.
As shown in Table 1, 15 studies (38%) reported psychiatric disorders in comorbidity at baseline age, mainly represented by Oppositional Defiant Disorder (ODD), with a proportion range of 9–81%, followed by Conduct Disorders (CD), which was reported in three studies associated with ODD, with a range between 26 and 38.3%. Only one study reported anxiety disorders (32%) and mood disorders (32%) in comorbidity with ADHD at baseline age (De Sanctis et al., Reference De Sanctis, Newcorn and Halperin2014). Fourteen studies reported data on ADHD treatments in childhood, in particular pharmacological therapies with stimulants (eight studies: Mannuzza et al., Reference Mannuzza, Klein, Bessler, Malloy and La Padula1993; Paternitè et al., Reference Paternitè, Loney, Salisbury and Whaley1999; Barkley et al., Reference Barkley, Fischer, Smallish and Fletcher2003; Biederman et al., Reference Biederman, Monuteaux, Spencer, Wilens and Faraone2009; Moffitt et al., Reference Moffitt, Houts, Asherson, Belsky, Corcoran, Hammerle, Harrington, Hogan, Meier, Polanczyk, Poulton, Ramrakha, Sugden, Williams, Rohde and Caspi2015; Shyu et al., Reference Shyu, Yuan, Lee, Yang, Yang, Lee and Wang2015; van Lieshout et al. Reference van Lieshout, Luman, Twisk, van Ewijk, Groenman, Thissen, Faraone, Heslenfeld, Hartman, Hoekstra, Franke, Buitelaar, Rommelse and Oosterlaan2016; Mohr-Jensen et al., Reference Mohr-Jensen, Müller Bisgaard, Boldsen and Steinhausen2019) and multimodal treatments (three studies: Döpfner et al., Reference Döpfner, Ise, Breuer, Rademacher, Metternich-Kaizman and Schürmann2016; Vitiello et al., Reference Vitiello, Perez Algorta, Arnold, Howard, Stehli and Molina2017; Molina et al., Reference Molina, Howard, Swanson, Stehli, Mitchell, Kennedy, Epstein, Arnold, Hechtman, Vitiello and Hoza2018), or both therapies (three studies: Satterfield et al., Reference Satterfield, Faller, Crinella, Schell, Swanson and Homer2007; Biederman et al., Reference Biederman, Petty, Clarke, Lomedico and Faraone2011; Biederman et al., Reference Biederman, Petty, Woodworth, Lomedico, Hyder and Faraone2012a).
Twenty studies reported data on ADHD persistence with a proportion ranging between 5% and 85%. Among psychiatric disorders reported by 11 studies at the follow-up, depressive and anxiety disorders were the most frequently investigated (N = 7), followed by bipolar disorders (N = 4), and schizophrenia spectrum disorders (N = 3). In general, substance use disorders were reported in 21 studies, in particular alcohol (N = 16) and cannabis use (N = 9). Only one study reported gambling with a frequency of 77%. Finally, 18 studies reported antisocial personality disorders and antisocial behavior with prevalence ranging from 9% to 85%; 15 studies reported a prevalence of criminal activities ranging between 3% and 67%.
Quality assessment of included studies
The quality of most studies included in the review was assessed as good with a median score of 8, in accordance with the score system of NOS (Table S2). In particular, 26 studies obtained a score of 8 or 9 at NOS (high quality), 10 studies a score of 6 or 7 (moderate quality), and only 3 studies a score of 4 or 5 (low quality). Regarding the “selection” domain, 29 studies (74%) obtained the maximum score of 4, 5 studies (13%) a score of 3, and only 5 studies (13%) a score of 2. As regards the “comparability” domain, 6 studies (15%) did not present a comparison group, and for this reason, they obtained a 0 score; 26 studies (67%) reported the maximum score (2/2), whereas 7 studies (18%) only a score of 1. For the third domain (“outcome” for cohort studies and “exposure” for case–control studies), 26 studies (67%) obtained the maximum score of 3, whereas 13 studies (33%) scored 2.
Study outcome analysis
The persistence of ADHD diagnosis in adulthood was reported by 14 studies among the 39 included in this review (Fig. 2), with the percentage ranged from 4% to 86% and a weighted mean of 49% (95% CI 33–64%) in overall studies, and 43% (95% CI 28–58%) in the 12 high-quality studies. The prevalence of persistent ADHD in adulthood reported by the most recent studies published after 2011 (the median of study publication years) was higher than that reported by the other studies published previously from 1985 to 2011: 55% (95% CI 35–76%) vs. 34% (95% CI 6–62%), respectively (Fig. 3).
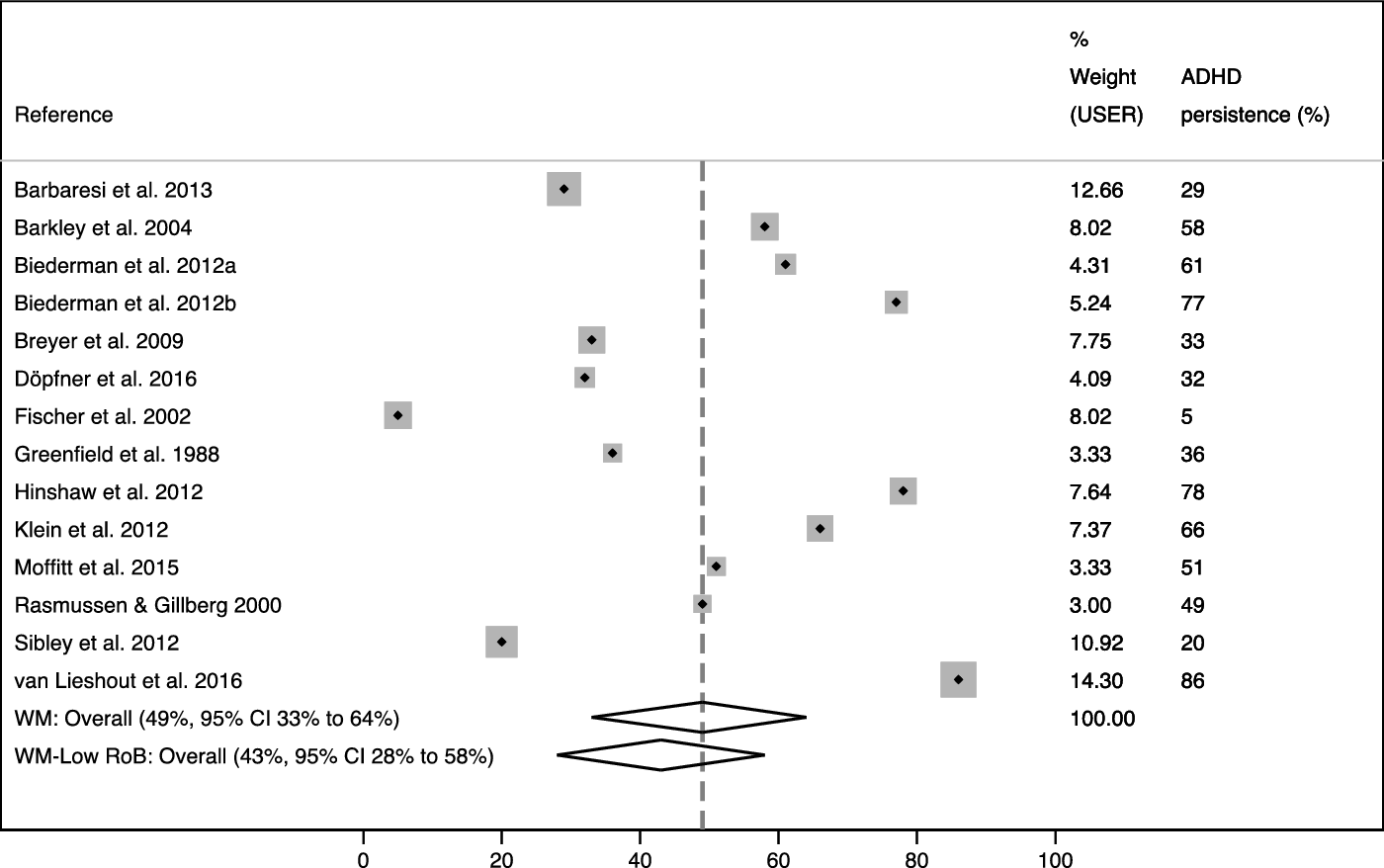
Fig. 2. Summary weight mean (WM) of ADHD persistence in adulthood (%) in overall studies and in high-quality studies.

Fig. 3. Summary weight mean (WM) of ADHD persistence in adulthood (%) in overall studies and in high-quality studies, divided by publication year (from 1985 to 2011 and after 2011).
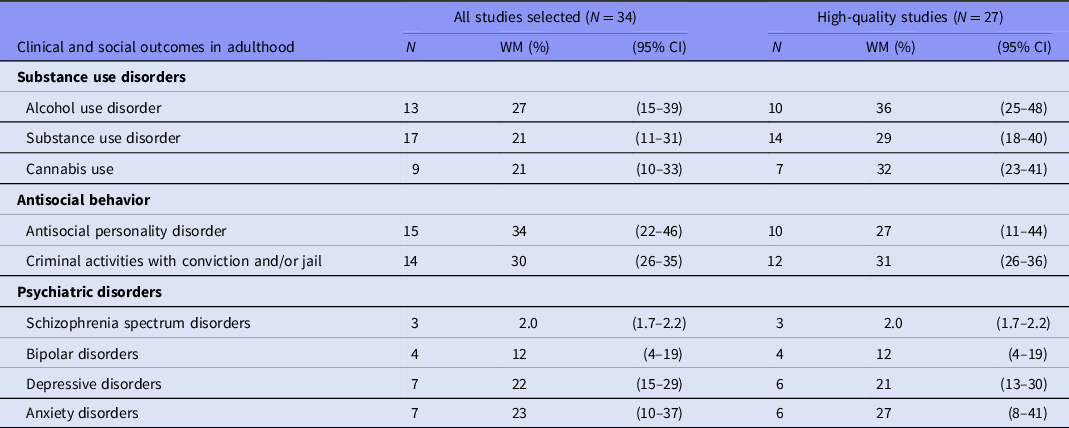
As reported in Table 2 and Supplemental Figures S1–S3, in the ADHD follow-up on adulthood, the most experienced condition was substance/alcohol use disorder, followed by antisocial personality disorder or criminal activities. Substance use disorder from 17 studies (21%, 95% CI 11–31%—Figure S1) and antisocial personality disorder from 15 studies (34%, 95% CI 22–46%—Figure S2). Focusing only on high-quality studies, substance/alcohol use disorder and antisocial personality or criminal activities were the most represented conditions: alcohol use disorder presented the highest percentage (36%, 95% CI 25–48% vs. 27%, 95% CI 15–39% on overall), followed by cannabis use (32%, 95% CI 23–41% vs. 21%, 95% CI 10–33% on overall) and criminal activities (32%, 95% CI 26–36% vs. 30%, 95% CI 26–35% on overall). Among the other psychiatric disorders associated with ADHD in adulthood, as shown in Figure S3, anxiety (23%, 95% CI 10–37%) and depressive (22%, 95% CI 15–29%) disorders were more frequently reported in comorbidity than bipolar disorders (12%, 95% CI 4–19%) and schizophrenia (2.0%, 95% CI 1.7–2.2%).
Table 2. Summary weighted mean (WM) and 95% confidence interval (CI) for secondary outcomes: substance use disorders, antisocial behavior, and psychiatric disorders
Discussion
This review was aimed at evaluating the follow-up of ADHD from childhood to adulthood to investigate the adult persistence of this disorder, the occurrence of psychiatric/substance use comorbidities, and antisocial consequences. In the literature, reports on ADHD persistence in adulthood are controversial and not exhaustive, probably due to the lack of clinical markers for diagnosing this disorder in both children and adults, which could condition the accuracy of diagnosis and the possibility of appropriate treatments. Similarly, the observations concerning the psychiatric comorbidities, which can be associated with ADHD in adulthood, are partial and not comprehensive. Only substance use disorders and antisocial behavior, which in extreme but frequent cases are represented by conviction and jail restriction, have been more extensively reported in the literature as ADHD long-term consequences in adulthood.
The studies included in this review report clinical observations during a long period of time, namely, 35 years, since they were published from 1984 to 2019, allowing us to collect an exhaustive framework of ADHD evolution in terms of diagnosis and treatments.
The majority of selected studies were conducted in the USA, 12 studies in other Western countries and only one among Asian population (Shyu et al., Reference Shyu, Yuan, Lee, Yang, Yang, Lee and Wang2015), indicating the careful attention paid to this disorder and its complications by the researchers and clinicians of these countries (Hodgkins et al., Reference Hodgkins, Arnold, Shaw, Caci, Kahle, Woods and Young2012). The country distribution of studies may represent a limitation, because all but one study investigated ADHD and its evolution mostly among Caucasians, thus restricting findings to a population with similar biological and cultural characteristics.
Most selected studies (37 out of 39) implemented a prospective cohort design that allowed an appropriate period of follow-up for the analysis of ADHD persistence. In addition, the number of people collected from the selected studies was large and representative of the general population. Indeed, all but one sample (Biederman et al., Reference Biederman, Petty, O’Connor, Hyder and Faraone2012b), which was composed exclusively of females, were mostly males (from 76% to 100% of samples), reflecting the higher prevalence of this disorder among this latter category in the general population. However, this feature, which reflects epidemiological data, may limit the generalizability of the study results, since many women with ADHD may be undiagnosed and unassessed (Ramtekkar et al., Reference Ramtekkar, Reiersen, Todorov and Todd2010).
The period of follow-up in selected studies was appropriate and sufficiently long to highlight the evolution of ADHD in early adulthood. In fact, the baseline age of people collected by most studies permits us to observe the ADHD onset and follow-up age to verify its evolution and comorbidity presence at early adult age, in accordance with the literature (American Psychiatric Association [APA], 2013; Sayal et al., Reference Sayal, Prasad, Daley, Ford and Coghill2018).
Some studies reported a maximum attrition rate of 45%, probably due to the long period of follow-up, representing a potential bias. Nevertheless, the sample retention gradually increased in the most recent studies compared to the earlier ones, suggesting an increase in both accuracy of studies and interest of participants. This observation seems further confirmed by the higher ADHD persistence in adulthood yielded in the stratified analysis on the most recent studies only.
Regarding the persistence of ADHD in adulthood, our studies reported a wide range of prevalence, in line with another recent review (Sibley et al., Reference Sibley, Mitchell and Becker2016), indicating the difficulties in ADHD diagnosis, especially in adulthood. In fact, the accuracy of ADHD data collection depends on the criteria used in the diagnosis of this disorder, which greatly differed: in some studies, diagnosis was evaluated through patients’ self-assessment or through specific scales or questionnaires, in others, ADHD symptoms were diagnosed through parent interviews or teacher assessments, and in others, only objective data, such as scholastic failure, incidents or legal conviction, were requested for evaluating ADHD outcomes. Moreover, during the period from 1985 to 2019, when studies included in our analysis were published, the ADHD diagnosis criteria underwent major changes, specifically in the definition of hyperkinetic disorder in ICD-9-CM (1978) or ICD-10 (1992) versus ADHD in DSM-III (American Psychiatric Association, 1980), DSM-III-R (American Psychiatric Association [APA], 1987), and DSM-IV (American Psychiatric Association [APA], 1994), which can have greatly influenced the accuracy and stability of ADHD diagnosis over time. Moreover, as recently highlighted by a review, self-reports and/or strict diagnostic criteria threshold as required by DSM-5 can lead to a very low persistence rate in adulthood (Sibley et al., Reference Sibley, Mitchell and Becker2016). Therefore, authors recommended multilevel diagnosis criteria for adult ADHD, including self-assessment ratings and parents/educators/others interviews, impaired social adjustment, and appropriate diagnosis criteria for adulthood (Sibley et al., Reference Sibley, Mitchell and Becker2016). The weighted average of 43% reported by this review as the mean incidence of persistent ADHD in adulthood overlaps that of the epidemiological literature (American Psychiatric Association [APA], 2013; Sayal et al., Reference Sayal, Prasad, Daley, Ford and Coghill2018), indicating that persistence of this disorder in adulthood affects approximately half of children with ADHD. In accordance with our results, higher prevalence of persistent ADHD was observed in the studies published after 2011 in comparison with those published before, suggesting increased attention drawn to this disorder and/or more accurate diagnosis criteria applied during the past 10 years (Sibley et al., Reference Sibley, Mitchell and Becker2016).
The majority of studies reported that oppositional defiant and conduct disorders were the more frequently associated comorbidities with ADHD in childhood. These data, in line with epidemiological findings (Erskine et al., Reference Erskine, Norman, Ferrari, Chan, Copeland, Whiteford and Scott2016), suggest the close and frequent association between ADHD and disorders characterised by externalizing symptoms and aggressive behavior. The high prevalence of these disorders in childhood is consistent with an equally high prevalence of antisocial behavior and/or criminality activities observed in adult ADHD, confirming that antisocial personality disorder and criminal activities can be the evolution of childhood oppositional and impulsive behavior, in accordance with the literature (Kessler et al., Reference Kessler, Nelson, McGonagle, Edlund, Frank and Leaf1996). Unfortunately, only one study among the selected ones (Molina et al., Reference Molina, Pelham, Gnagy, Thompson and Marshal2007) carried out stratified analysis according to ADHD comorbidity with ODD and/or CD in childhood, reporting higher prevalence of antisocial personality disorders in the latter category.
Differently, other psychiatric disorders were less frequently associated with ADHD in adulthood, especially schizophrenia, whose prevalence ranged between 1% and 2%, slightly higher than that of the general population (American Psychiatric Association [APA], 2013). This result can help us to differentiate ADHD from schizophrenia due to different biological substrates and clinical patterns. Moreover, the meta-analysis of Shyu et al. (Reference Shyu, Yuan, Lee, Yang, Yang, Lee and Wang2015) highlighted that methylphenidate use in ADHD did not increase the specific risk of developing schizophrenia.
In our selected studies, bipolar disorders associated with adult ADHD presented a prevalence of 2–15%, rates substantially greater than the general population. This result confirms the epidemiological observation that ADHD in adulthood is frequently associated with bipolar disorders with a maximum rate of 21% (Kessler et al., Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Ustun, Walters and Zaslavsky2006; Di Nicola et al., Reference Di Nicola, Sala, Romo, Catalano, Even, Dubertret, Martinotti, Camardese, Mazza, Tedeschi, Callea, De Risio, Guelfi, Rouillon, Janiri and Gorwood2014). This association can worsen both the disorders with an increase of affective episodes and suicide attempts (Sachs et al., Reference Sachs, Baldassano, Truman and Guille2000; Nierenberg, et al., Reference Nierenberg, Miyahara, Spencer, Wisniewski, Otto, Simon, Pollack, Ostacher, Yan, Siegel and Sachs2005). The association between bipolar disorders and attention-deficit/hyperactivity disorder (ADHD) in children and adolescents has been previously much debated due to the similarity of symptoms, age of onset, comorbidities, and chronic lifelong course, which makes the differential diagnosis and the treatment complicated (Marangoni et al., Reference Marangoni, De Chiara and Faedda2015). Moreover, due to these similarities, a potential common biological vulnerability shared by these two disorders has been hypothesised, but not confirmed to date (Marangoni et al., Reference Marangoni, De Chiara and Faedda2015).
Most selected studies reported that anxiety and depressive disorders were frequently reported as comorbid disorders in the adult ADHD, with a higher prevalence than the general population. The real incidence of these disorders, which has been generally underestimated over previous years in younger subjects, especially in case of mild or subthreshold symptoms (Wittchen et al., Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson, Jönsson, Olesen, Allgulander, Alonso, Faravelli, Fratiglioni, Jennum, Lieb, Maercker, van Os, Preisig, Salvador-Carulla, Simon and Steinhausen2011), could indicate that both disorders can represent psychological reactions to the relational and social difficulties induced by ADHD. The high prevalence of depressive disorders highlighted by this review is in line with that reported (38%) by a national comorbid ADHD survey (Kessler et al., Reference Kessler, Adler, Barkley, Biederman, Conners, Demler, Faraone, Greenhill, Howes, Secnik, Spencer, Ustun, Walters and Zaslavsky2006). The frequent relation between mood disorders and ADHD is also highlighted by the high prevalence (5–12%) of co-occurring ADHD and major depressive disorder in adults (McIntyre et al., Reference McIntyre, Kennedy, Soczynska, Nguyen, Bilkey, Woldeyohannes, Nathanson, Joshi, Chenq, Benson and Muzina2010; Bond et al., Reference Bond, Hadjipavlou, Lam, McIntyre, Beaulieu, Schaffer and Weiss2012; Di Nicola et al., Reference Di Nicola, Sala, Romo, Catalano, Even, Dubertret, Martinotti, Camardese, Mazza, Tedeschi, Callea, De Risio, Guelfi, Rouillon, Janiri and Gorwood2014). Depressive disorders associated with ADHD can be more severe, with greater functional impairment and higher rates of suicidality (Chronis-Tuscano et al., Reference Chronis-Tuscano, Molina, Pelham, Applegate, Dahlke, Overmyer and Lahey2010). In this regard, among our selected studies, only one (Hinshaw et al., Reference Hinshaw, Owens, Zalecki, Huggins, Montenegro-Nevado, Schrodek and Swanson2012) reported that suicide attempts in ADHD had a frequency of 22%. This finding is consistent with the recent observation of an increased risk for suicide in ADHD, especially in males, probably due to the worsening of comorbid conditions, in particular conduct disorder and depression (Balazs & Kereszteny, Reference Balazs and Kereszteny2017).
Another frequent complication of ADHD was represented by substance/alcohol use disorders, in particular alcohol and cannabis. Only one more recent study observed gambling as a frequent complication in adult ADHD, probably because this condition is currently more observed and diagnosed. This observation is in line with other recent studies: among adult patients with substance use, about one-fifth have ADHD, which further worsens the clinical course of addiction disorder (Wilens, Reference Wilens2007); 23% of patients with substance use disorder met DSM criteria for comorbid ADHD (van Emmerik-van Oortmerssen et al., Reference van Emmerik-van Oortmerssen, van de Glind, van den Brink, Smit, Crunelle, Swets and Schoevers2012).
In accordance with our results, alcohol and cannabis use disorders are the most frequent complications of adult persistent ADHD. A recent study estimated that the prevalence of ADHD in adults seeking treatment for cannabis use disorders ranged from 34% to 46% (Notzon et al., Reference Notzon, Pavlicova, Glass, Mariani, Mahony, Brooks and Levin2020). Another 25-year prospective longitudinal study (Fergusson & Boden, Reference Fergusson and Boden2008) in a birth cohort of 1265 New Zealand children reported that cannabis use by age 25 was significantly associated with increasing self-reported ADHD symptoms, which could support the hypothesis of common neurological dopaminergic paths (Castelli et al., Reference Castelli, Federici, Rossi, De Chiara, Napolitano, Studer, Motta, Sacchetti, Romano, Musella, Bernardi, Siracusano, Gu, Mercuri, Usiello and Centonze2011). Regarding alcohol use disorder, a review highlighted that both ADHD and alcohol use disorder can be associated with neuropsychological impairments in diverse domains, including executive functioning and working memory (Grazioli et al., Reference Grazioli, Gmel, Rougemont-Bücking, Baggio, Daeppen and Studer2019). This association may also favor the detrimental course of ADHD associated with alcohol use disorder.
Moreover, the high prevalence of substance and alcohol use disorders is similar to the high prevalence of antisocial behavior and personality disorders, confirming data from the literature regarding the frequent association of both conditions which can make each other worse (Mueser et al., Reference Mueser, Crocker, Frisman, Drake, Covell and Essock2006; Philipp-Wiegmann et al., Reference Philipp-Wiegmann, Rosler, Clasen, Zinnow, Retz-Junginger and Retz2018).
Our selected studies reported data concerning treatments prescribed in childhood and, in particular, their long-term efficacy in improving symptoms and in preventing complications of ADHD in adulthood. In this regard, a recent systematic review investigated the long-term efficacy of pharmacological treatments in reducing the impairment of quality of life (Shaw et al., Reference Shaw, Hodgkins, Caci, Young, Kahle, Woods and Arnold2012), highlighting that treatments improve the ADHD outcomes, reducing its negative impact on relational and social functioning in comparison with untreated ADHD but not with normal control groups. In any case, the real efficacy of therapy is difficult to evaluate due to the lack of clinical randomised studies, although a recent review and meta-analysis has highlighted that early diagnosis and treatment of ADHD may help alleviate the risk of harmful outcomes (Boland et al., Reference Boland, DiSalvo, Fried, Woodworth, Wilens, Faraone and Biederman2020).
This systematic review has a number of limitations. First of all is, as reported above, the instability of ADHD diagnosis over time, much increased by cultural changes and scientific measures over a period of 35 years. Moreover, the lack of many data regarding specific categories of population and outcomes limited the implementation of further stratified analyses. In addition, all but one of the selected studies was carried out in Western countries, further limiting the observation of population variability. On the other hand, the length of study follow-up allows us to assess the long-term consequences of ADHD in early adulthood, observing the most frequent and relevant outcomes of this disorder. The good quality of studies favored the accuracy of the review. Moreover, the long period of time in which the studies were published allowed us to appreciate the evolution over time of ADHD diagnosis and treatments, which reflect the concomitant cultural and social evolution.
Limitations
Some limitations affecting the present study need to be acknowledged. First, the adopted criteria were not completely standardised. In particular, we restricted our search to the last 5 years, and searched previous studies reviewing references from comprehensive systematic reviews of studies published before the last 5 years. Although we may have missed some papers published before our chosen time frame, a noticeable amount of studies has been included in this review, confirming the growing interest in this topic during the last 5 years which has led us to new insight in this disorder.
Conclusions
This review has contributed to highlighting the long-term consequences of childhood-onset ADHD, confirming that this disorder can persist into adulthood with a mean rate of 40% and can be mainly associated with both substance/alcohol use disorders and antisocial behavior and, less frequently, with anxiety and depressive disorders. Our results highlight the difficulty in evaluating adult ADHD, since the wide range of persistence observed in the selected study. This diagnosis showed an increased accuracy over time in the most recent studies, suggesting more interest and attention in this disorder, which should be not just considered a neurodevelopmental disorder but a chronic and complex condition, which can predispose the development of other psychiatric disorders or social maladjustment with detrimental consequences for quality of life in adulthood.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/neu.2021.23
Author contribution
RDL conceptualized the study and with the contribution of JB, CP, EA, AC and TF collected data and draft the tables and the first draft. TF performed statistical analysis. PF and RDA contributed to the review and revision of the manuscript. All authors read and approved the final version of the manuscript.
Financial support
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflicts of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.








